Your Blood Sugar, Blood Pressure, and Bones: How Magnesium-Rich Foods Help Regulate It All – The Silent Orchestrator of Health
In the grand symphony of human physiology, where countless processes hum in intricate harmony, there exist certain unsung heroes – minerals that, despite their profound influence, often remain in the background, their critical roles acknowledged only when their absence disrupts the delicate balance. Among these, magnesium stands as a true maestro, a silent orchestrator conducting hundreds of biochemical reactions that underpin our very existence. From the rhythmic beating of our hearts to the steady hum of our metabolism and the resilient structure of our bones, magnesium’s touch is ubiquitous. Yet, in our modern world, this essential mineral has become a forgotten friend, its deficiency a silent epidemic contributing to a cascade of chronic health issues, particularly those concerning blood sugar regulation, blood pressure stability, and skeletal integrity.
This article delves into the captivating story of magnesium – not merely as a nutrient, but as a pivotal player in the epic narrative of human health. We will explore how this remarkable mineral, often overlooked in the glare of more popular vitamins, wields its influence to maintain equilibrium across these three vital systems, unraveling the intricate mechanisms and offering insights into how magnesium-rich foods can become our allies in the quest for optimal well-being.
The Unseen Hand: Magnesium’s Foundational Role in Cellular Life
Before we dissect magnesium’s specific impacts on blood sugar, blood pressure, and bones, it’s imperative to grasp the sheer breadth of its involvement in cellular function. Magnesium is the fourth most abundant mineral in the human body and the second most abundant intracellular cation. Its omnipresence is no accident; it acts as a cofactor in over 600 enzymatic reactions, a number that continues to grow with advancing research. These reactions encompass virtually every metabolic pathway: energy production (ATP synthesis), protein synthesis, DNA and RNA synthesis, glucose metabolism, fatty acid synthesis, muscle contraction, nerve impulse transmission, and the regulation of ion channels.
Think of magnesium as the universal key that unlocks the efficiency of our cellular machinery. Without it, enzymes – the biological catalysts that drive life – would falter, and our cells would struggle to perform their basic functions. This foundational role means that a deficit in magnesium doesn’t just impact one isolated system; it sends ripples of dysfunction throughout the entire organism, creating a fertile ground for chronic disease.
Chapter 1: The Metabolic Maestro – Magnesium and Blood Sugar Regulation
The story of magnesium and blood sugar begins at the cellular gates, where glucose – the body’s primary fuel – seeks entry. Insulin, a hormone produced by the pancreas, acts as the key to these gates, signaling cells to absorb glucose from the bloodstream. This intricate dance between insulin and cellular receptors is critical for maintaining stable blood glucose levels and preventing the onset of insulin resistance and Type 2 Diabetes (T2D). Here, magnesium emerges as a crucial conductor.
The Insulin Sensitivity Symphony:
Magnesium plays a multi-faceted role in enhancing insulin sensitivity. Firstly, it is directly involved in the signaling pathways of insulin. When insulin binds to its receptor on the cell surface, a cascade of intracellular events is triggered, leading to the translocation of glucose transporters (like GLUT4) to the cell membrane, allowing glucose to enter. Magnesium is a necessary cofactor for the enzyme tyrosine kinase, which is part of the insulin receptor complex. Without adequate magnesium, this enzyme’s activity is diminished, impairing the cell’s ability to respond effectively to insulin. It’s like having a key (insulin) but a rusty lock (receptor) that won’t turn properly without lubrication (magnesium).
Secondly, magnesium influences the phosphorylation of the insulin receptor. This process, where phosphate groups are added to proteins, is vital for activating the receptor and initiating the signaling cascade. Magnesium-dependent kinases are essential for this phosphorylation, ensuring the receptor is primed to receive insulin’s message.
Energy Production and Glucose Utilization:
Beyond insulin signaling, magnesium is indispensable for ATP (adenosine triphosphate) synthesis, the universal energy currency of the cell. Many enzymes involved in glycolysis (the breakdown of glucose for energy) and oxidative phosphorylation (the primary pathway for ATP production in mitochondria) require magnesium. A deficiency in magnesium can compromise mitochondrial function, reducing the cell’s capacity to efficiently metabolize glucose for energy. This leads to a vicious cycle: cells become less efficient at using glucose, leading to higher blood sugar levels, and simultaneously, the energy-deprived cells struggle to perform their other magnesium-dependent tasks.
