Flare-Up Frequency: Why Your Gout Keeps Returning and How to Stop It
For those who have experienced it, gout is more than just a joint condition; it’s a thief of mobility, a destroyer of plans, and a source of profound frustration. But perhaps the most disheartening aspect is its tendency to return, again and again, trapping individuals in a seemingly endless cycle of pain and recovery. If you’re nodding your head in weary recognition, you’re not alone. This article is for you – the knowledgeable individual seeking to understand not just what gout is, but why it keeps coming back, and more importantly, how to break free from its grip once and for all.
This isn’t just about managing the pain of a flare; it’s about rewriting your story with gout, moving from a narrative of recurrent suffering to one of sustained remission and reclaimed quality of life. We’re going to delve deep into the science, the common pitfalls, and the strategic interventions necessary to silence the alarm bells of your body and truly stop the cycle of recurring gout flares.
The Insidious Nature of Gout: More Than Just a Painful Joint
Before we tackle the "why," it’s crucial to solidify our understanding of what gout truly is. It’s often misunderstood as a simple lifestyle disease, a consequence of indulgence. While lifestyle factors play a significant role, the underlying mechanism is a complex interplay of genetics, metabolism, and immunology.
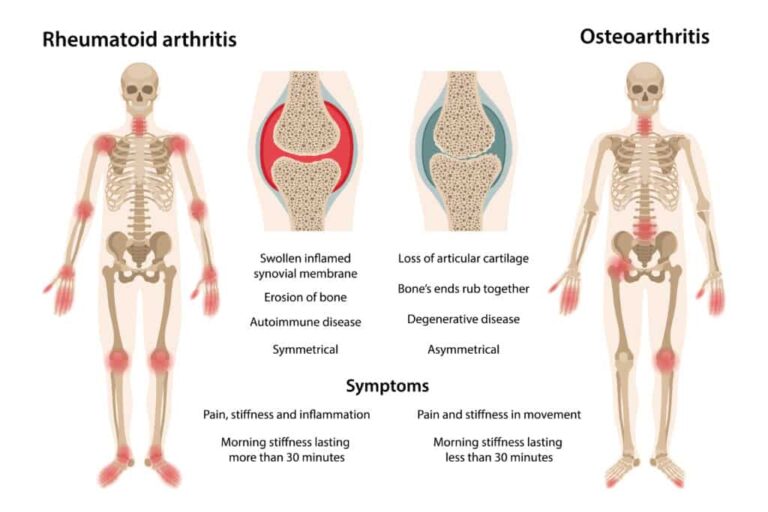
Gout is a form of inflammatory arthritis caused by the deposition of monosodium urate (MSU) crystals in joints and soft tissues. These crystals are the direct result of hyperuricemia – persistently elevated levels of uric acid in the blood. Uric acid is a natural byproduct of purine metabolism (purines are found in many foods and are also produced by your body). Normally, your kidneys efficiently filter out excess uric acid. However, if your body produces too much uric acid, or your kidneys don’t excrete enough (the most common scenario), uric acid levels can rise to a point where it supersaturates the blood.
At these supersaturated concentrations, uric acid can crystallize, forming sharp, needle-like MSU crystals. These crystals often prefer cooler areas of the body, like the big toe, but can appear in almost any joint. When these crystals shed from their deposits into the joint space, your immune system perceives them as foreign invaders. This triggers a powerful inflammatory response, orchestrated in part by the NLRP3 inflammasome pathway, leading to the characteristic excruciating pain, swelling, redness, and heat of a gout flare.
The "Silent" Enemy: Asymptomatic Hyperuricemia
One of the most insidious aspects of gout is the period of asymptomatic hyperuricemia. For years, or even decades, an individual can have elevated uric acid levels without experiencing a single flare. During this time, MSU crystals are silently forming and depositing in joints and tissues. This is the "iceberg" effect: the first flare is often just the tip, with significant crystal deposits already accumulated beneath the surface.
This silent phase is critical because it highlights that gout is a chronic disease, not just an episodic one. A flare is merely the symptom of the underlying problem: the presence of MSU crystal deposits driven by sustained hyperuricemia. Understanding this fundamental truth is the first step toward breaking the cycle.
Why Your Gout Keeps Returning: Unpacking the "Why"
The return of gout flares is rarely a random event. It’s almost always a signal that the underlying problem – crystal deposition – has not been adequately addressed, or that new triggers are exacerbating the existing issue. Let’s dissect the primary reasons why gout keeps making an unwelcome comeback.
