Navigating the Minefield: Your Guide to Gout-Friendly Eating
Introduction: Stepping into the Minefield
Imagine this: one moment, you’re enjoying life, perhaps a celebratory meal, perhaps just a regular Tuesday. The next, a searing, unrelenting pain erupts in your big toe, ankle, or knee. It’s not a sprain, not a break, but a ferocious, fiery agony that makes even the lightest touch unbearable. This, my friend, is gout – a condition often misunderstood, frequently dismissed, but undeniably debilitating. It’s a chronic metabolic disorder, a relentless adversary driven by an excess of uric acid crystallizing in your joints, turning them into battlegrounds of inflammation.
For those who live with it, gout isn’t just a fleeting inconvenience; it’s a constant, insidious threat. Every meal can feel like a gamble, every culinary choice a potential trigger. You stand at the edge of a vast, unseen minefield, where delicious temptations lurk as hidden explosives, ready to detonate a flare-up. The confusion is immense: what’s safe? What’s a definite no-go? How do you enjoy food again without fear?
This isn’t just a dietary guide; it’s an expedition. We’re going to equip you with a map, a compass, and the knowledge to navigate this culinary minefield with confidence. Our journey together will transform uncertainty into empowerment, fear into understanding. We’ll delve into the science, demystify the myths, and chart a course toward a gout-friendly eating strategy that doesn’t just manage symptoms, but reclaims the joy of food and, ultimately, the quality of your life. For the knowledgeable individual seeking control, this is your comprehensive story of how to disarm the dietary triggers and build a resilient, gout-resistant lifestyle.
Part 1: Understanding the Terrain – The Science Behind the Bites
Before we can navigate the minefield, we must understand its topography, its hidden mechanisms. Gout, at its core, is a disorder of purine metabolism. Purines are natural compounds found in all our body’s cells and in almost all foods. When purines break down, they produce uric acid. Normally, our kidneys filter uric acid out of the blood and excrete it through urine. But for someone with gout, this delicate balance is disrupted.
The Uric Acid Overload:
Hyperuricemia, the medical term for high levels of uric acid in the blood, is the precursor to gout. This can happen for two primary reasons, or often a combination of both:
- Overproduction: Your body produces too much uric acid from the breakdown of purines, either from its own cells (endogenous purines) or from the foods you eat (exogenous purines).
- Under-excretion: Your kidneys don’t efficiently remove enough uric acid from your body. This is the more common reason.
When uric acid levels consistently remain high, it begins to crystallize, forming sharp, needle-like urate crystals, most commonly in cooler areas of the body like the big toe joint. These crystals then trigger an intense inflammatory response, leading to the excruciating pain, swelling, redness, and warmth characteristic of a gout attack.
Beyond Purines: The Nuanced Triggers:
While purines are the prime suspects, the story is far more complex. Our knowledgeable audience understands that biology rarely offers simple, one-dimensional answers. Other dietary factors play crucial roles in influencing uric acid levels and inflammatory responses:
- Fructose: This simple sugar, especially in its processed form (high-fructose corn syrup) and in sugary drinks, is a potent trigger. Fructose is metabolized in a way that directly increases uric acid production and can hinder its excretion by the kidneys. It’s a silent, insidious threat, often hidden in seemingly innocuous foods.
- Alcohol: Beer, in particular, is a notorious culprit due to its high purine content (from yeast) and its ability to both increase uric acid production and reduce its excretion. Spirits can also be problematic, though perhaps less so than beer. Wine, surprisingly, has been shown to have a less pronounced effect for some individuals, but moderation remains key across all alcohol types.
- Dehydration: Adequate hydration is vital for kidney function. Insufficient water intake can concentrate uric acid in the blood, making crystallization more likely.
- Obesity: Excess body weight is strongly linked to hyperuricemia and gout. Adipose tissue (fat) is metabolically active and can contribute to chronic inflammation and altered uric acid metabolism. Weight loss, however, must be gradual, as rapid weight loss or crash diets can paradoxically trigger attacks due to increased purine breakdown.
