The Diagnostic Journey: What to Expect When Testing for Rheumatoid Arthritis
The journey to a diagnosis of rheumatoid arthritis (RA) is rarely a straight line. It’s often a winding path, fraught with uncertainty, dotted with anxious waits, and illuminated by moments of clarity. For those experiencing the initial whispers of discomfort – the morning stiffness, the tender joints, the pervasive fatigue – the quest for answers can be as challenging as the disease itself. This article aims to tell the story of that diagnostic journey, offering a comprehensive guide to what a knowledgeable patient can expect, from the first subtle symptoms to the ultimate confirmation of RA.
Chapter 1: The First Whispers – Recognizing the Unfamiliar
The story of RA often begins subtly, with symptoms that are easy to dismiss or attribute to other, less serious causes. It’s not a sudden, dramatic onset in most cases, but rather a slow creep, a series of seemingly unrelated aches and pains that gradually coalesce into a disturbing pattern.
Early Symptoms: More Than Just "Getting Old"
Many people initially rationalize their symptoms. A stiff finger? Perhaps a minor sprain. A persistent fatigue? Must be stress or lack of sleep. But for those developing RA, these seemingly innocuous signs persist and often worsen, becoming increasingly difficult to ignore.
- Morning Stiffness: This is one of the hallmarks of RA. Unlike the brief stiffness of osteoarthritis that eases quickly with movement, RA-related morning stiffness can last for 30 minutes, an hour, or even several hours. It’s a systemic, inflammatory stiffness that locks joints in place, making simple tasks like opening a jar or gripping a toothbrush incredibly difficult.
- Symmetrical Joint Pain and Swelling: While RA can affect any joint, it commonly targets the small joints of the hands and feet (metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints, and metatarsophalangeal (MTP) joints). Crucially, this often occurs symmetrically – if one wrist is affected, the other usually is too. The pain is often described as a deep ache, a throbbing sensation, or a persistent tenderness. Swelling, though sometimes subtle at first, indicates inflammation.
- Fatigue: This isn’t just ordinary tiredness; it’s a profound, debilitating exhaustion that sleep doesn’t alleviate. It can precede joint symptoms by weeks or months and is a direct result of the systemic inflammation ravaging the body.
- Low-Grade Fever and General Malaise: Some individuals experience a general feeling of being unwell, similar to having a mild flu, sometimes accompanied by a persistent low-grade fever. This reflects the body’s inflammatory response.
- Loss of Appetite and Weight Loss: Systemic inflammation can also lead to a decrease in appetite, sometimes resulting in unintentional weight loss.
Recognizing these patterns is the first, crucial step. It’s the moment when one transitions from casually dismissing symptoms to acknowledging that something is genuinely amiss and warrants medical attention. This self-awareness is the catalyst for the entire diagnostic journey.
Chapter 2: The Primary Care Physician – The First Point of Contact
Once the decision is made to seek medical advice, the primary care physician (PCP) or general practitioner (GP) is typically the first port of call. This visit is critical, as the PCP acts as a gatekeeper, performing an initial assessment and determining the need for specialist referral.
What to Expect at the First Visit:
Come prepared. The more information you can provide, the more effective your PCP can be.
-
Detailed History Taking:
- Symptom Onset and Progression: When did the symptoms start? How have they changed over time? Are they constant or intermittent?
- Affected Joints: Which joints are painful or swollen? Is it symmetrical?
- Morning Stiffness Duration: Be specific about how long it lasts.
- Other Systemic Symptoms: Fatigue, fever, weight loss, night sweats, skin rashes, dry eyes/mouth (secondary Sjögren’s syndrome is common with RA).
- Family History: Does anyone in your family have RA or other autoimmune diseases (e.g., lupus, psoriasis, thyroid disorders)? This is a significant piece of the puzzle.
- Medications and Lifestyle: Current medications, recent infections, travel history, smoking status (a known risk factor for RA).
-
Physical Examination:
- Joint Assessment: The PCP will carefully examine your joints, looking for swelling, tenderness, warmth, and assessing your range of motion. They’ll often palpate the small joints of your hands and feet.