1. Inadequate Urate-Lowering Therapy (ULT): The Most Common Culprit
This is, by far, the leading reason for recurrent gout flares. Many individuals with gout are either not on ULT, or if they are, the therapy is not optimized to achieve the target serum urate level.
- The Misconception of "Normal" Uric Acid: A common pitfall is the idea that "normal" uric acid levels are sufficient. For a gout patient, a serum urate level that is "normal" for the general population (e.g., <7 mg/dL) is often still too high to dissolve existing MSU crystals. The therapeutic target for gout patients is typically below 6 mg/dL (360 µmol/L), and often below 5 mg/dL (300 µmol/L) for those with severe, chronic gout, to facilitate the dissolution of crystal deposits. If your uric acid level consistently remains above this target, new crystals will continue to form, and existing ones will not dissolve, ensuring future flares.
- Insufficient Dosage or Duration: ULT medications like allopurinol or febuxostat need to be titrated (gradually increased) to reach the target serum urate. Many patients are kept on a low, sub-optimal dose, never achieving the critical dissolution threshold. Furthermore, ULT is a lifelong commitment for most; stopping therapy once symptoms subside is a guaranteed path to recurrence.
- Lack of Adherence: Taking medication consistently can be challenging. Reasons for non-adherence include:
- Feeling Better: Once flares subside, some patients mistakenly believe they are "cured" and stop taking their medication.
- Fear of Side Effects: While side effects can occur, they are often manageable, and the benefits of preventing flares far outweigh the risks for most.
- Misunderstanding: Patients may not fully grasp the chronic nature of gout or the lifelong necessity of ULT.
- Cost or Access: Financial barriers or difficulty accessing prescriptions can also impede adherence.
2. Mismanagement of Acute Flares During ULT Initiation
Paradoxically, starting or increasing ULT can sometimes trigger a flare. This is not a sign that the medication isn’t working; rather, it’s often a sign that the crystals are beginning to dissolve. As MSU crystals dissolve, they can become destabilized and shed into the joint space, provoking an inflammatory response.
- Lack of Prophylaxis: To counteract this, it’s crucial to co-prescribe anti-inflammatory medication (like low-dose colchicine or NSAIDs) for the first few months when initiating or titrating ULT. If this prophylactic treatment is omitted, patients may experience flares, become discouraged, and discontinue their ULT, thinking it’s making their condition worse.
