The Silent Saboteur: Gout in Women and the Unwritten Story of Misdiagnosis
The prevailing image of gout is often a caricature: a portly, middle-aged man, wincing in agony as his big toe throbs, a victim of overindulgence in rich foods and fine wines. This archetype, while sometimes accurate, casts a long, misleading shadow, obscuring a critical reality: gout affects women, often differently, and with alarming frequency, goes undiagnosed or misdiagnosed. For the knowledgeable audience, the story of gout in women isn’t just a footnote; it’s a compelling narrative of biological nuance, diagnostic bias, and the profound human cost of a medical blind spot. It’s a story that deserves to be told, understood, and ultimately, rewritten.
The Myth of the Male Domain: Unpacking the Historical Bias
For centuries, medical literature and popular culture alike have largely relegated gout to the male domain. Hippocrates himself dubbed it "the un걷able disease" and noted its rarity in women before menopause. This historical perspective, while rooted in some truth regarding incidence rates, has unfortunately fossilized into a clinical bias. When a woman presents with joint pain, particularly in her later years, the diagnostic radar often first pings for osteoarthritis, rheumatoid arthritis, fibromyalgia, or even carpal tunnel syndrome, before gout is even considered. This inherent predisposition, often unconscious, creates a formidable barrier to accurate diagnosis, pushing women down arduous, frustrating, and often ineffective treatment pathways for conditions they don’t have, while the true culprit continues its insidious work.