Inflammation and Oxidative Stress:
Chronic inflammation and oxidative stress are known contributors to insulin resistance and pancreatic beta-cell dysfunction. Magnesium possesses anti-inflammatory properties, helping to quell the systemic inflammation that can impair insulin signaling. It also acts as an antioxidant, combating oxidative stress by supporting the activity of various antioxidant enzymes. By reducing these cellular stressors, magnesium creates a healthier environment for insulin to function effectively and for beta cells to produce insulin without undue strain.
The Consequence of Deficiency:
Inadequate magnesium leads to a diminished cellular response to insulin, forcing the pancreas to produce more insulin to achieve the same effect – a hallmark of insulin resistance. Over time, this compensatory mechanism can exhaust the pancreatic beta cells, leading to their eventual failure and the progression to T2D. Studies have consistently shown an inverse relationship between magnesium intake and the risk of T2D, with higher magnesium intake associated with a lower risk. For individuals already living with T2D, magnesium supplementation has been shown to improve glycemic control and insulin sensitivity.
Chapter 2: The Vascular Virtuoso – Magnesium and Blood Pressure Regulation
The story of magnesium and blood pressure unfolds within the intricate network of our circulatory system, where the delicate balance between vasoconstriction (narrowing of blood vessels) and vasodilation (widening of blood vessels) dictates the pressure exerted on arterial walls. Hypertension, or high blood pressure, is a leading risk factor for cardiovascular disease, and here too, magnesium plays a crucial, often underappreciated, role as a vascular virtuoso.
Smooth Muscle Relaxation and Vasodilation:
One of magnesium’s most direct impacts on blood pressure is its ability to induce vasodilation. The walls of our arteries contain smooth muscle cells that contract and relax to regulate blood flow and pressure. Calcium is a primary mediator of muscle contraction, including the contraction of vascular smooth muscle. Magnesium acts as a natural calcium channel blocker, competing with calcium for entry into these cells. By limiting calcium influx, magnesium promotes the relaxation of vascular smooth muscle, leading to wider blood vessels and a reduction in peripheral vascular resistance, thereby lowering blood pressure.
Imagine a constricted garden hose; the water pressure inside is high. Magnesium gently loosens the grip on the hose, allowing the water (blood) to flow more freely and at lower pressure.
Endothelial Function and Nitric Oxide Production:
The endothelium, the inner lining of blood vessels, is crucial for maintaining vascular health. A healthy endothelium produces nitric oxide (NO), a potent vasodilator that relaxes smooth muscle and prevents platelet aggregation. Magnesium is essential for the activity of endothelial nitric oxide synthase (eNOS), the enzyme responsible for NO production. By ensuring adequate NO levels, magnesium supports healthy endothelial function, promoting vasodilation and protecting against arterial stiffness, a hallmark of hypertension.
Electrolyte Balance and Sodium-Potassium Pump:
Magnesium is intimately involved in regulating the balance of other key electrolytes, particularly sodium and potassium, which are critical for maintaining fluid balance and nerve and muscle function, including the heart. Magnesium is required for the proper functioning of the sodium-potassium pump (Na+/K+-ATPase), an enzyme embedded in cell membranes that actively pumps sodium out of cells and potassium into them. This pump is vital for maintaining cellular membrane potential and preventing excessive sodium retention, which can contribute to hypertension. A magnesium deficiency can impair this pump, leading to intracellular sodium accumulation and a cascade of events that can elevate blood pressure.
Modulation of the Renin-Angiotensin-Aldosterone System (RAAS):
The RAAS is a complex hormonal system that plays a central role in regulating blood pressure and fluid balance. Overactivity of the RAAS is a common feature of hypertension. Magnesium has been shown to modulate various components of the RAAS, potentially reducing the production of angiotensin II (a potent vasoconstrictor) and aldosterone (a hormone that promotes sodium and water retention). By dampening an overzealous RAAS, magnesium contributes to a more balanced blood pressure regulation.