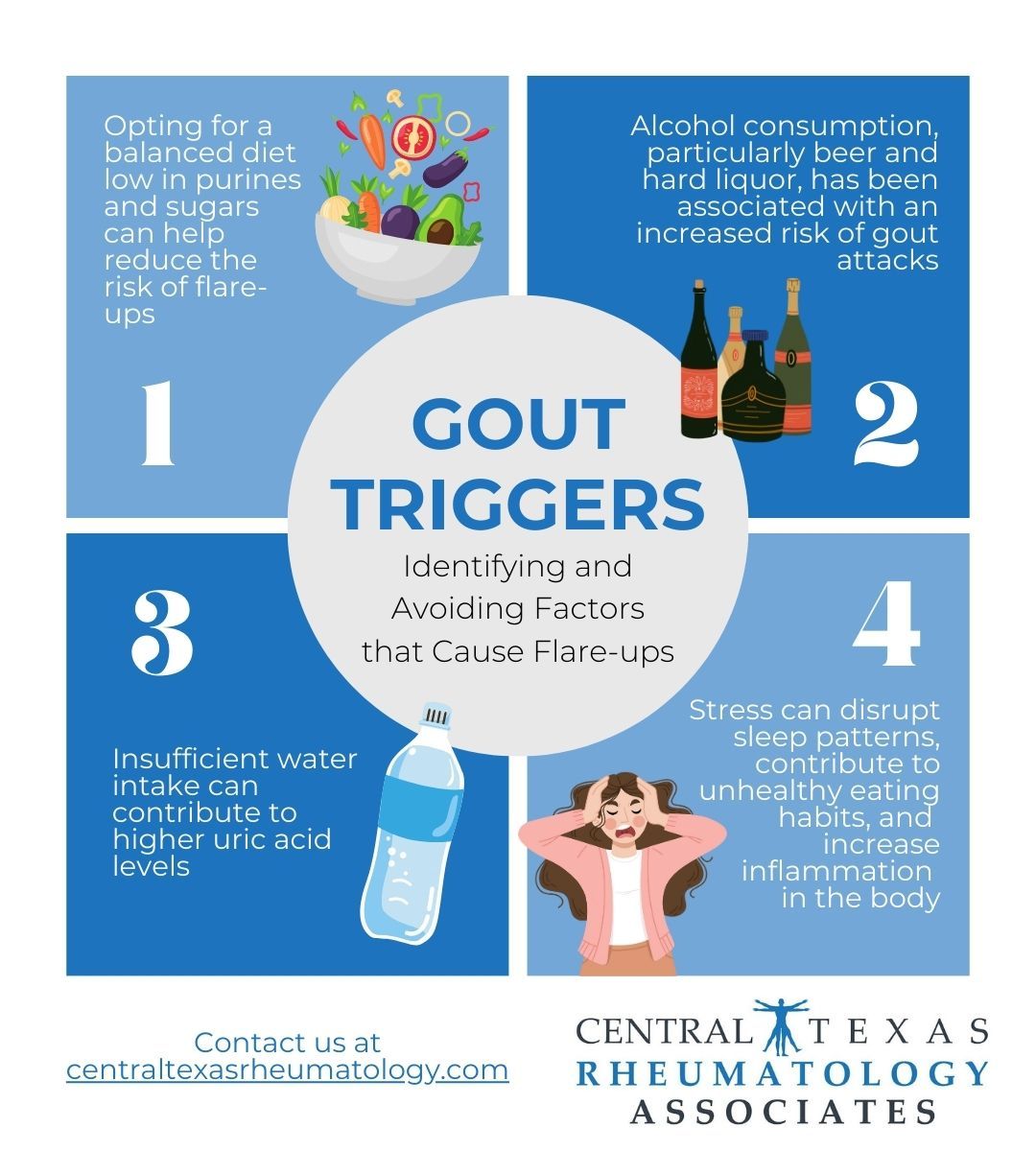
3. Lifestyle Triggers: The Catalysts, Not Always the Cause
While inadequate ULT is the primary driver, lifestyle factors act as powerful triggers, igniting flares in individuals with existing crystal deposits. It’s important to remember these are usually catalysts, not the sole cause; you can have a perfect diet but still experience flares if your uric acid is too high.
- Dietary Choices: High-purine foods (red meat, organ meats, certain seafood like anchovies, sardines, mussels), high-fructose corn syrup, and excessive sugar intake can acutely raise uric acid levels or increase inflammation.
- Alcohol Consumption: Beer and spirits are particularly problematic due to their purine content and impact on kidney function. Even wine, while less impactful, can trigger flares in susceptible individuals. Alcohol increases uric acid production and reduces its excretion.
- Dehydration: Concentrates uric acid in the blood and can make crystal formation more likely.
- Sudden Weight Loss or Gain: Rapid fluctuations can destabilize uric acid levels.
- Trauma or Injury: Even minor joint trauma can release crystals into the joint space, initiating a flare.
- Stress: Physical and emotional stress can trigger an inflammatory response, exacerbating the likelihood of a flare.
- Certain Medications: Diuretics (water pills) and some blood pressure medications can increase uric acid levels. Aspirin in low doses can also interfere with uric acid excretion.
4. Co-morbid Conditions and Other Medical Factors
Gout often doesn’t travel alone. It frequently coexists with other health conditions that can either contribute to hyperuricemia or make gout management more complex.
- Kidney Disease: Impaired kidney function is a major cause of reduced uric acid excretion, leading to hyperuricemia. As kidney disease progresses, managing gout becomes more challenging.
- Metabolic Syndrome/Obesity: Insulin resistance, high blood pressure, high cholesterol, and abdominal obesity are strongly linked to hyperuricemia and gout. These conditions can impair renal urate excretion.
- Cardiovascular Disease: Gout is independently associated with an increased risk of heart disease and stroke. The chronic inflammation associated with gout contributes to vascular damage.
- Psoriasis: A chronic autoimmune skin condition that can also be associated with elevated uric acid levels.