- General Assessment: Checking for other signs like skin changes, rashes, or enlarged lymph nodes.
-
Initial Blood Tests (Screening):
- Complete Blood Count (CBC): To check for anemia (common in chronic inflammatory conditions) and evaluate white blood cell counts.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These are non-specific inflammatory markers. Elevated levels indicate inflammation somewhere in the body, but don’t pinpoint RA specifically. They serve as general indicators of disease activity.
- Thyroid Function Tests: To rule out thyroid disorders, which can mimic some RA symptoms like fatigue and joint pain.
The Differential Diagnosis: More Than Just RA
A crucial aspect of the PCP’s role is considering the "differential diagnosis." Many conditions can cause joint pain and fatigue. The PCP will be thinking about possibilities like:
- Osteoarthritis (OA): Typically affects larger, weight-bearing joints, is asymmetrical, and stiffness is usually shorter-lived (less than 30 minutes) and worsens with activity, not rest.
- Psoriatic Arthritis (PsA): Often associated with psoriasis, can be symmetrical or asymmetrical, and can affect the spine.
- Lupus (Systemic Lupus Erythematosus – SLE): Can cause widespread joint pain, fatigue, and other systemic symptoms, often with distinct skin manifestations.
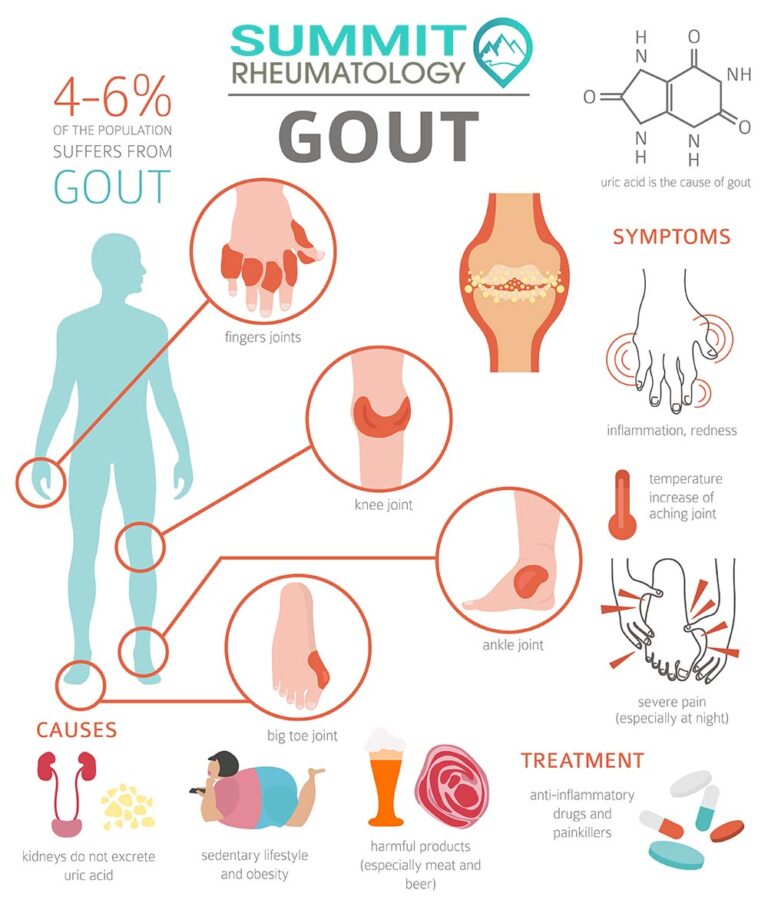
- Gout/Pseudogout: Characterized by acute, severe attacks of joint pain, usually in one joint, caused by crystal deposits.
- Viral Infections: Parvovirus B19, hepatitis, and others can cause temporary joint pain.
- Fibromyalgia: Widespread pain, fatigue, and tender points, but without joint inflammation.
Based on the initial assessment, if RA is suspected, the next critical step is a referral to a specialist.
