The Ultimate Gout Food List: Eat This, Not That – Reclaiming Your Plate, Reclaiming Your Life
The fire in your joint ignites without warning. One moment, you’re simply existing; the next, a searing, debilitating pain flares, usually in your big toe, making even the weight of a bedsheet unbearable. This, for millions, is the agonizing reality of a gout attack – a silent, metabolic war erupting into a crippling battle. If you’re reading this, you likely know this pain intimately, or you’re on the precipice of understanding it. You’ve heard the whispers, the warnings, the conflicting advice: “Don’t eat red meat!” “Avoid seafood!” “Is that beer going to kill me?”
The narrative around gout often feels like a story of deprivation, a constant fear of food. But what if we told you it doesn’t have to be? What if the "Ultimate Gout Food List" isn’t about what you can’t have, but about the incredible abundance you can embrace? This isn’t just a list; it’s a guide to reclaiming your plate, understanding the intricate dance between your diet and your body, and ultimately, reclaiming your life from the shadow of gout.
Our journey begins not with restrictions, but with understanding. For the knowledgeable individual, you know gout is more than just joint pain; it’s a form of inflammatory arthritis caused by elevated levels of uric acid in the blood (hyperuricemia). When uric acid crystals accumulate in the joints, they trigger that excruciating inflammation. And while genetics play a role, diet is often the most powerful lever we have to pull.
Forget the simplistic notion that all high-purine foods are evil. The science has evolved, and so too should our approach. This comprehensive guide will empower you to navigate your dietary landscape with confidence, turning fear into informed choice, and transforming your kitchen into a sanctuary of healing.
>
Part 1: Beyond the Purine Panic – Understanding the True Dietary Triggers
Before we dive into the "Eat This, Not That," it’s crucial to grasp that gout is a complex metabolic disorder. While purines (compounds that break down into uric acid) are a significant factor, they are not the only factor. For a truly effective dietary strategy, we need to look at the bigger picture:
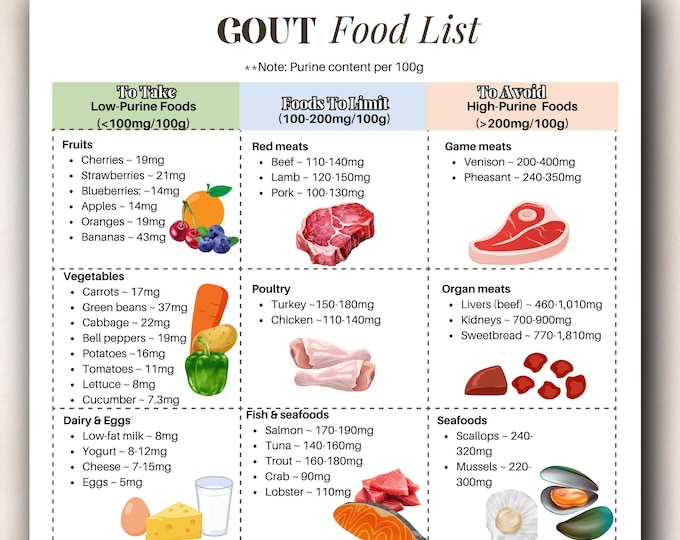
- Purine Content: Yes, some foods are naturally high in purines, and their breakdown contributes directly to uric acid levels. This remains a cornerstone of gout diet advice.
- Fructose Metabolism: This is often an underappreciated culprit. High-fructose corn syrup (HFCS) and even natural fruit sugars, in excess, can significantly increase uric acid production through a distinct metabolic pathway in the liver, independent of purines.
- Alcohol Consumption: Different types of alcohol affect uric acid differently, but all can be problematic. Alcohol interferes with uric acid excretion by the kidneys and can increase its production. Beer, in particular, contains purines.
- Insulin Resistance & Metabolic Syndrome: Gout often coexists with conditions like obesity, type 2 diabetes, high blood pressure, and high cholesterol – collectively known as metabolic syndrome. Diets high in refined carbohydrates and unhealthy fats contribute to insulin resistance, which can impair the kidneys’ ability to excrete uric acid.
- Inflammation: Beyond uric acid, gout is an inflammatory disease. Foods that promote systemic inflammation can exacerbate attacks, while anti-inflammatory foods can help mitigate them.
- Hydration: Water is a silent hero. Proper hydration helps the kidneys flush out uric acid.