- Insulin Resistance & Metabolic Syndrome: These conditions, often associated with obesity, diabetes, and heart disease, are deeply intertwined with gout. Insulin resistance can impair the kidneys’ ability to excrete uric acid effectively.
Understanding these interconnected factors is like having an advanced reconnaissance report on the minefield. It reveals that gout-friendly eating isn’t just about avoiding purines; it’s about a holistic approach to metabolic health and inflammation.
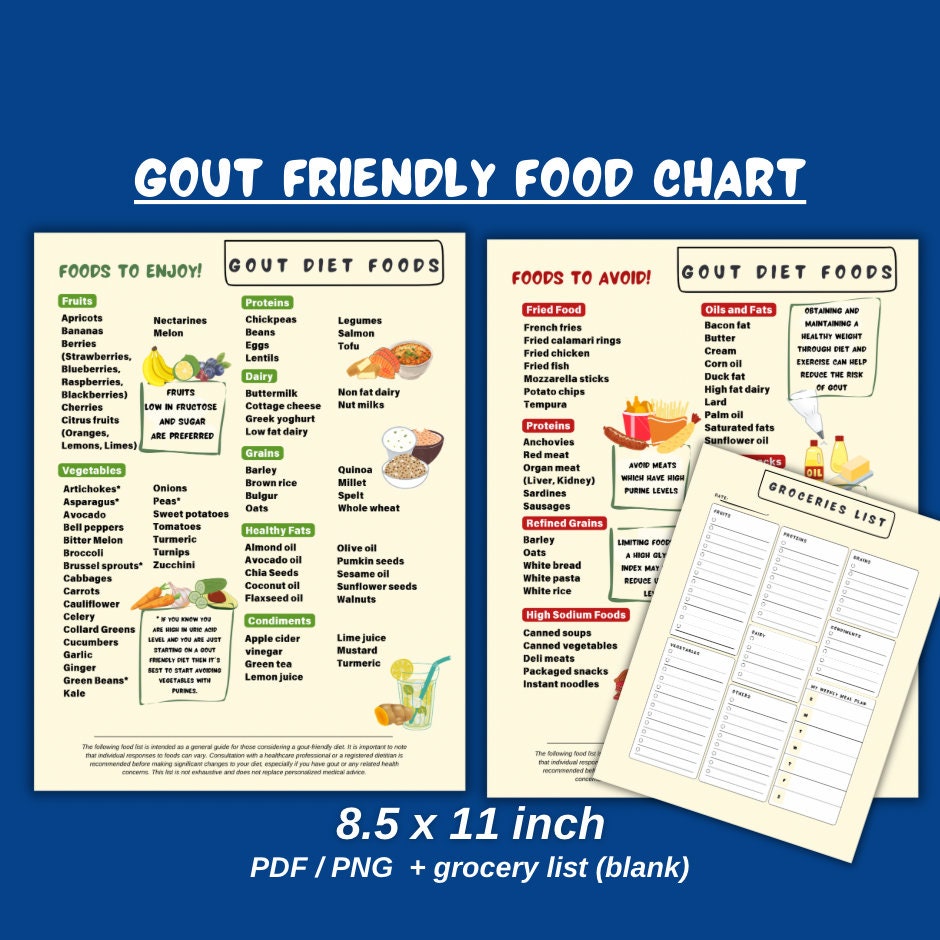
Part 2: The Minefield Map – Foods to Approach with Caution (or Avoid)
Now that we understand the science, let’s plot the dangers on our map. This section details the specific dietary components that act as the most common "mines," capable of detonating a painful flare-up.
High-Purine Offenders: The Obvious Explosives
These foods are generally high in purines (over 200 mg per 100 grams) and should be consumed sparingly, if at all, especially during a flare-up or if your uric acid levels are poorly controlled.
- Organ Meats: Liver, kidney, sweetbreads, brain. These are the absolute top-tier purine bombs. They are packed with the genetic material that produces uric acid upon breakdown. Think of them as high-yield explosives.
