Hydration for Health: The Simple Gout Management Trick You Might Be Missing
The sharp, relentless agony of a gout flare is a torment that few who haven’t experienced it can truly comprehend. It’s not just a joint ache; it’s an inflammatory inferno, often striking with malicious intent in the dead of night, transforming the simplest touch, even the weight of a bedsheet, into an unbearable assault. For millions worldwide, this recurring nightmare dictates diet, limits activity, and casts a perpetual shadow of dread. Many embark on a quest for relief, meticulously tracking purine intake, adhering to prescribed medications, and exploring every dietary nuance, yet still find themselves ambushed by the familiar, debilitating pain. What if, amidst this complex tapestry of management strategies, one of the most fundamental and accessible tools for controlling gout has been consistently overlooked, deemed too simple to be truly effective? What if the answer, or at least a significant part of it, lies in the humble act of drinking more water?
Let me introduce you to Arthur. For over a decade, Arthur, a successful architect in his late fifties, had been locked in a bitter struggle with gout. His big toe, his knee, his ankle – they had all, at various times, become battlegrounds for the invisible crystals of monosodium urate. He’d tried everything. Allopurinol was a daily fixture, NSAIDs were his emergency rations, and colchicine his desperate plea for ceasefire during acute attacks. His diet had been meticulously overhauled: no more rich cuts of red meat, minimal seafood, beer was a distant memory. He’d lost weight, exercised moderately, and consulted specialists who confirmed his hyperuricemia was indeed the culprit. Yet, the flares persisted, albeit with reduced frequency, still disrupting his work, his hobbies, and his peace of mind. He felt perpetually on edge, waiting for the next attack, convinced he was doing everything right, but somehow still falling short.
One particularly severe flare landed Arthur in the emergency room. As the physician reviewed his history, labs, and current medications, she paused. "Arthur," she began, "we’ve covered diet, meds, weight… but tell me, how much water do you actually drink in a day?" Arthur shrugged. "Enough, I suppose. A few glasses, coffee in the morning, maybe some juice." The doctor nodded slowly. "Arthur, I want you to try something. For the next three months, before we consider any further medication adjustments, I want you to aim for at least three liters of plain water daily. Consistently. Spread throughout the day. And let’s see what happens."
Arthur was skeptical. Water? Could something so utterly basic, so universally preached for general health, hold the key to his complex, chronic condition? He’d always considered hydration a given, a background hum of health, not a targeted intervention for a specific, painful disease. But desperate for any sliver of hope, he decided to commit. This simple, seemingly innocuous piece of advice would, over the following months, begin to unravel a profound truth, not just for Arthur, but for countless others: adequate hydration is not merely good for you; it is a powerful, often overlooked, and undeniably simple strategy in the intricate dance of gout management.
Understanding Gout: The Enemy Within
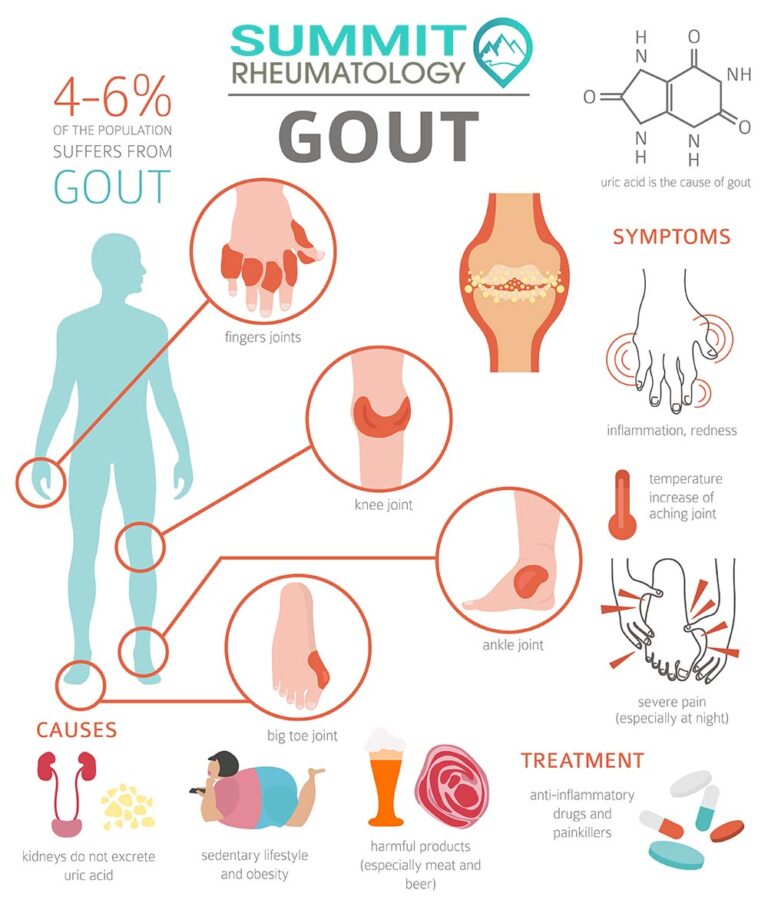
To appreciate the profound role of hydration, we must first truly understand the enemy. Gout is a complex metabolic disorder characterized by hyperuricemia – an abnormally high level of uric acid in the blood. Uric acid is a natural waste product of purine metabolism. Purines are organic compounds found in all living cells, including our own bodies and the foods we consume. When purines break down, they produce uric acid, which is then primarily filtered out by the kidneys and excreted in urine.