5. Misdiagnosis or Incomplete Diagnosis
While less common for recurrent flares, an initial misdiagnosis can lead to inappropriate treatment. Other conditions, such as pseudogout (calcium pyrophosphate deposition disease), septic arthritis, or other inflammatory arthritides, can mimic gout. A definitive diagnosis of gout requires joint aspiration and identification of MSU crystals under polarized light microscopy. Without this, treatment might not be tailored to the specific pathology.
How to Stop the Cycle: A Comprehensive Strategy for Sustained Remission
Breaking free from the relentless cycle of gout flares requires a multi-faceted, proactive, and patient-centered approach. It’s not just about treating symptoms; it’s about addressing the root cause and maintaining long-term control.
1. Re-evaluate and Optimize Urate-Lowering Therapy (ULT)
This is the cornerstone of effective gout management.
- Confirm Diagnosis: If not already done, consider joint aspiration to confirm MSU crystals, especially if the presentation is atypical or response to treatment is poor.
- Establish a Clear Serum Urate Target: Work with your rheumatologist to ensure your serum urate is consistently below 6 mg/dL (360 µmol/L), and ideally below 5 mg/dL (300 µmol/L) if you have extensive crystal deposits (tophi) or very frequent flares.
- Consistent Monitoring: Regular blood tests (every few weeks initially, then every 6-12 months once stable) are crucial to ensure your uric acid levels remain within the target range.
- Medication Adherence:
- Understand Your Meds: Ask your doctor or pharmacist about how your ULT works, its potential side effects, and why lifelong adherence is important.
- Don’t Stop When You Feel Better: This is a critical message. ULT works by slowly dissolving crystal deposits, a process that takes months to years. Stopping therapy prematurely guarantees recurrence.
- Manage Side Effects: If you experience side effects, discuss them with your doctor. There may be alternative medications or strategies to mitigate them.
- Explore All ULT Options:
- Xanthine Oxidase Inhibitors (XOIs): Allopurinol (first-line for most) and Febuxostat. These reduce uric acid production. Allopurinol needs to be started at a low dose and slowly titrated up. Febuxostat can be an alternative if allopurinol is not tolerated or effective.
- Uricosurics: Probenecid. These help the kidneys excrete more uric acid. Used when XOIs are insufficient or contraindicated.
- Pegloticase: For severe, refractory gout that doesn’t respond to other treatments. This is an intravenous enzyme that rapidly breaks down uric acid.
- Newer Agents: Discuss with your rheumatologist if other options like lesinurad (often used in combination with an XOI) are appropriate for your case.
2. Prophylactic Anti-Inflammatory Therapy During ULT Initiation
To prevent initial flares when starting or increasing ULT:
- Low-Dose Colchicine: Typically 0.6 mg once or twice daily, for 3-6 months or until the serum urate target has been consistently met and the patient has been flare-free for several months.
- NSAIDs: Non-steroidal anti-inflammatory drugs (e.g., naproxen, ibuprofen) can also be used, but with caution, especially in patients with kidney disease or cardiovascular issues.
- Corticosteroids: May be considered in specific cases where colchicine or NSAIDs are contraindicated or ineffective.
3. Strategic Lifestyle Modifications: Supporting Your Treatment
While diet alone won’t cure gout, it plays a vital supportive role in conjunction with effective ULT.
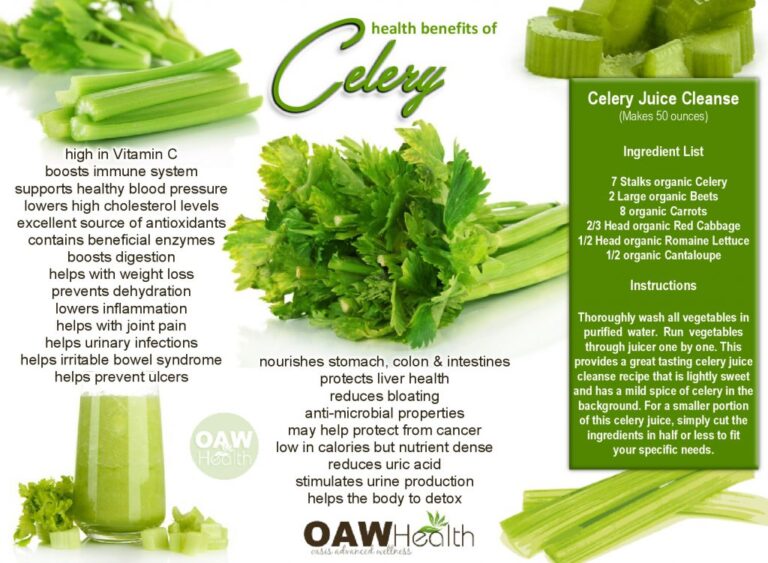
- Hydration: Drink plenty of water throughout the day. Aim for clear urine. This helps flush uric acid from your system.