- Certain Seafood: Anchovies, sardines, herring, mackerel, scallops, mussels, codfish. While fish is generally healthy, these specific varieties are exceptionally high in purines. A small portion might be tolerated by some, but for others, they are definite triggers.
- Red Meats (in large quantities): Beef, lamb, pork, venison. While not as concentrated as organ meats, large, frequent servings of red meat can contribute significantly to purine load. The risk isn’t just in the purine content but also in the overall saturated fat intake often associated with these meats, which can indirectly exacerbate inflammation.
- Game Meats: Duck, goose. Similar to red meats, these can be quite purine-dense.
- Yeast and Yeast Extracts: Brewer’s yeast, nutritional yeast, Marmite/Vegemite. These products are concentrated sources of purines. Beer, as mentioned, is problematic due to its yeast content.
Fructose-Rich Detonators: The Hidden Threats
These are often more insidious because they don’t immediately scream "gout trigger." Their impact is metabolic, not directly purine-related, but no less potent.
- Sugary Drinks: Soda, fruit juices (even 100% natural fruit juice in large quantities), sports drinks, energy drinks. These are loaded with fructose, which as discussed, increases uric acid production and hinders excretion. They are arguably one of the most significant modern dietary triggers for gout.
- High-Fructose Corn Syrup (HFCS): This omnipresent sweetener is found in countless processed foods, from cereals and baked goods to condiments and snacks. Scrutinize food labels carefully.
- Excessive Fruit Intake (context matters): While whole fruits are generally healthy, those very high in fructose (e.g., mangoes, grapes, pears, dried fruits) should be consumed in moderation, especially if you are sensitive. The fiber in whole fruit mitigates some of the fructose impact compared to juice, but portion control is still wise.
Alcoholic Explosives: The Double-Edged Sword
- Beer: High in purines from yeast and interferes with uric acid excretion. A potent trigger.
- Spirits (Liquor): Can also increase uric acid levels and interfere with excretion, though some studies suggest a lesser effect than beer.
- Wine: Generally considered less risky than beer or spirits, and some studies even suggest moderate wine consumption might not increase gout risk. However, excessive intake of any alcohol can dehydrate and compromise liver function, making it a potential trigger. For gout sufferers, it’s best approached with extreme caution and in very limited quantities.
Other Potential Minefields:
- Certain Vegetables (Misinformation Alert): Historically, some vegetables like spinach, asparagus, mushrooms, and cauliflower were thought to be high-purine dangers. However, modern research has largely debunked this. While they contain moderate purine levels, their overall health benefits, fiber content, and lack of adverse impact on uric acid levels mean they are generally considered safe and beneficial for gout patients. Do not restrict these healthy vegetables based on outdated advice. We’ll revisit this in the "Safe Zones."
- Refined Carbohydrates: White bread, white rice, pasta (non-whole grain). While not direct purine sources, these can contribute to insulin resistance and overall metabolic dysfunction, indirectly increasing gout risk.
Part 3: The Safe Zones & Superfoods – Your Arsenal for Defense
Now, let’s identify the safe paths and the powerful allies in our culinary journey. These are the foods and habits that can actively help lower uric acid levels, reduce inflammation, and strengthen your body’s defenses against gout attacks.
Hydration: The Flushing Powerhouse
- Water, Water, Water: This is your most fundamental and powerful tool. Aim for at least 8-12 glasses (2-3 liters) of water daily. Water helps dilute uric acid in the blood and aids the kidneys in flushing it out of your system. Think of it as constantly clearing the battlefield.
- Herbal Teas: Many herbal teas are excellent hydrating options. Green tea also offers antioxidant benefits.
Low-Fat Dairy Products: The Uric Acid Excretion Boosters
- Skim Milk, Low-Fat Yogurt, Low-Fat Cheese: Studies consistently show that low-fat dairy products are associated with lower uric acid levels and a reduced risk of gout attacks. The exact mechanism isn’t fully understood, but it’s believed that certain proteins in dairy (casein and lactalbumin) enhance uric acid excretion through the kidneys. Consider these your strategic fortifications.