The story of gout in women begins not with the onset of symptoms, but with this ingrained preconception – a narrative already written, leaving little room for a divergent plotline.
Why the Script Changes: Biological Nuances in Women
The differences in gout presentation between men and women are not arbitrary; they are deeply rooted in fundamental biological distinctions, primarily hormonal and metabolic. Understanding these variances is the first step in dismantling the diagnostic bias.
The Estrogen Shield: A Double-Edged Sword
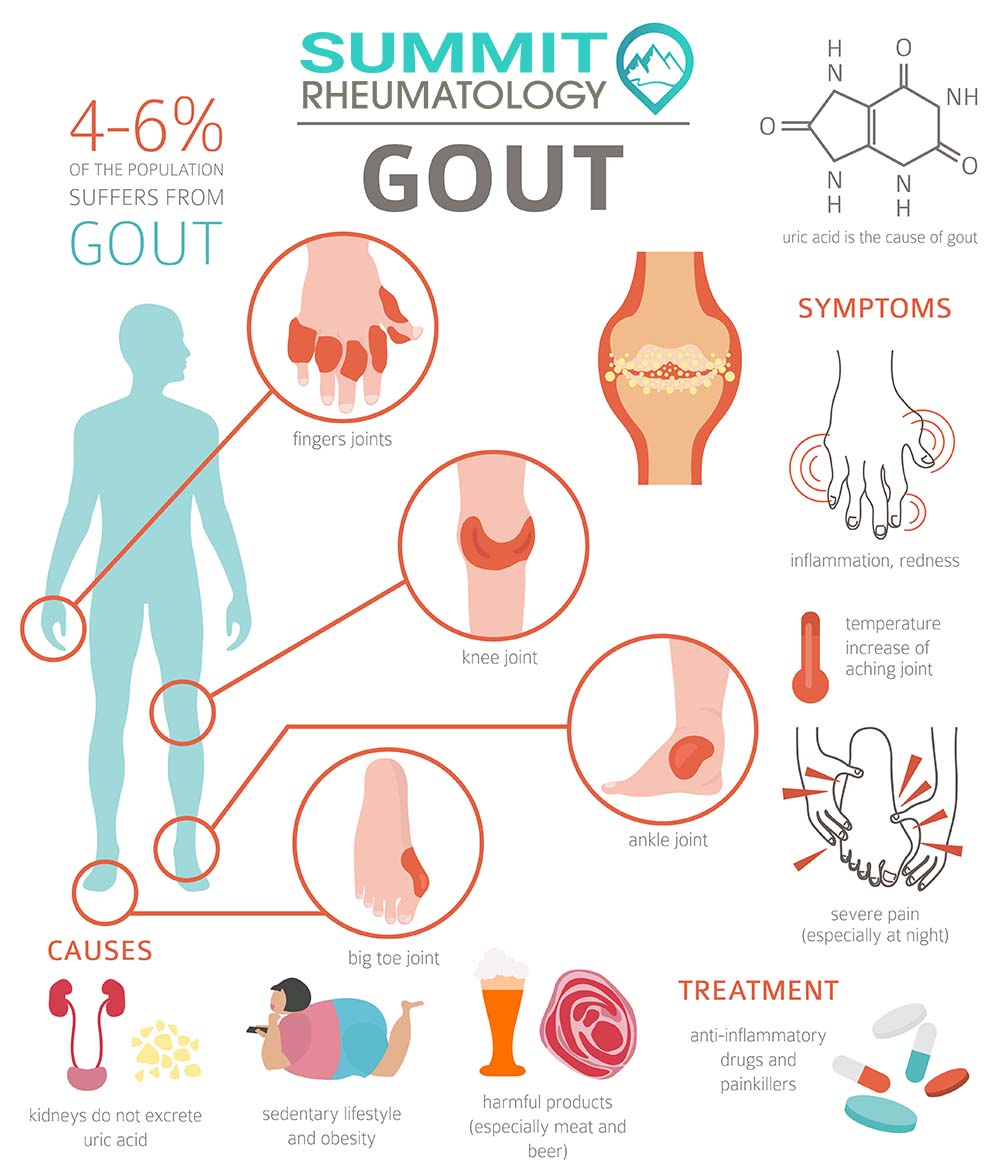
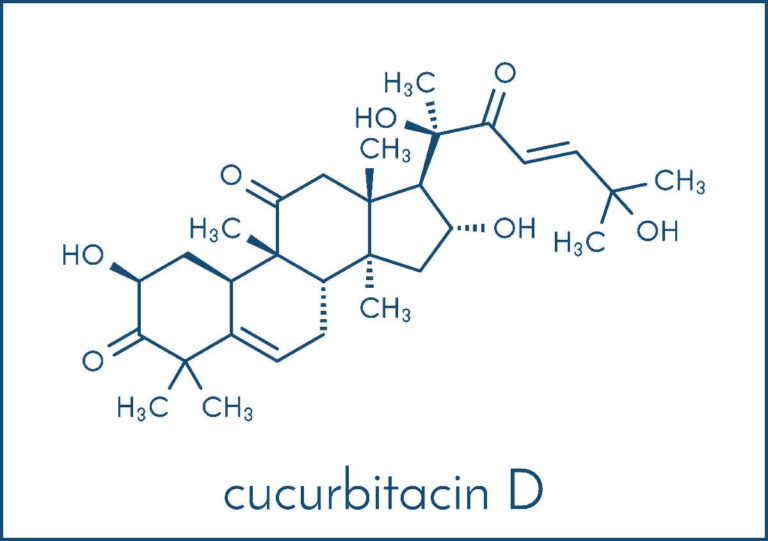
Estrogen plays a pivotal role in renal urate excretion, effectively acting as a natural uricosuric agent. By enhancing the kidneys’ ability to clear uric acid from the bloodstream, estrogen helps maintain lower serum urate levels in pre-menopausal women compared to age-matched men. This "estrogen shield" largely explains the significantly lower incidence of gout in younger women. It’s a protective mechanism, a biological advantage that delays the accumulation of uric acid crystals in the joints.
However, this shield is not impenetrable, nor is it permanent. As women approach and enter menopause, estrogen levels plummet. With this hormonal shift, the protective effect diminishes, and serum urate levels typically rise, often reaching or even exceeding those seen in men. This explains why gout in women is predominantly a post-menopausal phenomenon, with the average age of onset often a decade or more later than in men. The sudden loss of this natural uricosuric effect, combined with other age-related factors, sets the stage for hyperuricemia and subsequent gout attacks.