Understanding these interconnected factors allows us to build a more nuanced, effective, and sustainable dietary plan. It’s not just about avoiding purines; it’s about nurturing a body that is less prone to hyperuricemia and inflammation.
>
Part 2: The "Eat This" List – Abundance, Anti-Inflammation, and Uric Acid Balance
This is where we shift from fear to freedom, from restriction to abundance. The cornerstone of a gout-friendly diet is not what you must forgo, but the vast array of delicious, nutritious foods that actively work with your body to manage uric acid, reduce inflammation, and promote overall health.
1. The Mighty Fruits: Nature’s Sweet Medicine
Don’t let the fear of fructose deter you from the incredible benefits of whole fruits. While excessive added fructose is problematic, the fructose in whole fruits comes packaged with fiber, antioxidants, and vitamins that offer protective effects.
- Cherries (Especially Tart Cherries): If there’s a superstar in the gout diet, it’s the cherry. Numerous studies have shown that cherries, particularly tart varieties, can lower uric acid levels and reduce the frequency and severity of gout attacks. Their power comes from anthocyanins, potent antioxidants and anti-inflammatory compounds.
- How to Enjoy: Fresh, frozen, tart cherry juice (unsweetened, diluted), or even tart cherry extract supplements (consult your doctor).
- Berries (Strawberries, Blueberries, Raspberries): Like cherries, berries are packed with antioxidants and anti-inflammatory compounds. They’re also relatively low in fructose and high in fiber.
- How to Enjoy: Smoothies, oatmeal toppings, snacks, or in salads.
- Citrus Fruits (Oranges, Grapefruits, Lemons, Limes): Rich in Vitamin C, which has been shown to reduce uric acid levels.
- How to Enjoy: Freshly squeezed juice, added to water, or as part of meals.
- Apples & Pears: Good sources of fiber and antioxidants.
- Bananas: While slightly higher in natural sugars, their potassium content can be beneficial, and they are generally well-tolerated.
2. The Verdant Victory: Vegetables Galore
For years, there was a misconception that all vegetables, especially those high in purines, should be avoided. This myth has been thoroughly debunked. Research consistently shows that vegetables, even those with moderate purine levels (like spinach, asparagus, mushrooms, cauliflower), do not increase the risk of gout or gout attacks. In fact, they are protective!
- Leafy Greens (Spinach, Kale, Collard Greens): High in vitamins, minerals, fiber, and antioxidants. While spinach has moderate purines, its overall health benefits far outweigh any theoretical risk for gout sufferers.
- How to Enjoy: Salads, smoothies, sautéed, added to soups and stews.
- Cruciferous Vegetables (Broccoli, Brussels Sprouts, Cabbage): Excellent sources of Vitamin C, K, and fiber. They also contain compounds that support detoxification.
- How to Enjoy: Roasted, steamed, stir-fried.
- Alliums (Onions, Garlic): Known for their anti-inflammatory and immune-boosting properties.
- How to Enjoy: As a base for almost any savory dish.
- Root Vegetables (Carrots, Potatoes, Sweet Potatoes): Good sources of complex carbohydrates, fiber, and various vitamins.
- Bell Peppers: High in Vitamin C and antioxidants.
3. Whole Grains: Fueling Your Body Wisely
Opt for unrefined, whole grains over highly processed ones. They provide sustained energy, fiber (which helps regulate blood sugar and promotes satiety), and important nutrients.
- Oats: A fantastic breakfast choice, rich in soluble fiber.
- Brown Rice, Quinoa, Farro, Barley: Excellent alternatives to white rice and refined pastas.
- Whole-Wheat Bread & Pasta: In moderation, choose varieties with minimal added sugars.
4. Dairy Delights: A Surprising Ally
Low-fat dairy products have been consistently linked to a lower risk of gout. The exact mechanism isn’t fully understood, but it’s believed that certain proteins in dairy (casein and lactalbumin) may enhance uric acid excretion by the kidneys.
- Low-Fat Milk: An easy way to incorporate dairy.
- Low-Fat Yogurt (Plain, Unsweetened): Contains probiotics beneficial for gut health.
- Low-Fat Cheese: In moderation.
5. Healthy Fats: The Anti-Inflammatory Powerhouses
Not all fats are created equal. Focus on sources of monounsaturated and polyunsaturated fats, especially Omega-3 fatty acids, which are potent anti-inflammatory agents.
- Olive Oil (Extra Virgin): A cornerstone of the Mediterranean diet, known for its heart-healthy and anti-inflammatory properties.
- Avocado: Rich in monounsaturated fats, fiber, and potassium.