- Weight Management: If overweight or obese, gradual weight loss can significantly improve uric acid levels and reduce the strain on joints. Avoid crash diets, as rapid weight loss can trigger flares.
- Dietary Choices:
- Limit High-Purine Foods: Organ meats (liver, kidney), red meat, certain seafood (sardines, anchovies, mussels, scallops, tuna).
- Avoid High-Fructose Corn Syrup & Sugary Drinks: These significantly increase uric acid production.
- Moderate Alcohol Intake: Especially beer and spirits. Wine appears to have a lesser, but still present, effect.
- Include Urate-Lowering Foods: Low-fat dairy products (milk, yogurt), vitamin C (cherries, oranges, strawberries), and coffee have been shown to potentially lower uric acid levels.
- Prioritize Whole Foods: Fruits, vegetables, whole grains, and lean proteins.
- Exercise: Regular, moderate exercise can help with weight management and overall health. Avoid high-impact activities during flares.
- Stress Management: Chronic stress can exacerbate inflammatory conditions. Incorporate stress-reduction techniques like meditation, yoga, or spending time in nature.
4. Comprehensive Management of Co-morbid Conditions
Work closely with your healthcare team to manage any co-existing conditions.
- Kidney Disease: Essential to monitor kidney function and adjust ULT dosages accordingly.
- Metabolic Syndrome/Diabetes/Hypertension: Addressing these conditions with diet, exercise, and appropriate medications can indirectly help manage gout.
- Medication Review: Discuss all your medications with your doctor, as some (e.g., diuretics, low-dose aspirin) might be contributing to hyperuricemia. Alternatives may be available.
5. Patient Empowerment and Education
Knowledge is power. The more you understand about gout, the better equipped you’ll be to manage it effectively.
- Keep a Flare Diary: Track flare frequency, severity, potential triggers, and your response to treatment. This data can be invaluable for your doctor.
- Ask Questions: Don’t hesitate to ask your doctor about your serum urate target, medication choices, and potential side effects.
- Advocate for Yourself: If you feel your gout is not adequately controlled, seek a referral to a rheumatologist, who specializes in inflammatory joint conditions.
- Understand the Long Game: Gout management is a marathon, not a sprint. Be prepared for a lifelong commitment to monitoring and therapy.
6. The Role of the Healthcare Team
You are not alone in this journey. A multidisciplinary approach often yields the best results.
- Primary Care Physician (PCP): Often the first point of contact, managing routine care, monitoring, and prescribing initial ULT.
- Rheumatologist: The specialist who should ideally manage moderate to severe or complex gout, especially if flares are recurrent, if there are tophi, or if ULT is challenging.
- Nephrologist: If kidney disease is a significant factor.
- Dietitian: Can provide personalized guidance on dietary modifications.
Living Beyond Flares: A Future of Remission
Imagine a life where the fear of the next gout flare doesn’t loom over every meal, every social gathering, every morning. This is not an impossible dream. For the vast majority of individuals, consistent and optimized urate-lowering therapy, combined with strategic lifestyle adjustments, can lead to a state of sustained remission.
When gout is effectively managed, not only do the flares cease, but the underlying crystal deposits slowly dissolve. This prevents further joint damage, preserves mobility, and significantly improves your overall quality of life. Furthermore, by addressing hyperuricemia and its associated comorbidities, you are also taking proactive steps to reduce your risk of other serious health issues, particularly cardiovascular disease.
Breaking the cycle of recurring gout flares is a journey that requires commitment, patience, and a close partnership with your healthcare team. It demands moving beyond reactive symptom management to proactive disease control. But the rewards – a life free from the debilitating pain, the fear, and the limitations of gout – are immeasurable.
Your story with gout doesn’t have to be one of endless recurrence. It can be one of understanding, empowerment, and ultimately, liberation. By embracing the comprehensive strategy outlined here, you can reclaim your health, your mobility, and your peace of mind, transforming your narrative from one of persistent suffering to one of lasting remission. The power to stop the return of gout is within your grasp.