The problem arises when the body either produces too much uric acid (overproduction) or, more commonly, when the kidneys fail to excrete enough of it (underexcretion). When uric acid levels in the blood become excessively high, it can crystallize into needle-like monosodium urate crystals. These microscopic, sharp crystals often deposit in joints, particularly the big toe (podagra), but also ankles, knees, wrists, and fingers. Once these crystals form and are released into the joint space, they trigger a ferocious inflammatory response, attracting white blood cells that attempt to "clean up" the crystals, leading to the characteristic excruciating pain, swelling, redness, and heat of a gout flare.
Beyond acute flares, chronic hyperuricemia can lead to more insidious complications:
- Tophi: Hard, chalky deposits of urate crystals that can form under the skin, around joints, and in cartilage, causing disfigurement and joint damage.
- Kidney Stones: Uric acid crystals can also form stones in the urinary tract, leading to renal colic and potential kidney damage.
- Chronic Kidney Disease: Persistent hyperuricemia is a risk factor for the development and progression of chronic kidney disease.
- Cardiovascular Disease: Gout is increasingly recognized as a systemic inflammatory disease linked to a higher risk of heart attack, stroke, and other cardiovascular problems.
Traditional gout management focuses on two main pillars:
- Acute Flare Management: Using medications like Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), colchicine, and corticosteroids to reduce inflammation and pain during an attack.
- Urate-Lowering Therapy (ULT): Medications such as allopurinol and febuxostat aim to reduce the body’s production of uric acid, while probenecid helps the kidneys excrete more uric acid. These are crucial for long-term control and preventing crystal formation.
Dietary modifications are also vital, limiting high-purine foods (organ meats, certain seafoods, red meat), sugary drinks (especially those high in fructose), and alcohol (particularly beer and spirits). Weight management and regular exercise round out the conventional advice. Yet, even with diligent adherence to these strategies, many, like Arthur, find themselves grappling with persistent challenges. This is where the overlooked power of hydration steps onto the stage.
The Science of Hydration and Uric Acid Metabolism: A Deep Dive
The connection between hydration and uric acid metabolism is rooted in fundamental renal physiology. Our kidneys are master regulators of our body’s fluid and electrolyte balance, and they play a central role in filtering waste products from the blood, including uric acid.
1. The Kidney’s Role in Uric Acid Excretion:
Approximately two-thirds of the uric acid produced daily is excreted by the kidneys; the remaining third is eliminated through the gastrointestinal tract. In the kidneys, uric acid undergoes a complex process involving filtration, reabsorption, and secretion. Most uric acid is initially filtered from the blood by the glomeruli (tiny filtering units), but a significant portion is then reabsorbed back into the bloodstream by the renal tubules, and a smaller amount is subsequently secreted back into the urine. The balance of these processes determines the net amount of uric acid excreted. In individuals with gout, particularly those who are underexcreters (the majority), this balance is skewed, leading to insufficient uric acid removal.