Cherries and Berry Power: The Anti-Inflammatory Warriors
- Tart Cherries (and their juice/extract): This is perhaps the most well-researched "superfood" for gout. Tart cherries are rich in anthocyanins, powerful antioxidants and anti-inflammatory compounds that have been shown to lower uric acid levels and reduce the frequency and severity of gout attacks. Fresh, frozen, juice (unsweetened), or extract – incorporate them regularly.
- Other Berries: Blueberries, strawberries, raspberries. While less potent than tart cherries, these are also packed with antioxidants and anti-inflammatory compounds, making them excellent choices.
Vitamin C: The Uric Acid Lowering Agent
- Citrus Fruits: Oranges, grapefruits, lemons.
- Bell Peppers: Especially red and yellow.
- Broccoli, Kale, Brussels Sprouts: Excellent sources.
- Kiwi: Another Vitamin C powerhouse.
Studies indicate that higher intake of Vitamin C is associated with lower uric acid levels, likely by promoting its excretion. Aim for natural sources, but a supplement (under medical guidance) can also be considered.
Complex Carbohydrates & Fiber: The Foundation of Stability
- Whole Grains: Oats, brown rice, quinoa, whole-wheat bread and pasta. These provide sustained energy, are rich in fiber, and generally have a low glycemic index, which helps manage insulin levels and overall metabolic health.
- Legumes: Lentils, beans (black beans, kidney beans, chickpeas), peas. While some contain moderate purines, their high fiber, protein, and nutrient content make their overall impact beneficial for gout patients. Studies show that plant-based purines do not increase gout risk in the same way animal purines do. They are crucial for a plant-forward diet.
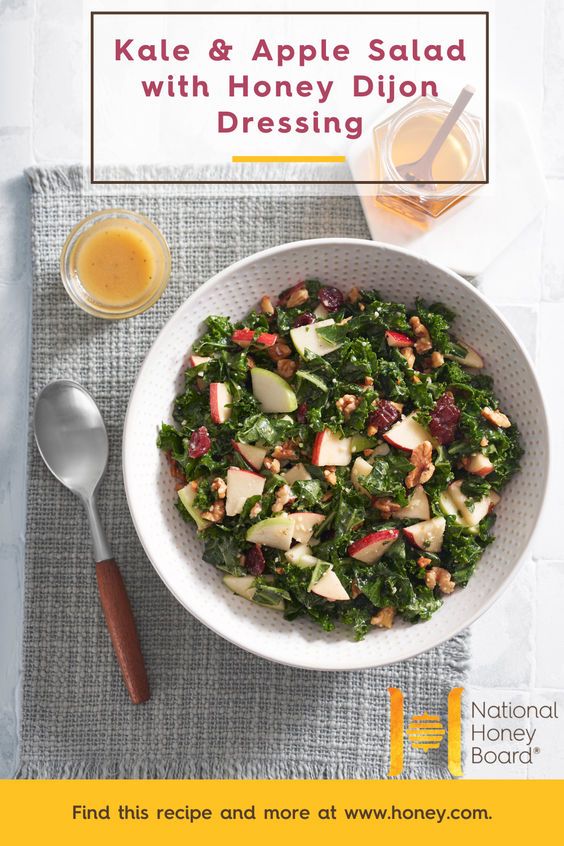
- Vegetables (Yes, Even the "Controversial" Ones): As mentioned earlier, spinach, asparagus, mushrooms, and cauliflower are perfectly safe and beneficial. Load up on a wide variety of vegetables – leafy greens, cruciferous vegetables, root vegetables. They are low in calories, high in fiber, vitamins, and antioxidants, and contribute minimally to uric acid levels. They are your everyday protective gear.
Healthy Fats: The Soothing Agents
- Olive Oil: Extra virgin olive oil is a monounsaturated fat rich in anti-inflammatory compounds.