The Metabolic Tapestry: Comorbidities and Medications
Beyond hormones, women often present with a unique constellation of comorbidities and medication exposures that significantly influence their risk and presentation of gout.
- Hypertension and Diuretics: High blood pressure is more prevalent in post-menopausal women, and a common first-line treatment is thiazide diuretics (e.g., hydrochlorothiazide). These medications are notorious for increasing serum urate levels by impairing renal uric acid excretion. A woman being treated for hypertension may inadvertently be increasing her risk of gout, a critical piece of the puzzle often overlooked.
- Kidney Disease: Chronic kidney disease (CKD) is a significant risk factor for gout in both sexes, but its prevalence and management can differ. Impaired renal function directly reduces the body’s ability to excrete uric acid, leading to hyperuricemia.
- Obesity and Metabolic Syndrome: While not exclusive to women, the prevalence of obesity and metabolic syndrome continues to rise, contributing to insulin resistance, which can impair renal urate excretion.
- Hypothyroidism: An often-underestimated risk factor, hypothyroidism can slow metabolism and affect kidney function, potentially leading to elevated urate levels.
- Psoriasis: Women with psoriasis are at an increased risk of gout, and the joint pain can easily be attributed solely to psoriatic arthritis, masking the underlying gout.
- Aspirin (Low-Dose): While high-dose aspirin is uricosuric, low-dose aspirin, commonly prescribed for cardiovascular protection, can paradoxically impair renal uric acid excretion, contributing to hyperuricemia.
These interwoven medical conditions and their pharmacological treatments create a complex metabolic landscape in women, subtly but significantly increasing their susceptibility to gout, often under the radar of both patient and physician.
The Chameleon Disease: When Symptoms Don’t Fit the Mold
Perhaps the most compelling reason gout is missed in women lies in its atypical presentation. The classic "podagra" – excruciating pain in the big toe – is far less common as the initial presentation in women. Instead, gout in women often acts like a chameleon, mimicking other conditions and defying the expected script.
Polyarticular vs. Monoarticular Onset
While men typically experience monoarticular (affecting one joint) attacks, particularly in the big toe, women are significantly more likely to present with polyarticular (affecting multiple joints) gout. This widespread joint involvement can easily be confused with rheumatoid arthritis (RA) or osteoarthritis (OA), especially given the age of onset. The insidious nature of polyarticular flares, often less explosively acute than the classic male presentation, further blurs the diagnostic lines.
Atypical Joint Locations
Forget the big toe. In women, gout frequently targets:
- Fingers and Wrists: The small joints of the hands and wrists are common sites, leading to misdiagnosis as OA of the hands, rheumatoid arthritis, or even carpal tunnel syndrome. The stiffness and swelling can be chronic, lacking the dramatic acute flare often associated with gout.
- Knees and Ankles: While not entirely atypical, the knee can be a frequent target, again leading to confusion with OA or other forms of inflammatory arthritis.
- Elbows and Shoulders: Less common but still observed, especially in polyarticular presentations.
This predilection for upper extremity involvement, coupled with the polyarticular nature, makes the clinical picture deviate significantly from the male archetype, contributing to diagnostic delays.
The "Less Severe" Flare – A Deceptive Calm
Women’s gout flares are often described as less intensely acute than men’s. While still painful, they may lack the sudden, explosive onset and excruciating, "cannot-bear-a-sheet-on-it" severity that characterizes classic podagra. Instead, flares might be more protracted, smoldering, and characterized by persistent stiffness, aching, and swelling. This less dramatic presentation can lead both patients and physicians to underestimate the severity of the condition, delaying investigation for gout. The "less severe" flare is a deceptive calm, masking ongoing crystal deposition and joint damage.
Tophi: A Later, More Subtle Appearance
Tophi – visible deposits of uric acid crystals under the skin – are a hallmark of chronic, uncontrolled gout. While they eventually appear in women, they tend to develop later in the disease course and in different locations. In women, tophi might be found in:
- Finger joints: Mimicking Heberden’s or Bouchard’s nodes associated with OA.
- Ear helices: Often small and mistaken for benign skin lesions.