Chapter 3: The Rheumatologist – The Specialist’s Lens
The rheumatologist is the expert in inflammatory joint diseases and autoimmune conditions. Their involvement marks a significant progression in the diagnostic journey, bringing a higher level of specialized knowledge and diagnostic tools to bear.
The Rheumatologist’s Comprehensive Assessment:
The rheumatologist’s evaluation will be far more in-depth than the PCP’s, focusing specifically on the nuances of inflammatory arthritis.
-
Revisiting the History (with a Finer Comb):
- They will delve deeper into the character of your pain, the specific joints affected, the pattern of stiffness, and the impact on your daily life.
- They’ll inquire about "extra-articular" symptoms – those outside the joints – such as skin nodules (rheumatoid nodules), dry eyes/mouth, chest pain (pleurisy/pericarditis), or numbness/tingling (nerve involvement).
- They will meticulously review your family history of autoimmune diseases, recognizing genetic predispositions.
-
The Expert Physical Examination:
- Palpation of Synovitis: The rheumatologist is highly skilled at detecting subtle signs of synovitis (inflammation of the synovial membrane lining the joints). They will systematically palpate joints, looking for the characteristic "boggy" or spongy feel of inflamed synovium, warmth, and tenderness. They’ll also assess the symmetry of involvement.
- Range of Motion: Evaluating the flexibility and function of your joints.
- Deformities: Looking for any early signs of joint damage or deformity, though these are typically seen in later stages of untreated disease.
- Overall Musculoskeletal Assessment: Assessing muscle strength, gait, and posture.
-
Advanced Diagnostic Tests – The Core of RA Diagnosis:
This is where the "detective work" truly intensifies. No single test diagnoses RA; it’s a mosaic of clinical presentation, blood work, and imaging.
A. Blood Tests (Serology and Inflammation Markers):
These tests are crucial for identifying specific antibodies and markers of inflammation associated with RA.
-
Rheumatoid Factor (RF):
- What it is: An autoantibody (an antibody that mistakenly targets the body’s own tissues) that is present in about 70-80% of people with RA. It’s usually an IgM antibody against the Fc region of IgG.
- Significance: A positive RF can strongly suggest RA, particularly in the right clinical context. However, it’s not exclusive to RA.
- Caveats:
- False Positives: RF can be positive in other autoimmune diseases (e.g., Sjögren’s syndrome, lupus), chronic infections (e.g., hepatitis C, tuberculosis), and even in a small percentage of healthy individuals, especially as they age.
- False Negatives: Approximately 20-30% of RA patients are "seronegative," meaning their RF test is negative despite having RA. This is why other tests are vital.
-
Anti-Cyclic Citrullinated Peptide (Anti-CCP) Antibodies:
- What it is: Another autoantibody that targets citrullinated proteins. Citrullination is a post-translational modification of proteins that can occur during inflammation, and the immune system in RA patients often reacts to these modified proteins.
- Significance: Anti-CCP is highly specific for RA (around 95-98%). It’s often positive earlier in the disease course than RF and is a strong predictor of more erosive (joint-damaging) disease.
- Caveats: While highly specific, it’s not 100% sensitive (meaning some RA patients will be negative for anti-CCP).
-
Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP):
- What they are: These are acute-phase reactants, meaning their levels rise in response to inflammation. ESR measures how quickly red blood cells settle in a test tube, while CRP is a protein produced by the liver during inflammation.
- Significance: Elevated ESR and CRP levels indicate active inflammation and are often used to monitor disease activity and response to treatment.
- Caveats: They are non-specific. Many other conditions (infections, other inflammatory diseases, trauma) can cause elevated ESR and CRP. A normal ESR/CRP does not rule out RA, especially in early stages.
-
Antinuclear Antibodies (ANA):
- What it is: A broad screening test for systemic autoimmune diseases. ANAs target components within the nucleus of a cell.
- Significance: While frequently positive in lupus, ANAs can also be positive in about 30-40% of RA patients.
- Caveats: A positive ANA is not diagnostic for RA on its own and requires further investigation. Many healthy individuals can have a low-titer positive ANA.