- Avocados: Another source of healthy monounsaturated fats and fiber.
- Nuts and Seeds: Almonds, walnuts, chia seeds, flax seeds. These provide healthy fats (including omega-3s in walnuts, chia, and flax), fiber, and protein.
- Fatty Fish (in moderation): Salmon, tuna, trout. While these contain moderate purines, their rich omega-3 fatty acid content (EPA and DHA) offers powerful anti-inflammatory benefits that can outweigh the purine contribution for many. It’s a calculated risk, often a beneficial one, consumed in reasonable portions (e.g., 2-3 times a week).
Plant-Based Proteins: The Sustainable Replacements
- Tofu and Tempeh: Excellent sources of complete plant-based protein, generally well-tolerated by gout patients.
- Plant-Based Protein Powders: Pea protein, hemp protein.
- Legumes: (reiterated for their protein content).
These options allow you to reduce your reliance on animal proteins, thereby lowering your overall dietary purine load without sacrificing essential nutrients.
Part 4: Navigating the Battlefield – Practical Strategies & Lifestyle Hacks
Knowing what to eat and what to avoid is one thing; implementing it consistently in daily life is another. This section focuses on the practical tactics and lifestyle adjustments that will help you successfully navigate the minefield day in and day out.
Weight Management: The Strategic Retreat
- Gradual Weight Loss: If you are overweight or obese, losing even 5-10% of your body weight can significantly reduce uric acid levels and the frequency of gout attacks. However, extreme crash diets or rapid weight loss can trigger attacks due to increased purine breakdown. Aim for a slow, steady, sustainable approach (1-2 pounds per week).
- Focus on Whole Foods: A diet rich in whole, unprocessed foods naturally supports healthy weight management.
Portion Control: The Art of Moderation
- Even "Safe" Foods: While most plant-based foods are beneficial, remember that even healthy foods can contribute to overall calorie and nutrient intake. Portion control is always important for weight management and overall health.