- Olecrana bursa (elbow): Resembling bursitis.
- Achilles tendons: Confused with tendinitis.
Their insidious onset and atypical locations mean tophi in women are often overlooked or misidentified, further delaying a correct diagnosis.
The Diagnostic Labyrinth: Why Gout is Missed
The unique biological and symptomatic profile of gout in women creates a complex diagnostic labyrinth.
The Physician’s Blind Spot: Cognitive Bias
Despite increasing awareness, cognitive bias remains a formidable challenge. When a woman, particularly post-menopausal, presents with polyarticular pain and swelling, the diagnostic algorithm in many clinicians’ minds still defaults to more common female-predominant conditions like OA or RA. Gout, being "atypical" in this demographic, may not even enter the differential diagnosis until considerable time has passed. This diagnostic inertia can lead to years of unnecessary suffering and joint damage.
Patient-Delayed Presentation
Women themselves, often conditioned by societal expectations to "power through" pain or attribute it to aging, may also delay seeking medical attention. When they do, if their symptoms don’t fit the "classic" male picture of gout, they may not advocate strongly for a gout workup, particularly if their doctor is steering them towards other diagnoses.
Diagnostic Challenges: The Elusive Crystal
Even when gout is suspected, confirming the diagnosis can be challenging.
- Normal Serum Urate During a Flare: A significant hurdle is that serum uric acid levels can be normal, or even low, during an acute gout flare. This is because the body’s inflammatory response can temporarily shift uric acid from the bloodstream into the joints, or increase renal excretion. A single blood test showing "normal" uric acid during an acute flare can falsely reassure a physician and lead them away from a gout diagnosis. Serial testing or testing outside of an acute flare is crucial.
- Difficulty with Synovial Fluid Aspiration: The gold standard for gout diagnosis is the identification of negatively birefringent monosodium urate (MSU) crystals in synovial fluid, usually obtained via joint aspiration. However, aspiring small joints (like those in the fingers or wrists) can be technically challenging. Furthermore, if the flare is less acute or polyarticular, there may be less effusive fluid to aspirate. The procedure itself may also be deferred if the initial suspicion of gout is low, due to the atypical presentation.