Stress and Sympathetic Nervous System:
Chronic stress activates the sympathetic nervous system, leading to the release of stress hormones like adrenaline and noradrenaline, which can increase heart rate and constrict blood vessels, elevating blood pressure. Magnesium has calming effects on the nervous system, helping to regulate the stress response. It helps reduce the excitability of nerve cells and promotes relaxation, thereby mitigating the blood pressure-raising effects of chronic stress.
The Consequence of Deficiency:
A chronic deficit in magnesium can lead to increased vascular tone, reduced nitric oxide production, impaired electrolyte balance, and an overactive stress response – all converging to contribute to the development and progression of hypertension. Observational studies and meta-analyses consistently link lower magnesium intake with a higher risk of high blood pressure, and magnesium supplementation has shown modest but significant reductions in blood pressure, particularly in individuals with pre-existing hypertension or magnesium deficiency.
Chapter 3: The Skeletal Steward – Magnesium and Bone Health
The story of magnesium and bone health is often overshadowed by calcium and vitamin D, yet magnesium is a fundamental architect and steward of our skeletal system. Bones are not inert structures; they are dynamic, living tissues constantly undergoing remodeling, with old bone being removed by osteoclasts and new bone being formed by osteoblasts. Magnesium is vital at every stage of this intricate process, impacting bone mineral density, crystal formation, and the regulation of other bone-building nutrients.
The Bone Matrix Blueprint:
Approximately 60% of the body’s magnesium is stored in the bones, either on the surface or within the bone crystal lattice. Magnesium is a crucial component of hydroxyapatite, the primary mineral crystal that gives bone its strength and rigidity. It contributes to the crystal structure itself and influences crystal size and density. Adequate magnesium levels are essential for the formation of strong, healthy bone crystals. A deficiency can lead to larger, more brittle crystals that are more prone to fracture.
Parathyroid Hormone (PTH) and Vitamin D Activation:
Magnesium’s role in bone health extends to its crucial interplay with parathyroid hormone (PTH) and Vitamin D, two key regulators of calcium and phosphate metabolism.
- PTH Regulation: The parathyroid glands secrete PTH, which helps maintain blood calcium levels by stimulating its release from bones. However, both an excess and a deficiency of magnesium can impair PTH secretion. Magnesium is required for the proper functioning of the calcium-sensing receptor on parathyroid cells. Without sufficient magnesium, PTH secretion can be inappropriately low or resistant to calcium signals, leading to imbalances in calcium metabolism.
- Vitamin D Activation: Vitamin D is vital for calcium absorption in the gut and its incorporation into bone. However, Vitamin D is biologically inert and must be converted into its active form (calcitriol) in the liver and kidneys. All the enzymes that metabolize Vitamin D require magnesium as a cofactor. Without adequate magnesium, even if you consume enough Vitamin D, your body cannot effectively utilize it, rendering your calcium absorption and bone mineralization efforts less effective. It’s like having a blueprint (Vitamin D) but lacking the essential tools (magnesium) to build the structure.
Calcium Regulation and Bone Mineral Density:
While calcium is the star of bone health, magnesium acts as its indispensable supporting cast. Magnesium regulates calcium transport across cell membranes, ensuring that calcium goes where it’s needed (into bones) and doesn’t accumulate where it’s detrimental (in soft tissues like arteries, contributing to calcification). It helps maintain the proper calcium-to-magnesium ratio, which is critical for bone health. An imbalance, particularly an excess of calcium without adequate magnesium, can paradoxically weaken bones and contribute to other health issues.
Osteoblast and Osteoclast Activity:
Magnesium influences the activity of both osteoblasts (bone-building cells) and osteoclasts (bone-resorbing cells). It appears to stimulate osteoblast proliferation and differentiation, promoting the formation of new bone tissue. Simultaneously, it may modulate osteoclast activity, helping to prevent excessive bone breakdown. This balanced regulation is essential for maintaining bone mineral density and preventing conditions like osteoporosis.
Inflammation and Oxidative Stress:
Similar to its role in blood sugar and blood pressure, magnesium’s anti-inflammatory and antioxidant properties contribute to bone health. Chronic low-grade inflammation and oxidative stress can accelerate bone loss by promoting osteoclast activity and inhibiting osteoblast function. By mitigating these factors, magnesium creates a more favorable environment for bone maintenance and growth.