2. The Concentration Effect: Dilution is the Solution:
This is perhaps the most straightforward and intuitive mechanism. When you are adequately hydrated, your body’s fluid volume is optimal. This translates to a larger volume of blood circulating through your kidneys, and consequently, a larger volume of urine produced. A larger volume of urine means that the uric acid being excreted is more diluted.
Think of it like dissolving sugar in water. If you try to dissolve a spoon of sugar in a tiny thimble of water, it will quickly become saturated and some sugar will remain undissolved, possibly crystallizing. But if you put that same spoon of sugar into a large glass of water, it will dissolve completely and remain in solution. The same principle applies to uric acid in your urine. Dehydration leads to concentrated urine, creating an environment where uric acid is less soluble and more likely to precipitate out of solution, forming crystals. These crystals are the precursors to both gout flares and uric acid kidney stones. By increasing fluid intake, you effectively increase the "volume of water" for the "sugar" (uric acid), keeping it dissolved and less prone to crystallization.
3. Maintaining Optimal Glomerular Filtration Rate (GFR) and Renal Blood Flow:
Adequate hydration is crucial for maintaining a healthy Glomerular Filtration Rate (GFR), which is the rate at which blood is filtered by the kidneys. GFR is a key indicator of kidney function. When you are dehydrated, your blood volume decreases, leading to a drop in blood pressure and reduced blood flow to the kidneys. This diminished blood flow directly impacts the GFR, making the kidneys less efficient at filtering waste products, including uric acid, from the blood.
By ensuring consistent hydration, you support optimal blood volume and pressure, which in turn ensures robust renal blood flow. This allows the kidneys to operate at peak efficiency, filtering and excreting uric acid effectively, preventing its accumulation in the bloodstream. It’s a foundational element for the kidneys to perform their essential excretory duties without undue stress.
4. Impact on Urine pH (A Secondary Mechanism):
While the primary mechanism of hydration for gout management is dilution and improved excretion, there’s a secondary, albeit less direct, effect on urine pH. Uric acid is a weak acid. Its solubility is significantly affected by the pH of the urine. In acidic urine (lower pH), uric acid is less soluble and more prone to crystallization. In more alkaline urine (higher pH), it is more soluble.
While plain water itself is generally neutral and doesn’t drastically alter urine pH, some fluids can have this effect. For instance, certain fruits and vegetables can contribute to a more alkaline urine pH. More importantly, severe dehydration can sometimes lead to a more acidic urine environment as the kidneys work to conserve water and concentrate other waste products. By maintaining good hydration, one helps the kidneys maintain a more balanced physiological environment, indirectly supporting uric acid solubility. However, it’s critical to note that direct urine alkalinization (e.g., with citrate supplements) is a specific medical intervention for certain conditions like uric acid kidney stones, and should only be pursued under medical guidance, as overly alkaline urine can also lead to other types of kidney stones. For gout management through hydration, the primary benefit remains dilution.
In essence, consistent and adequate hydration provides the kidneys with the necessary volume and flow to efficiently process and excrete uric acid, preventing its concentration and subsequent crystallization, both in the bloodstream and in the urinary tract. It’s a simple mechanical and physiological advantage that cannot be replicated by any medication alone.
Beyond Basic Thirst: The Nuances of Hydration for Gout
Arthur’s doctor didn’t just say "drink water"; she emphasized "at least three liters… consistently… spread throughout the day." This nuance is critical. Hydration for gout management isn’t just about quenching thirst; it’s a strategic, proactive intervention.
1. The Primacy of Plain Water:
While various beverages contribute to fluid intake, plain water remains the gold standard. It’s calorie-free, additive-free, and optimally absorbed. Filtered tap water, spring water, or mineral water – the type matters less than the consistent intake. It provides the pure solvent necessary for optimal kidney function without introducing other compounds that might interfere with uric acid metabolism.