- Mimicry of Other Conditions: The very symptoms that characterize gout in women (polyarticular, finger/wrist involvement, chronic stiffness) are also hallmarks of rheumatoid arthritis and osteoarthritis. Differentiating these conditions requires careful clinical acumen, specific lab tests (rheumatoid factor, anti-CCP antibodies for RA), and often imaging. However, a woman can have both OA and gout, or even RA and gout, further complicating the diagnostic picture.
The Human Cost: Consequences of Missed Diagnosis
The failure to diagnose gout in women has far-reaching and devastating consequences, extending beyond mere joint pain.
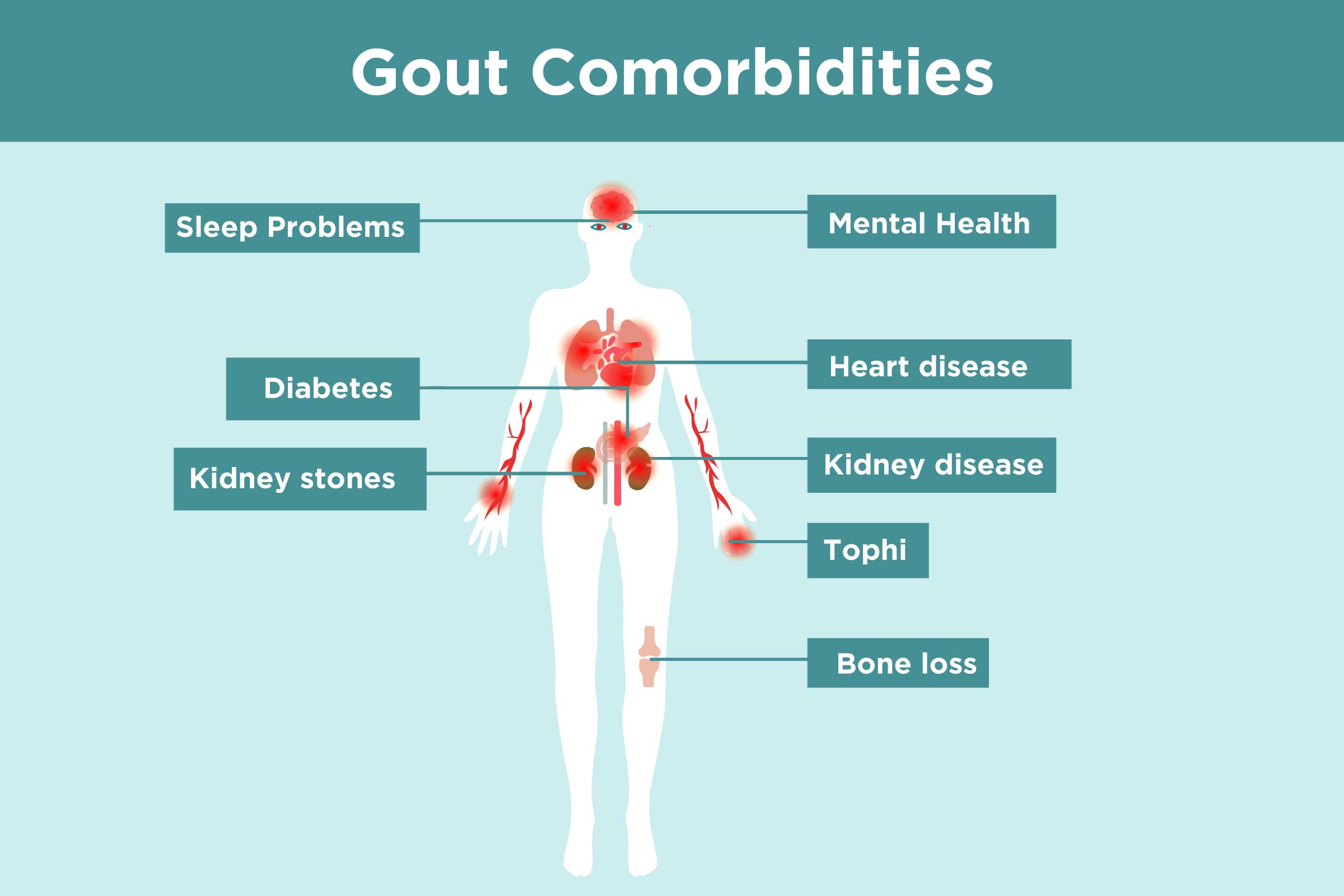
- Progressive Joint Damage: Uncontrolled hyperuricemia leads to chronic crystal deposition, causing irreversible damage to cartilage and bone. This can result in chronic arthritis, deformity, and significant functional impairment, impacting daily activities and quality of life. The delay in diagnosis means this damage progresses unchecked for years.
- Impaired Quality of Life: Persistent pain, stiffness, and limited mobility lead to reduced physical activity, social isolation, sleep disturbances, and a significant decline in overall well-being. The frustration of being misdiagnosed or dismissed adds a psychological burden.
- Increased Cardiovascular Risk: Gout is not just a joint disease; it’s a systemic inflammatory condition associated with an increased risk of cardiovascular disease (heart attack, stroke), kidney disease, and metabolic syndrome. Untreated gout means these systemic risks also remain unaddressed, contributing to higher morbidity and mortality.
- Kidney Stones and Renal Impairment: Chronic hyperuricemia increases the risk of uric acid kidney stones and can contribute to progressive kidney damage (urate nephropathy).
- Psychological Impact: Living with chronic, undiagnosed pain can lead to anxiety, depression, and a sense of invalidation. The repeated cycles of misdiagnosis and ineffective treatments erode trust in the medical system and can leave women feeling helpless and unheard.
Rewriting the Narrative: A Path to Better Diagnosis and Management
The story of gout in women doesn’t have to end in missed diagnoses and progressive suffering. A concerted effort from both healthcare providers and patients can rewrite this narrative.