- High-Purine Foods (if consumed): If you occasionally choose to indulge in a moderate portion of a higher-purine food (like a small steak or a serving of salmon), ensure it’s an infrequent treat, not a regular occurrence.
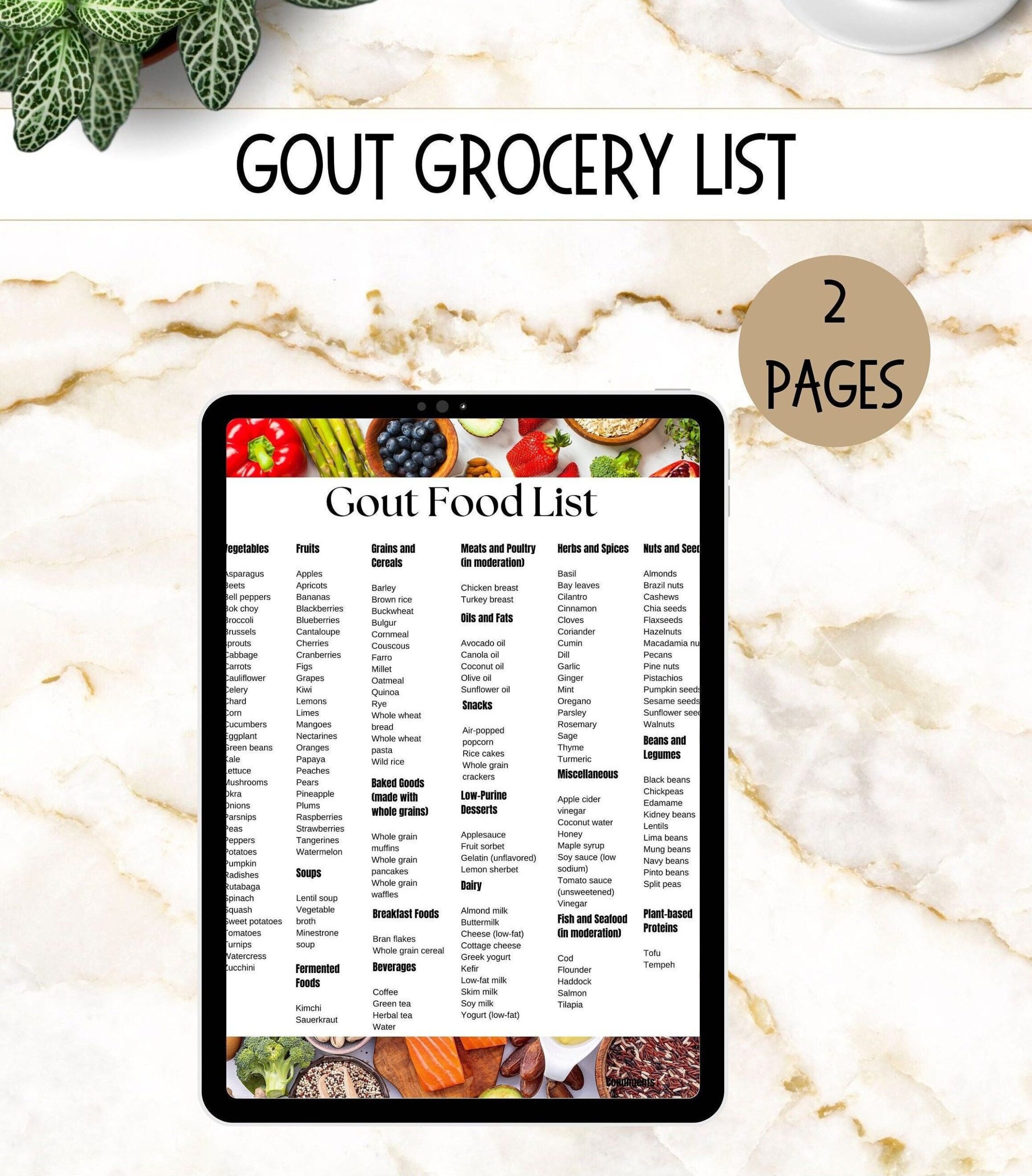
Meal Planning & Preparation: Taking Control
- Plan Ahead: Dedicate time each week to plan your meals and snacks. This reduces impulse decisions and ensures you have gout-friendly options readily available.
- Grocery Shopping: Shop with a list, focusing on whole, unprocessed ingredients from the "safe zones."
- Batch Cooking: Prepare larger quantities of healthy meals and store them for quick access throughout the week. This is a game-changer for consistency.
- Read Food Labels Religiously: Become a detective. Look for hidden sugars, especially high-fructose corn syrup, in sauces, dressings, yogurts, and packaged snacks. "Natural flavors" can sometimes mask fructose.
Cooking Methods: The Culinary Tactics
- Lean Cooking: Opt for baking, grilling, broiling, steaming, or stir-frying with minimal healthy fats (like olive oil) instead of deep-frying.
- Flavor Boosters: Use herbs, spices, lemon juice, and vinegars to add flavor without relying on high-sodium or high-sugar ingredients.
Supplements: The Auxiliary Support (with Caution)
- Always Consult Your Doctor: Before starting any supplements, discuss them with your healthcare provider. Supplements are not a replacement for medication or a healthy diet.
- Tart Cherry Extract: A concentrated form of the benefits found in tart cherries.
- Vitamin C: If dietary intake is insufficient, a supplement might be considered.
- Omega-3 Fatty Acids: Fish oil supplements can help reduce overall inflammation, but be mindful of any purines in fish oil if derived from high-purine fish (though generally purified). Plant-based omega-3s (algae oil) are an alternative.
Stress Management: The Mental Fortification
- Mind-Body Connection: Chronic stress can exacerbate inflammation throughout the body. While not a direct dietary trigger, managing stress through mindfulness, meditation, yoga, or hobbies can indirectly support overall health and potentially reduce the frequency or intensity of gout attacks.