2. Beneficial Adjunct Fluids (with Caution):
- Herbal Teas: Many herbal teas (e.g., green tea, ginger tea, peppermint tea) can be excellent, low-calorie, hydrating options. Some even offer anti-inflammatory properties.
- Diluted Fruit Juices (Highly Cautious): While fruit juices often contain fructose, which can elevate uric acid, highly diluted juices, particularly those from fruits with low fructose content and high vitamin C (like tart cherry juice, known for its anti-inflammatory properties, or diluted lemon water), can be acceptable in moderation. The key is dilution to minimize sugar intake and moderation.
- Vegetable Broths: Low-sodium vegetable broths can be hydrating and provide electrolytes and nutrients, especially beneficial during illness or hot weather.
- Low-Fat Milk: Some studies suggest that dairy products, particularly skim milk, may have a urate-lowering effect. It can be a good source of hydration and calcium.
3. Fluids to Limit or Avoid:
- Sugary Drinks: Sodas, fruit punches, and other sugar-sweetened beverages are notorious for their high fructose content. Fructose metabolism directly increases uric acid production, making these drinks highly detrimental for gout sufferers. Even "natural" fruit juices should be consumed with extreme caution and in very limited quantities due to their concentrated fructose.
- Alcohol: Alcohol, particularly beer and spirits, is a significant risk factor for gout flares. Alcohol metabolism increases uric acid production and reduces its renal excretion. While some studies suggest moderate wine consumption might have less impact, the safest approach for gout patients is often complete avoidance or severe limitation.
- High-Purine Broths: Broths made from meat (especially organ meats) can be high in purines and should be avoided.
- Caffeinated Beverages (in Excess): While moderate coffee intake has been linked to a lower risk of gout in some studies, excessive caffeine can have a mild diuretic effect. It’s not a primary source of hydration for the purposes of gout management.
4. Timing and Consistency are Key:
The "chugging" approach is less effective than consistent, sustained intake throughout the day. Spreading fluid intake helps maintain stable blood volume and urine dilution.
- Start the day with a large glass of water.
- Keep a water bottle handy and sip frequently.
- Drink water before meals to aid digestion and promote satiety.
- Drink water between meals.
- Don’t wait until you’re thirsty; thirst is often a sign you’re already mildly dehydrated.
- Adjust intake based on activity level, climate (hot weather, high altitude), and individual needs.
5. Monitoring Hydration Status:
While fluid intake goals are useful, observing your body’s signals is equally important.
- Urine Color: Pale yellow urine (like lemonade) indicates good hydration. Darker urine (like apple juice) suggests dehydration. Clear urine might indicate over-hydration, but this is less common with reasonable intake.
- Frequency of Urination: Being well-hydrated generally means more frequent trips to the bathroom.
- Thirst Cues: While an unreliable sole indicator, paying attention to thirst and addressing it promptly is important.
- Energy Levels: Dehydration can manifest as fatigue and lethargy.
6. Individual Needs and Medical Considerations:
It’s crucial to acknowledge that "three liters" is a general guideline. Individual fluid needs vary based on body size, activity level, climate, and overall health. Furthermore, certain medical conditions necessitate caution with increased fluid intake:
- Congestive Heart Failure: Individuals with CHF often have fluid restrictions to prevent fluid overload.
- Chronic Kidney Disease (Advanced Stages): As kidney function declines, fluid management becomes more complex, and excessive fluid can be harmful.
- Hyponatremia: In rare cases, excessive water intake without adequate electrolyte replacement can lead to dangerously low sodium levels.
Always consult with a healthcare professional to determine the appropriate fluid intake for your specific health profile, especially if you have underlying medical conditions. The goal is optimal, not excessive, hydration.
The "Story" Continues: Arthur’s Journey with Hydration
Back to Arthur. His initial skepticism about the "water trick" slowly began to erode as he committed to the doctor’s advice. He bought a large, insulated water bottle, made it his constant companion, and set reminders on his phone to drink every hour. The first few days were a struggle; he felt perpetually full and was making frequent trips to the restroom. But he persevered.