-
Other Blood Tests: Your rheumatologist might also order tests like liver and kidney function tests (important before starting certain medications), and sometimes hepatitis or HIV screens (as these can sometimes mimic RA or impact treatment choices).
B. Imaging Studies: Visualizing the Damage and Inflammation:
Imaging helps visualize the state of the joints, detecting inflammation, and assessing for damage that might not be apparent on physical examination.
-
X-rays:
- Purpose: Primarily used to establish a baseline and detect joint damage (erosions, joint space narrowing) that occurs in later stages of RA.
- Significance: In early RA, X-rays are often normal, as erosions take time to develop. However, they are essential for monitoring disease progression and distinguishing RA from other forms of arthritis.
- What to expect: Usually involves X-rays of the hands, wrists, and feet, as these are commonly affected.
-
Musculoskeletal Ultrasound:
- Purpose: A highly sensitive tool for detecting early inflammatory changes in the joints that X-rays might miss. It can visualize synovitis, tenosynovitis (inflammation of tendon sheaths), and even subtle bone erosions.
- Significance: Ultrasound can detect inflammation before it’s clinically apparent and can guide injections. It’s becoming increasingly important in early RA diagnosis and monitoring.
- What to expect: A gel is applied to the skin over the joint, and a transducer is moved over the area, displaying real-time images. It’s painless and non-invasive.
-
Magnetic Resonance Imaging (MRI):
- Purpose: The most sensitive imaging modality for detecting early inflammatory changes, including synovitis, bone marrow edema (a precursor to erosion), and cartilage damage.
- Significance: MRI can detect changes within weeks to months of symptom onset, providing crucial information for early diagnosis and intervention.
- What to expect: You’ll lie still in a scanner. It’s a longer procedure than an X-ray or ultrasound, and some people find the enclosed space and noise uncomfortable. Contrast dye may be used to highlight inflammation.
Chapter 4: The Nuance of Diagnosis – Piecing Together the Puzzle
The journey to an RA diagnosis is akin to solving a complex puzzle. There’s no single "RA test" that definitively gives a yes or no answer. Instead, the rheumatologist meticulously combines all the information gathered – clinical symptoms, physical examination findings, blood test results, and imaging – to meet established diagnostic criteria.