The Consequence of Deficiency:
Chronic magnesium deficiency leads to a cascade of detrimental effects on bones: impaired Vitamin D activation, altered PTH secretion, reduced bone mineral density, and an increased risk of osteoporosis and fractures. Studies have shown a significant correlation between lower magnesium intake and lower bone mineral density, especially in older adults and postmenopausal women. While calcium and Vitamin D are crucial, their efficacy for bone health is severely hampered in the absence of adequate magnesium.
The Modern Paradox: Why Magnesium Deficiency is So Prevalent
Given magnesium’s profound and pervasive roles, one might assume it’s a nutrient we effortlessly obtain. Yet, the story takes a somber turn as we confront the reality of widespread magnesium deficiency in the modern world. Several factors contribute to this silent epidemic:
- Soil Depletion: Decades of intensive farming practices have stripped essential minerals, including magnesium, from our agricultural soils. Crops grown in nutrient-depleted soil naturally contain less magnesium, meaning even "healthy" foods may offer less than they once did.
- Food Processing: The refining and processing of foods significantly reduce their magnesium content. Whole grains, for example, are rich in magnesium, but milling them into white flour removes the magnesium-rich germ and bran. Similarly, refined sugars and fats contain virtually no magnesium.
- Modern Dietary Habits: The typical Western diet, characterized by high consumption of processed foods, refined sugars, unhealthy fats, and a low intake of whole, unprocessed foods, is inherently magnesium-poor.
- Stress: Chronic psychological and physiological stress increases the body’s demand for magnesium and leads to its increased excretion. The fight-or-flight response depletes magnesium, creating a vicious cycle where stress depletes magnesium, and low magnesium exacerbates the stress response.
- Medications: Many commonly prescribed medications can interfere with magnesium absorption or increase its excretion. These include diuretics (often prescribed for hypertension), proton pump inhibitors (for acid reflux), antibiotics, and certain chemotherapy drugs.
- Chronic Diseases: Conditions like diabetes, kidney disease, and gastrointestinal disorders (e.g., Crohn’s disease, celiac disease) can impair magnesium absorption or increase its loss.
- Alcohol Consumption: Excessive alcohol intake increases urinary magnesium excretion and can impair its absorption.
- Aging: As we age, magnesium absorption tends to decrease, and kidney excretion may increase, making older adults particularly vulnerable to deficiency.
The challenge in diagnosing magnesium deficiency further complicates the narrative. Standard blood tests for magnesium (serum magnesium) often do not accurately reflect the body’s total magnesium status, as only about 1% of the body’s magnesium is in the blood. The majority resides within cells and bones. Thus, a "normal" serum magnesium level can mask a significant intracellular deficiency.
Reclaiming the Maestro: Embracing Magnesium-Rich Foods
The story of magnesium, though punctuated by the challenges of modern life, offers a hopeful resolution. By consciously reintroducing magnesium-rich foods into our diets, we can empower our bodies to restore balance and resilience.
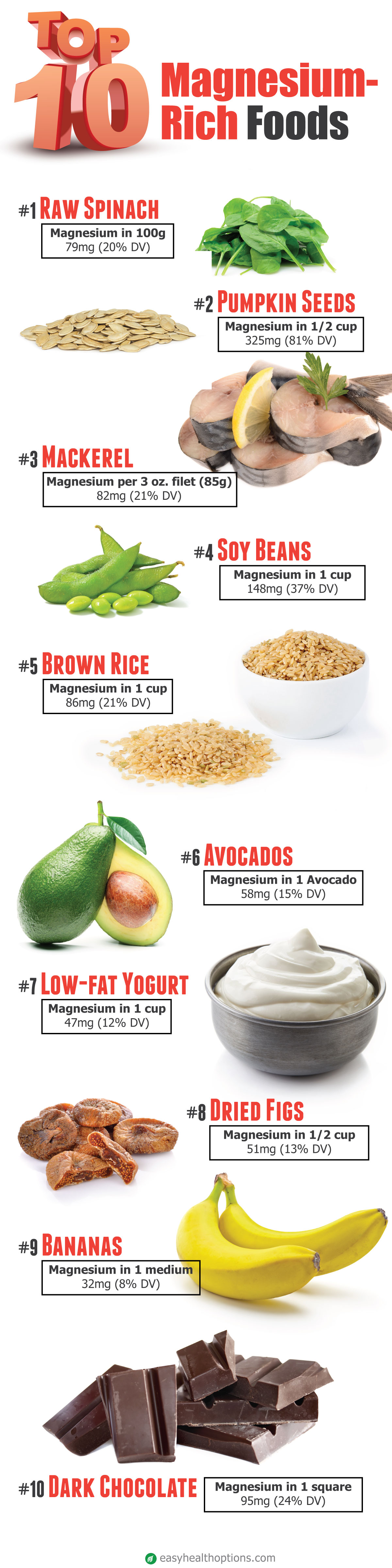
Magnesium-Rich Food Sources:
- Dark Leafy Greens: Spinach, kale, Swiss chard, collard greens are nutritional powerhouses packed with magnesium.