Within a couple of weeks, subtle changes emerged. He noticed his urine was consistently lighter in color. He felt a general sense of improved well-being, a slight lift in his energy levels that he hadn’t realized was missing. His usual afternoon slump began to diminish. More importantly, the niggling aches in his joints, which he had learned to live with as part of his "gout background noise," seemed to lessen.
The real breakthrough came after about two months. He realized he hadn’t had a full-blown flare. There had been a couple of fleeting moments of tenderness in his big toe, a ghost of an impending attack, but they had never escalated into the incapacitating pain he knew so well. Previously, even with his medication and dietary vigilance, he would experience a significant flare every 3-4 months. Now, the longest stretch of flare-free living in years was unfolding.
One weekend, Arthur made a slight misstep. Distracted by a family gathering, he forgot his water bottle, got caught up in conversations, and ended up drinking less than half his usual intake. The next morning, a familiar twinge in his ankle sent a jolt of anxiety through him. It wasn’t a full flare, but it was enough to remind him of the delicate balance he had achieved. He immediately resumed his diligent hydration, and the twinge subsided within a day. This experience cemented his belief: hydration wasn’t a placebo; it was a powerful, active player in his gout management.
Over the next year, Arthur’s life transformed. His flares became rare occurrences, and when they did strike, they were significantly milder and resolved faster, often without the need for potent NSAIDs. His uric acid levels, which had always hovered at the upper end of the target range despite allopurinol, showed a noticeable dip into a more optimal zone. He felt more in control, less anxious, and more confident in his ability to manage his condition. He rediscovered hobbies he had abandoned, like long walks and gardening, without the constant fear of a sudden attack. The "simple trick" had given him back a significant piece of his life.
Integrating Hydration into a Comprehensive Gout Management Plan
It is crucial to reiterate that hydration is not a standalone cure for gout. It is a powerful, foundational element of a comprehensive management strategy. Think of it as a critical supporting pillar, enhancing the efficacy of other interventions rather than replacing them.
For a knowledgeable audience, the integration looks like this:
- Medication Adherence: Continue to take all prescribed urate-lowering therapies (e.g., allopurinol, febuxostat) and acute flare medications (NSAIDs, colchicine) as directed by your physician. Hydration works synergistically with these drugs, potentially optimizing their effects and reducing the frequency/intensity of flares, thereby reducing reliance on acute medications.
- Dietary Modifications: Maintain a low-purine diet. This includes limiting red meat, organ meats, certain seafoods (sardines, anchovies, shellfish), and high-fructose corn syrup. Emphasize fruits, vegetables, whole grains, and low-fat dairy. Hydration helps process any dietary purines that are consumed.
- Weight Management: If overweight or obese, gradual weight loss can significantly improve gout outcomes. Rapid weight loss, however, can sometimes temporarily elevate uric acid, so it should be managed carefully with medical supervision. Hydration can support weight management by promoting satiety and boosting metabolism.
- Regular Exercise: Engage in regular, moderate physical activity. Exercise helps with weight management, improves overall metabolic health, and can reduce systemic inflammation. Ensure adequate hydration before, during, and after exercise, as fluid loss through sweat increases demands.
- Stress Management: Chronic stress can exacerbate inflammatory conditions. Incorporate stress-reduction techniques like meditation, yoga, or hobbies.
- Regular Medical Check-ups: Consistent monitoring of uric acid levels, kidney function, and overall health markers with your healthcare provider is essential. Discuss your hydration strategy with them to ensure it’s appropriate for your individual health status.
- Patient-Doctor Collaboration: View your healthcare provider as a partner. Be open about your lifestyle habits, including hydration, and work together to fine-tune your management plan.
By thoughtfully integrating optimal hydration into this multi-faceted approach, patients can significantly enhance their control over gout, reduce flare frequency and severity, and improve their overall quality of life.