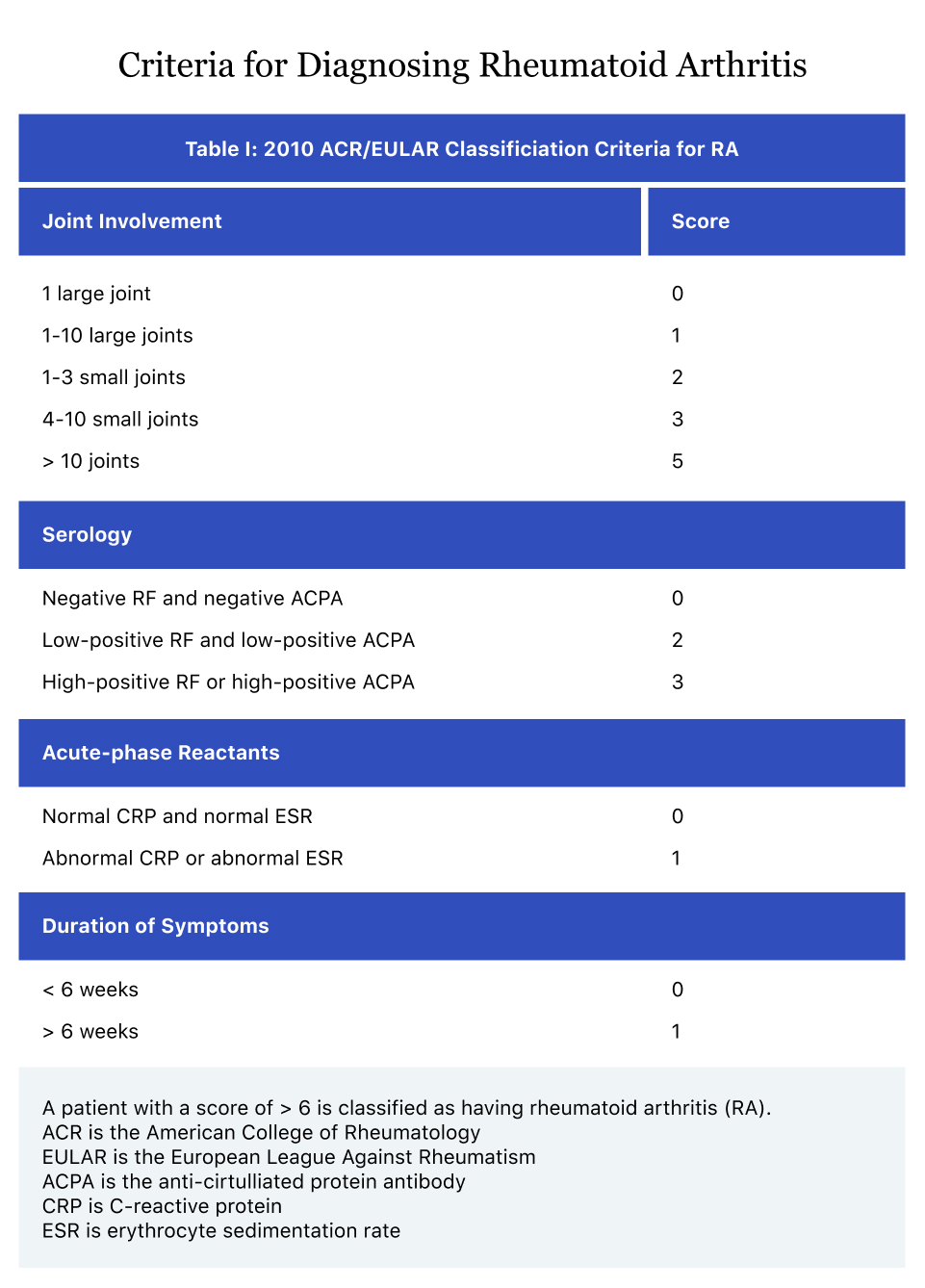
The Classification Criteria (ACR/EULAR):
Rheumatologists use classification criteria, such as those developed by the American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR), to help standardize diagnosis. These criteria assign points based on:
- Joint Involvement: The number and type of joints affected (small vs. large, symmetrical).
- Serology: Positive or high-positive RF or Anti-CCP.
- Acute Phase Reactants: Elevated ESR or CRP.
- Duration of Symptoms: Symptoms lasting for at least six weeks.
A certain score (e.g., 6 out of 10) indicates a definite diagnosis of RA. It’s important to remember these are classification criteria, not absolute diagnostic criteria, especially in early or atypical cases. The rheumatologist’s clinical judgment always plays a paramount role.
Challenges in Diagnosis:
- Early RA: In the very early stages, symptoms might be mild, and blood tests or imaging might not yet show clear signs. This is a period of "undifferentiated arthritis," where close monitoring is essential.
- Seronegative RA: As mentioned, 20-30% of RA patients test negative for RF and Anti-CCP. Diagnosing seronegative RA relies more heavily on clinical presentation, physical findings, elevated inflammatory markers, and imaging evidence of inflammation. This can be particularly frustrating for patients who feel their symptoms aren’t being fully validated by lab tests.
- Overlapping Conditions: Sometimes, symptoms might overlap with other autoimmune diseases, making a clear distinction challenging. For example, some individuals may have features of both RA and lupus.
- Mimics: Conditions like osteoarthritis, viral arthritis, or even certain cancers can initially present with joint pain, requiring careful exclusion.
The "Wait and See" Period:
Sometimes, after the initial battery of tests, the diagnosis isn’t immediately clear. The rheumatologist might recommend a "wait and see" approach, scheduling follow-up appointments to monitor symptom progression, repeat blood tests, or order further imaging. This period can be emotionally taxing, a limbo between uncertainty and a definitive answer. It’s during this time that patient advocacy becomes even more crucial: keeping detailed symptom diaries, noting changes, and asking questions.
