Your Heart’s Best Friend: Why Magnesium is Key to Maintaining a Steady Beat and Blood Pressure
The Heart’s Silent Symphony: A Delicate Balance
Imagine the human heart, not merely as a pump, but as a tireless, intricate orchestra. For every moment of our lives, from the first flutter in the womb to the final beat, this muscular marvel conducts a symphony of contractions and relaxations, a relentless rhythm that sustains every cell, every thought, every movement. It’s a performance of unparalleled precision, driven by electrical impulses and fueled by biochemical reactions, all orchestrated to maintain a steady beat and a healthy blood pressure. When this symphony falters – when the rhythm becomes erratic or the pressure climbs too high – the consequences can be profound, casting a shadow over our health and vitality.
For centuries, medical science has painstakingly peeled back the layers of this complexity, identifying the major players: sodium, potassium, and calcium, the star soloists of cellular electrophysiology. Yet, often overlooked, working diligently behind the scenes, is a mineral that acts as the quiet, indispensable conductor, the heart’s true best friend: magnesium. This unsung hero, a humble cation, holds the key to maintaining the heart’s steady beat and regulating the intricate dance of blood pressure. To truly appreciate magnesium’s profound impact, we must embark on a journey deep into the heart’s inner workings, uncovering the story of its crucial role in this life-sustaining performance.
Magnesium: The Unsung Hero – A Molecular Biography
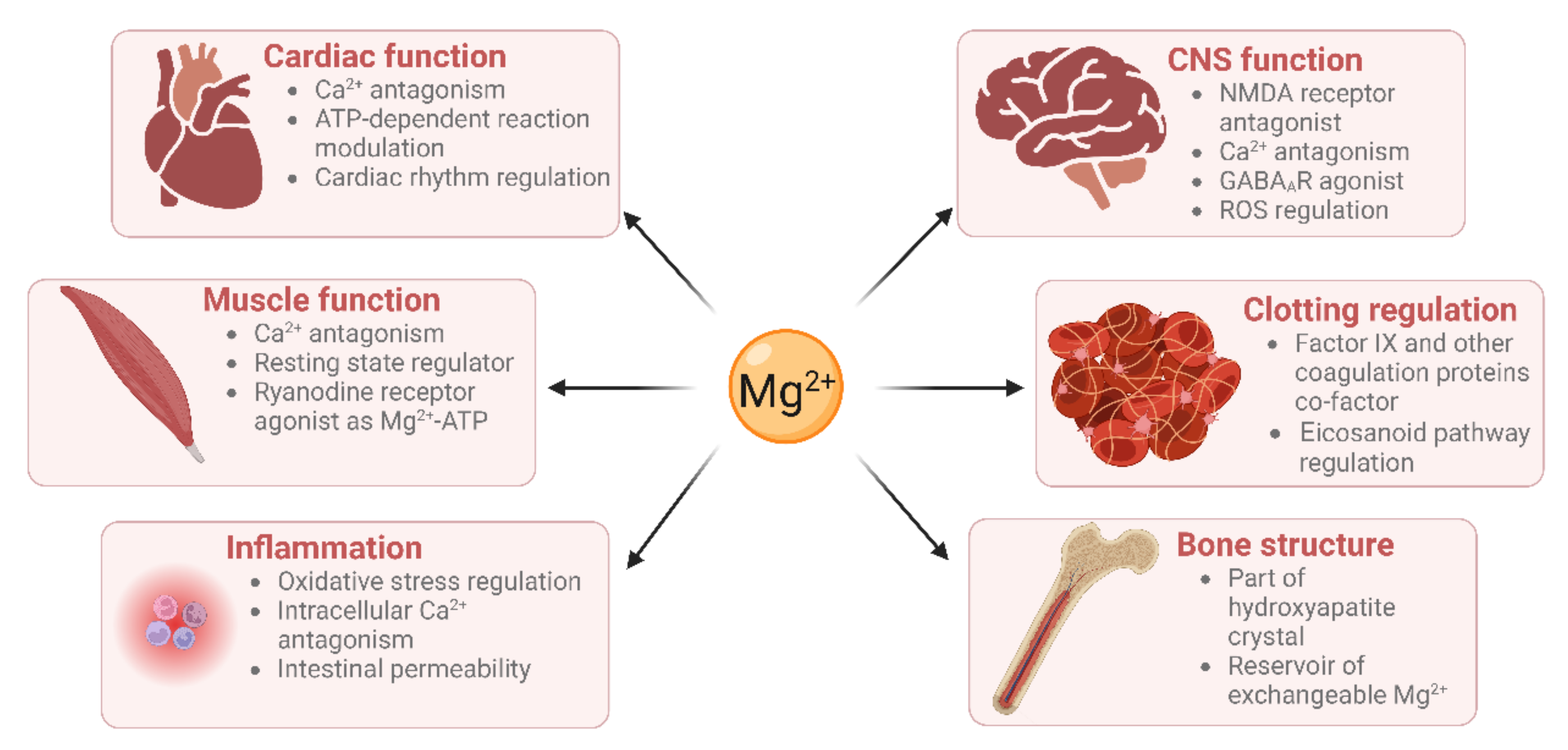
Magnesium (Mg) is the fourth most abundant mineral in the human body, an essential macronutrient involved in over 300 enzymatic reactions. Its ubiquity speaks volumes about its fundamental importance. Found predominantly within our bones (60%), muscles, and soft tissues, with only a tiny fraction (less than 1%) circulating in the blood, magnesium is a true intracellular powerhouse. It’s not just a nutrient; it’s a critical cofactor, a molecular assistant that enables countless biological processes to occur smoothly and efficiently.