Addressing Common Misconceptions and Challenges
Despite its simplicity, effective hydration often faces resistance or misunderstanding. A knowledgeable audience benefits from debunking these common pitfalls:
- "I drink coffee/soda/juice, that’s enough fluid." This is a critical misconception. Caffeinated beverages have a mild diuretic effect, meaning they can increase urine output and thus fluid loss. Sugary drinks, as discussed, are detrimental due to fructose content. While they contribute to fluid volume, they don’t offer the same pure, beneficial hydration as water, and often come with counterproductive ingredients.
- "I’ll just drink a lot when I feel a flare coming on." While increased hydration during a flare can help flush uric acid and potentially shorten its duration, the power of hydration lies in prevention. Consistent, daily intake maintains a diluted state, preventing crystal formation in the first place. Reactive hydration is far less effective than proactive, preventative hydration.
- "Water is boring." This is a common complaint. To combat this, one can infuse water with natural flavors: slices of cucumber, lemon, lime, berries, mint leaves, or ginger. Unsweetened sparkling water can also add variety. The key is to avoid added sugars or artificial sweeteners.
- "I have X condition, can I drink that much water?" As previously emphasized, individuals with certain medical conditions, especially congestive heart failure or advanced kidney disease, must consult their doctor before significantly increasing fluid intake. For most healthy individuals, three liters is a safe and beneficial target, but personalized advice is paramount.
- "It’s too much effort/inconvenient." Integrating consistent hydration requires a conscious shift in habit. Keeping a water bottle visible, setting reminders, and making hydration a non-negotiable part of the daily routine can help overcome this. The long-term benefits far outweigh the initial inconvenience.
- "Hydration is just a ‘detox’ fad." While many fad diets promote "detox" through water, the mechanism for gout is scientifically robust and rooted in renal physiology, not unsubstantiated claims. It’s about optimizing a known biological process, not a mystical cleanse.
The Future of Gout Management and the Enduring Role of Simple Habits
The field of gout management continues to evolve. New medications targeting different pathways of uric acid metabolism are being developed. Advanced diagnostics offer deeper insights into individual patient profiles. Genetic research promises personalized treatment strategies. Yet, amidst these sophisticated advancements, the foundational principles of health, including optimal hydration, will always remain relevant.
The story of gout management is often one of complexity – understanding purines, navigating medication side effects, managing comorbidities. It’s easy to overlook the elegantly simple solutions that lie within our daily reach. Hydration for gout is not a glamorous new drug; it’s an age-old physiological necessity, repurposed and highlighted as a targeted intervention. It empowers patients like Arthur to take an active, tangible role in their own health management, fostering a sense of control that can be profoundly therapeutic in itself.
The "simple trick" isn’t a magic bullet. It’s a consistent, disciplined habit that leverages the body’s natural mechanisms to combat a complex disease. It reminds us that sometimes, the most profound improvements in health don’t come from groundbreaking scientific discoveries, but from rediscovering and diligently applying the fundamental truths of our own biology.
Conclusion
Arthur’s journey is a testament to the transformative power of a seemingly minor adjustment. What began as a skeptical experiment, born of desperation, blossomed into a cornerstone of his gout management. His once-frequent, debilitating flares became rare whispers, and his anxiety about the next attack gave way to a renewed sense of confidence and well-being. He learned that the answer to a complex chronic condition doesn’t always lie in another pill or a more restrictive diet, but sometimes in the diligent application of the simplest, most accessible tools.
Optimal hydration, a mere act of drinking enough plain water, plays a critical, often underestimated, role in the management of gout. It supports the kidneys in their vital task of filtering uric acid, dilutes urine to prevent crystal formation, and maintains optimal bodily functions necessary for overall health. For the knowledgeable audience grappling with the nuances of gout, this is not just general health advice; it is a targeted, evidence-backed strategy.
If you are living with gout, take a moment to honestly assess your daily fluid intake. Are you truly providing your body, and specifically your kidneys, with the liquid volume they need to efficiently manage uric acid? Discuss this simple yet powerful strategy with your healthcare provider. It might just be the missing piece in your personal puzzle, the unsung hero in your fight against gout, offering you, like Arthur, a path to fewer flares, less pain, and a significantly improved quality of life. The most profound health improvements, after all, often stem from the simplest, most consistent habits. Don’t miss out on this one.