- Nuts & Seeds (Almonds, Walnuts, Chia Seeds, Flaxseeds): Provide healthy fats, fiber, and protein. Walnuts, in particular, are rich in Omega-3s.
- Fish Oil/Omega-3 Supplements: While fatty fish can be high in purines (see "Not That" list for specifics), fish oil supplements (free of purines) can provide the beneficial Omega-3s without the purine load. Always discuss with your doctor.
6. Plant-Based Proteins: Dispelling the Purine Myth
Many plant-based protein sources, even those with moderate purine levels, do not seem to increase gout risk and can even be protective. This is likely due to their overall nutrient profile, including fiber and beneficial phytochemicals.
- Legumes (Lentils, Beans, Chickpeas): Excellent sources of protein, fiber, and complex carbohydrates.
- Tofu & Tempeh: Soy-based products that are good protein sources.
- Peas: Another good plant-based protein option.
7. Hydration: Your Body’s Internal Cleanser
This is perhaps the simplest yet most crucial dietary intervention. Water helps your kidneys flush out uric acid and prevents the formation of crystals.
- Water: Make it your primary beverage. Aim for at least 8-12 glasses (2-3 liters) daily, more if you’re active or in a hot climate.
- Herbal Teas: Unsweetened varieties can contribute to your fluid intake.
- Coffee: Surprisingly, regular coffee consumption has been associated with a lower risk of gout. Moderate amounts (2-4 cups daily) are generally considered safe and potentially beneficial.
>
Part 3: The "Not That" List – Strategic Moderation and Careful Avoidance
This section isn’t about rigid prohibition but about informed choices. Some foods, due to their high purine content, their impact on uric acid metabolism, or their inflammatory properties, warrant significant reduction or complete avoidance, especially during a flare-up.
1. High-Purine Animal Proteins: The Primary Offenders
While animal proteins are essential for many diets, certain types are particularly problematic for gout sufferers.
- Organ Meats (Liver, Kidney, Sweetbreads): These are exceptionally high in purines and should be strictly avoided.
- Certain Seafood: Some fish and shellfish are very high in purines.
- High Purine Seafood to Avoid: Anchovies, sardines, herring, mussels, scallops, cod, haddock, trout.
- Moderate Purine Seafood (Consume Sparingly): Tuna, shrimp, crab, lobster.
- Red Meat (Beef, Lamb, Pork): While not as high in purines as organ meats, regular consumption of large portions of red meat can increase gout risk.
- Recommendation: Limit red meat to 2-3 servings per week, and opt for lean cuts.
- Poultry (Chicken, Turkey): Generally lower in purines than red meat, but very large portions can still contribute.
- Recommendation: Lean poultry in moderation is usually fine.
2. The Sugary Saboteurs: Fructose and Added Sugars
This is a critical area often overlooked in traditional gout advice. The metabolism of fructose directly leads to uric acid production, regardless of purine content.
- Sugary Drinks (Sodas, Fruit Juices with Added Sugar): These are perhaps the biggest dietary culprits for rising uric acid levels. The high concentration of fructose delivers a direct hit to your uric acid metabolism.
- High-Fructose Corn Syrup (HFCS): Found in countless processed foods, candies, pastries, and even some seemingly healthy items. Read labels diligently.
- Excessive Natural Fruit Juices: Even 100% fruit juice, without the fiber of whole fruit, can deliver a concentrated dose of fructose. Opt for whole fruits instead.
- Candy, Pastries, Desserts: Often loaded with added sugars and HFCS.
3. Alcohol: A Double-Edged Sword
Alcohol can both increase uric acid production and reduce its excretion, making it a significant trigger for gout attacks.
- Beer: Contains purines and is particularly problematic.
- Spirits (Liquor): While not containing purines, they still impair uric acid excretion.
- Wine: Generally considered the least problematic alcohol for gout, but even wine can trigger attacks in some individuals, especially in excess.
- Recommendation: If you must drink, do so in very strict moderation, and avoid during active flares. Many experts advise complete avoidance for optimal gout management.
4. Refined Carbohydrates: The Silent Contributors
Foods made with refined flours (white bread, white pasta, white rice, many breakfast cereals) lack fiber and can contribute to insulin resistance, which, as discussed, impacts uric acid excretion.
- White Bread, Pastries, Cakes: Limit these in favor of whole-grain alternatives.
- Processed Snacks: Chips, crackers, and similar items often contain refined carbs, unhealthy fats, and added sugars.