Sleep: The Essential Recovery
- Quality Sleep: Prioritize 7-9 hours of quality sleep per night. Sleep deprivation can increase systemic inflammation and negatively impact metabolic health.
Exercise: The Physical Conditioning
- Regular Physical Activity: Alongside diet, exercise is critical for weight management, improving insulin sensitivity, and reducing inflammation. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, plus strength training a couple of times a week. Choose activities that are low-impact on your joints during periods of remission.
Part 5: Beyond the Plate – The Holistic Approach and Long Game
Understanding the minefield and mastering the tactics is crucial, but true victory lies in adopting a holistic strategy that integrates diet with professional medical care and a long-term perspective.
Medication and Diet: A Symbiotic Relationship
- Diet is Complementary, Not a Cure-All: It is imperative to understand that dietary changes, while powerful, are usually complementary to prescribed medication for gout management. For many, medication (like allopurinol or febuxostat to lower uric acid, or colchicine/NSAIDs for acute attacks) is essential to achieve and maintain target uric acid levels. Diet helps to support this, reduce the need for higher doses, and minimize triggers. Never discontinue medication without consulting your doctor.
- Individual Variability: Gout is highly individual. What triggers one person might not affect another. This is where personalized medicine and careful tracking come in.
Working with Professionals: Your Expert Guidance
- Rheumatologist: This specialist will manage your medication and overall gout treatment plan. Openly discuss your dietary efforts with them.
- Registered Dietitian (RD) / Nutritionist: A dietitian specializing in chronic diseases can provide personalized dietary advice, help you create meal plans, identify specific triggers, and ensure you’re meeting all your nutritional needs while managing gout. They are invaluable guides in this complex terrain.
Tracking and Learning: Your Personal Intelligence Gathering
- Food Diary: Keep a detailed food diary, especially when starting new dietary changes or if you experience a flare-up. Record everything you eat and drink, along with any symptoms or attacks. This can help you identify your unique triggers and sensitivities.
- Symptom Journal: Note the severity and duration of attacks, any medications taken, and any suspected dietary links.
- Uric Acid Monitoring: Regular blood tests to monitor your uric acid levels (as directed by your doctor) are essential to gauge the effectiveness of your diet and medication.
Patience and Persistence: The Marathon Mindset
- It’s a Journey, Not a Destination: Managing gout is a long-term commitment. There will be good days and bad days, successes and setbacks. Don’t get discouraged by occasional slip-ups or unexpected flare-ups. Learn from them and keep moving forward.
- Focus on Progress, Not Perfection: Aim for consistent healthy eating habits rather than striving for an impossible standard of perfection. Small, sustainable changes add up over time.
- Celebrate Small Victories: A week without an attack, a lower uric acid reading, successfully navigating a social event with gout-friendly choices – acknowledge and celebrate these achievements.
Conclusion: Disarming the Minefield, Reclaiming Your Life
You’ve now traversed the landscape of gout-friendly eating, armed with scientific understanding, a detailed map of dietary risks and safe zones, and a practical guide to daily navigation. The "minefield" of gout-inducing foods no longer needs to be a source of constant anxiety. Instead, it becomes a challenge you are equipped to meet, a landscape you can confidently traverse.
Remember, this journey is about empowerment. It’s about taking control of what you put into your body, understanding its profound impact on your health, and making conscious choices that support your well-being. Gout management is a multifaceted endeavor, and while diet is not the sole solution, it is an incredibly powerful and often underestimated component.
By embracing whole, unprocessed foods, prioritizing hydration, carefully managing your intake of purines and fructose, and integrating healthy lifestyle habits, you are not just preventing future attacks; you are actively building a more resilient, vibrant you. You are reclaiming the joy of eating, the freedom of movement, and the peace of mind that comes with proactive self-care.
Step forward with confidence. The minefield has been mapped, the dangers understood, and your arsenal for defense is ready. This is your story of triumph over pain, a testament to the power of knowledge, and a blueprint for a life where gout no longer dictates your choices, but rather, inspires a healthier, happier you.