Chapter 5: The Emotional Landscape of Diagnosis
Beyond the medical procedures and scientific data, the diagnostic journey for RA is profoundly emotional. It’s a narrative woven with fear, frustration, hope, and ultimately, a form of acceptance.
The Burden of Uncertainty:
From the first twinges of pain, the unknown casts a long shadow. Is it serious? Will it go away? The period leading up to the first doctor’s visit is often characterized by anxiety and self-doubt. Once the medical process begins, the waiting game for test results, the possibility of a "negative" test despite debilitating symptoms, and the iterative nature of diagnosis can be incredibly draining. Patients often report feeling dismissed, or that their pain isn’t being taken seriously, especially if initial tests are inconclusive.
The Impact of a Chronic Disease:
Receiving an RA diagnosis is often a watershed moment. While it can bring a sense of validation and relief ("finally, I know what’s wrong!"), it also ushers in a new set of anxieties:
- Fear of the Future: What will this mean for my quality of life? Will I become disabled? How will it affect my work, my family, my hobbies?
- Grief: Grieving the loss of a perceived healthy future, the activities one once enjoyed effortlessly, or simply the person one was before the disease.
- Adjustment: Learning to live with a chronic condition that requires ongoing management, medication, and lifestyle adjustments.
Finding Support and Empowerment:
Crucially, patients are not alone in this journey.
- Support Systems: Leaning on family, friends, and support groups (online or in-person) can provide immense emotional relief and practical advice.
- Patient Education: Understanding RA – its mechanisms, treatments, and prognosis – empowers patients to become active participants in their care.
- Advocacy: Learning to advocate for oneself, asking clarifying questions, seeking second opinions, and maintaining detailed medical records are essential. Your voice is the most important in your care team.
Chapter 6: Post-Diagnosis – The Path Forward
Once a definitive diagnosis of RA is made, the narrative shifts from diagnosis to management. This is not an endpoint but a new beginning, focused on controlling inflammation, preventing joint damage, and maintaining quality of life.
Immediate Next Steps:
- Treatment Plan: The rheumatologist will discuss treatment options, typically involving disease-modifying antirheumatic drugs (DMARDs) – often methotrexate as a first line – and potentially biologics or targeted synthetic DMARDs. Corticosteroids or NSAIDs may be used for symptom relief during initial phases.
- Patient Education: Understanding your medications, potential side effects, and the importance of adherence is vital.
- Lifestyle Modifications: Diet, exercise, stress management, and smoking cessation play significant roles in managing RA.
- Regular Monitoring: Frequent follow-up appointments will be scheduled to assess disease activity, monitor treatment effectiveness, and check for side effects. Blood tests (ESR, CRP, liver/kidney function) will be regularly repeated.
- Multidisciplinary Care: You may be referred to other healthcare professionals, such as a physical therapist (to maintain joint flexibility and strength), an occupational therapist (to adapt daily tasks and protect joints), or a podiatrist.
The Importance of Early Diagnosis and Treatment:
The story of RA diagnosis underscores the critical importance of early intervention. The "window of opportunity" for effective treatment is often within the first few months of symptom onset. Delaying diagnosis and treatment can lead to irreversible joint damage, increased disability, and a poorer long-term prognosis. This is why recognizing the early whispers of RA and navigating the diagnostic journey efficiently is paramount.
Conclusion: A Journey of Resilience and Hope
The diagnostic journey for rheumatoid arthritis is a testament to human resilience. It begins with the disquieting realization that something is wrong, progresses through a complex medical investigation, and often culminates in a diagnosis that, while challenging, opens the door to effective management.
For the knowledgeable patient, understanding each step – from the subtle symptoms to the nuanced blood tests and imaging – transforms the experience from a passive ordeal into an empowered partnership with their medical team. While the path may be long and the answers not always immediate, modern medicine offers powerful tools to combat RA. The story doesn’t end with diagnosis; it evolves into a new chapter of proactive management, adaptation, and the enduring hope for a life lived fully, despite the presence of chronic illness. The journey, ultimately, is one of discovery – of a diagnosis, of medical advancements, and of one’s own inner strength.