5. High-Sodium and Processed Foods: General Unhealthiness
While not directly purine-related, highly processed foods and those high in sodium contribute to overall inflammation, poor kidney function, and other metabolic issues that can indirectly exacerbate gout.
- Fast Food, Processed Meats (Bacon, Sausage, Deli Meats): Often high in unhealthy fats, sodium, and sometimes purines.
- Convenience Meals: Typically loaded with sodium, sugar, and unhealthy fats.
>
Part 4: Beyond the Plate – A Holistic Approach to Gout Management
Diet is incredibly powerful, but it’s one piece of a larger puzzle. To truly reclaim your life from gout, consider these lifestyle factors:
- Weight Management: Obesity is a significant risk factor for gout. Losing weight, even a modest amount, can dramatically reduce uric acid levels and the frequency of attacks. However, rapid weight loss (crash diets) can sometimes trigger attacks, so aim for a slow, steady approach.
- Hydration is Key (Again!): We can’t stress this enough. Consistent water intake is your body’s best friend in flushing out excess uric acid.
- Regular Exercise: Physical activity helps with weight management, improves insulin sensitivity, and reduces inflammation. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Stress Management: Chronic stress can increase inflammation in the body, potentially exacerbating gout. Incorporate stress-reducing activities like meditation, yoga, deep breathing exercises, or hobbies you enjoy.
- Adequate Sleep: Prioritize 7-9 hours of quality sleep per night. Sleep deprivation can contribute to inflammation and metabolic dysfunction.
- Supplements (with Caution): While diet is primary, some supplements may offer additional support.
- Vitamin C: As mentioned, can help lower uric acid.
- Tart Cherry Extract: A concentrated form of the beneficial compounds in tart cherries.
- Omega-3 Fatty Acids: From fish oil or algae, for their anti-inflammatory effects.
- Always consult your doctor before starting any new supplements. They can interact with medications or be contraindicated for certain conditions.
- Medication Adherence: For many, diet and lifestyle changes are powerful, but medication (like allopurinol or febuxostat) is necessary to consistently keep uric acid levels in check. Work closely with your doctor to find the right treatment plan for you.
>
Part 5: Practical Tips for Navigating Your New Dietary Story
Implementing these changes can feel daunting, but remember, it’s a journey, not a sprint. Here are some practical tips to help you rewrite your gout story:
- Start Small, Build Momentum: Don’t overhaul your entire diet overnight. Choose one or two changes to implement each week. Maybe swap your sugary soda for water, or incorporate a serving of cherries daily.
- Meal Planning is Your Superpower: Plan your meals for the week. This reduces impulse eating, ensures you have gout-friendly ingredients on hand, and helps you stay on track.
- Read Labels Diligently: Become a detective. Look for hidden sugars (especially HFCS) and high sodium content in processed foods.
- Cook at Home More Often: This gives you complete control over your ingredients, allowing you to avoid problematic additives and excessive purines.
- Stay Hydrated, Always: Keep a water bottle with you and sip throughout the day.
- Embrace Variety: A diverse diet ensures you’re getting a wide array of nutrients and makes eating enjoyable.
- Track Your Triggers: Keep a food diary, especially if you’re experiencing flares. This can help you identify specific foods or patterns that might be triggering your attacks.
- Consult a Professional: A registered dietitian or nutritionist specializing in gout can provide personalized guidance and help you create a sustainable plan tailored to your needs.
- Educate Yourself Continuously: The science of nutrition is always evolving. Stay informed, but always cross-reference information with credible sources and medical professionals.
>
Conclusion: Your Plate, Your Power, Your Future
The story of gout doesn’t have to be one of perpetual pain and dietary fear. It can be a narrative of empowerment, understanding, and healing. By choosing to "Eat This, Not That," you’re not just restricting yourself; you’re actively nourishing your body, reducing inflammation, and giving your kidneys the support they need to manage uric acid effectively.
This ultimate gout food list is more than just a set of rules; it’s a philosophy. It’s about seeing food not as an enemy, but as medicine, as fuel, and as a source of joy. It’s about understanding the intricate dance between your metabolic health and the choices you make every day.
The journey to a gout-free life is personal, and it requires patience, consistency, and a willingness to learn. But with each conscious choice, each vibrant meal, and each glass of water, you are taking a powerful step towards reclaiming your comfort, your mobility, and your peace of mind. Your plate is your power. Use it wisely, and rewrite your story from one of suffering to one of vibrant health.