For Healthcare Providers: Cultivating a High Index of Suspicion
- Challenge the Archetype: Actively question the traditional "male gout" stereotype. When a post-menopausal woman presents with polyarticular arthritis, particularly in the hands, wrists, or knees, always include gout in the differential diagnosis.
- Thorough History Taking: Inquire about specific risk factors in women: menopausal status, diuretic use, history of hypertension, kidney disease, psoriasis, and any family history of gout.
- Beyond Serum Urate: Understand the limitations of a single serum uric acid measurement, especially during a flare. Consider serial measurements and interpreting levels in the context of symptoms and comorbidities.
- Embrace Imaging: Musculoskeletal ultrasound is increasingly valuable in diagnosing gout. It can detect early crystal deposits (the "double contour sign") and tophi even before they are clinically apparent, and it can differentiate gout from other arthropathies. Dual-energy CT (DECT) can also identify urate crystal deposits.
- The Gold Standard: When feasible, perform synovial fluid aspiration. Even if fluid is scant, the effort to confirm MSU crystals is paramount for an accurate diagnosis.
- Interdisciplinary Approach: Collaborate with rheumatologists, nephrologists, and primary care physicians to manage complex cases, especially those with significant comorbidities.
For Women: Becoming Your Own Advocate
- Be Informed: Understand that gout is not just a "man’s disease" and that your symptoms may differ from the classic description.
- Document Your Symptoms: Keep a detailed journal of your pain, swelling, affected joints, duration of flares, and any associated factors. This can provide crucial information to your doctor.
- Share Your Full Medical History: Don’t omit details about medications (especially diuretics), family history, or other medical conditions, even if they seem unrelated to your joint pain.
- Ask Questions and Persist: If your symptoms don’t improve with initial treatments, or if you feel your concerns are being dismissed, don’t hesitate to ask about gout. Request a referral to a rheumatologist if your primary care physician seems unsure or unwilling to investigate further.
- Understand Diagnostic Tests: If your doctor orders a serum uric acid test, ask if they will consider follow-up tests if the initial one is normal but symptoms persist, or if a joint aspiration is appropriate.
Management Considerations for Women
Once diagnosed, managing gout in women requires specific considerations:
- Urate-Lowering Therapy (ULT): Allopurinol and febuxostat are first-line ULTs. The choice and dosing should consider renal function, potential drug interactions (especially with diuretics), and individual patient factors.
- Acute Flare Management: NSAIDs, colchicine, and corticosteroids are used for acute flares, with careful consideration of comorbidities (e.g., kidney disease, heart failure, osteoporosis risk with steroids).
- Lifestyle Modifications: Dietary advice (reducing purine-rich foods, sugary drinks, alcohol), weight management, and adequate hydration are crucial, though often less impactful than ULT.
- Bone Health: Given the post-menopausal age of onset, bone mineral density should be monitored, as chronic inflammation from gout and certain medications can impact bone health.
- Cardiovascular Risk Management: Proactive management of hypertension, dyslipidemia, and diabetes is essential, as gout is an independent risk factor for cardiovascular disease.
Conclusion: A Call for Recognition and Empathy
The story of gout in women is a poignant reminder of how deeply ingrained medical stereotypes can impact diagnosis and patient care. It is a narrative of biological complexity, where hormonal shifts and metabolic nuances create a different clinical picture, often leading to misinterpretation. It’s a story of a "silent saboteur" that works subtly, causing insidious damage while masquerading as more common conditions.
By recognizing the unique ways gout manifests in women – its polyarticular nature, atypical joint involvement, later onset, and association with specific comorbidities and medications – healthcare providers can dismantle the diagnostic bias. By empowering women to advocate for themselves, armed with knowledge about their distinct presentation, we can bridge the gap between symptom and diagnosis.
The goal is not just to identify a disease, but to alleviate suffering, prevent irreversible joint damage, and mitigate systemic health risks. It’s time to retire the outdated caricature and embrace the full, nuanced, and often overlooked story of gout in women – a story that, with proper recognition and empathy, can finally have a healthier ending.