- Nuts and Seeds: Almonds, cashews, pumpkin seeds, chia seeds, flax seeds, and sunflower seeds are excellent sources.
- Legumes: Black beans, lentils, chickpeas, and edamame provide substantial magnesium.
- Whole Grains: Oats, quinoa, brown rice, and whole wheat are far superior to their refined counterparts.
- Avocados: A creamy, delicious source of healthy fats and magnesium.
- Dark Chocolate: Opt for chocolate with a high cocoa content (70% or more) for a magnesium boost (and antioxidants!).
- Bananas: A popular fruit that offers a decent amount of magnesium.
- Fatty Fish: Salmon, mackerel, and halibut contain magnesium along with beneficial omega-3 fatty acids.
- Tofu: A versatile plant-based protein that is also a good source of magnesium.
Beyond the Plate: Considerations for Optimal Absorption
While dietary intake is paramount, several factors influence magnesium absorption:
- Phytates and Oxalates: Found in some plant foods (like spinach and whole grains), these compounds can bind to magnesium, reducing its bioavailability. However, the overall nutritional benefits of these foods typically outweigh this effect, and soaking, sprouting, or fermenting can reduce phytate content.
- Vitamin D: As discussed, adequate Vitamin D is essential for magnesium’s function, and vice versa.
- Gut Health: A healthy gut microbiome and intestinal lining are crucial for efficient mineral absorption.
- Stress Management: Reducing chronic stress can prevent magnesium depletion.
Strategic Supplementation: When and How
For some individuals, especially those with diagnosed deficiency, chronic diseases, or high magnesium demands, dietary sources alone may not be sufficient. In such cases, magnesium supplementation might be considered, always under the guidance of a healthcare professional.
Different forms of magnesium supplements offer varying absorption rates and potential benefits:
- Magnesium Citrate: Highly bioavailable, often used for its laxative effect in higher doses.
- Magnesium Glycinate/Bisglycinate: Highly absorbable, well-tolerated, and less likely to cause digestive upset; often favored for its calming effects.
- Magnesium Malate: May be beneficial for energy production and muscle pain.
- Magnesium L-Threonate: Known for its ability to cross the blood-brain barrier, potentially benefiting cognitive function.
- Magnesium Oxide: Less bioavailable, often used for constipation relief rather than correcting deficiency.
It’s crucial to note that excessive magnesium intake, especially from supplements, can lead to side effects like diarrhea, nausea, and abdominal cramping. In rare cases, extremely high doses can cause magnesium toxicity, particularly in individuals with kidney impairment.
The Symphony Continues: A Holistic Perspective
The story of magnesium and its profound impact on blood sugar, blood pressure, and bones is a compelling testament to the interconnectedness of our physiological systems. It highlights how a seemingly small mineral can exert immense influence, serving as a reminder that true health is not about addressing isolated symptoms but fostering holistic balance.
By understanding magnesium’s role as a silent orchestrator, we are empowered to make informed dietary and lifestyle choices that support its vital functions. Embracing a diet rich in whole, unprocessed foods, managing stress, and being mindful of medications that may interfere with magnesium status are all critical steps in reclaiming this maestro for our health.
The narrative of magnesium is far from over. Ongoing research continues to uncover new facets of its incredible versatility, from its potential role in mental health to its influence on athletic performance. What remains clear, however, is that this unsung hero deserves a prominent place in our consciousness as we strive for a healthier, more balanced existence. Let us listen to the subtle whispers of our bodies and allow magnesium to conduct its essential symphony, ensuring our blood sugar, blood pressure, and bones remain in perfect harmony for years to come.