From the synthesis of DNA and RNA to energy production in the form of ATP, from muscle contraction and nerve transmission to the regulation of blood glucose levels, magnesium’s fingerprints are everywhere. Yet, despite its pervasive influence, its specific role in cardiovascular health often remains overshadowed by more commonly discussed minerals. For the knowledgeable audience, it’s crucial to understand that magnesium doesn’t just play a supporting role; it’s a foundational element, a molecular linchpin that directly influences the very mechanisms that govern heart rhythm and blood pressure.
The understanding of magnesium’s significance has evolved over time. Early researchers in the late 19th and early 20th centuries began to observe its effects on muscle contraction and nerve excitability. By the mid-20th century, its role in preventing eclampsia and treating certain arrhythmias started to emerge in clinical practice. However, it is only in recent decades, with advanced molecular and physiological research, that the full scope of its intricate interactions within the cardiovascular system has been unveiled. This journey of discovery paints a compelling picture of magnesium as an orchestrator, a stabilizer, and a protector of the heart.
The Electrifying Dance: Magnesium and Cardiac Rhythm
The heart’s rhythm is a marvel of electrical engineering. Each beat originates from specialized pacemaker cells that generate an electrical impulse, which then propagates through the heart muscle, triggering a coordinated contraction. This intricate process relies on the precise movement of ions – charged particles – across cell membranes, creating what are known as action potentials. Sodium, potassium, and calcium ions are the primary dancers in this electrical ballet, but magnesium is the choreographer, ensuring each step is perfectly timed and executed.
At the cellular level, magnesium exerts its influence through several critical mechanisms:
-
Ion Channel Modulation: Magnesium acts as a natural calcium channel blocker. Calcium ions are essential for muscle contraction, but too much calcium entering heart cells can lead to over-excitation, sustained contraction, and even cell damage. Magnesium directly competes with calcium for binding sites on the cell membrane, effectively limiting calcium influx. This "calcium antagonist" effect is fundamental to preventing hyperexcitability and maintaining a relaxed state during diastole (the heart’s filling phase). Beyond calcium channels, magnesium also modulates potassium channels, influencing the repolarization phase of the action potential, which is crucial for resetting the cell for the next beat. It ensures the outflow of potassium ions is neither too fast nor too slow, preventing both premature beats and prolonged QT intervals, which can lead to life-threatening arrhythmias.
-
The Na+/K+ ATPase Pump: This vital pump, located in the cell membrane, actively transports sodium ions out of the cell and potassium ions into the cell, maintaining the electrochemical gradient essential for nerve and muscle function. The Na+/K+ ATPase pump is magnesium-dependent; it requires magnesium as a cofactor to function properly. Without adequate magnesium, this pump becomes inefficient, leading to an imbalance of sodium and potassium that can destabilize the cell membrane and predispose the heart to arrhythmias.
-
Membrane Stabilization: Magnesium helps stabilize the cell membranes of cardiomyocytes (heart muscle cells). By interacting with phospholipids in the cell membrane, magnesium reduces membrane permeability, making the cells less prone to uncontrolled depolarization and spontaneous electrical activity. This stabilizing effect is akin to a finely tuned shock absorber, dampening erratic electrical signals and promoting a smooth, consistent rhythm.
-
ATP Production: All cellular processes, including the active transport of ions and the contraction of muscle fibers, require energy in the form of adenosine triphosphate (ATP). Magnesium is indispensable for ATP synthesis and stability. ATP exists in the cell primarily as a complex with magnesium (Mg-ATP). Without magnesium, ATP cannot be effectively utilized, leading to energy depletion that can impair the heart’s ability to maintain its electrical and mechanical functions.
When magnesium levels are insufficient, the delicate balance of these processes is disrupted. The heart becomes more electrically unstable, akin to an orchestra where the conductor has stepped away, and the musicians begin to play out of sync. This instability can manifest as various arrhythmias:
- Atrial Fibrillation (AFib): A common arrhythmia characterized by rapid, irregular quivering of the atria. Magnesium deficiency can contribute to AFib by increasing atrial excitability and promoting calcium overload. Studies have shown that magnesium supplementation can help reduce the frequency and severity of AFib episodes, and intravenous magnesium is a standard treatment in acute AFib management.
- Premature Ventricular Contractions (PVCs): These are extra, abnormal heartbeats that originate in the ventricles. While often benign, frequent PVCs can be a sign of underlying cardiac irritability, and magnesium deficiency is a known contributor.
- Ventricular Tachycardia/Fibrillation: These are life-threatening arrhythmias where the ventricles beat too fast and erratically, leading to insufficient blood pumping and potentially sudden cardiac death. In acute settings, intravenous magnesium is a critical intervention, particularly in cases of Torsades de Pointes, a specific type of ventricular tachycardia often associated with electrolyte imbalances.
The story of magnesium and cardiac rhythm is one of precise regulation and vital support. It highlights how a seemingly simple mineral acts as the guardian of the heart’s electrical integrity, preventing chaos and ensuring the harmonious flow of life-sustaining beats.
Taming the Pressure: Magnesium and Blood Pressure Regulation
Beyond its role in maintaining a steady beat, magnesium is also a formidable ally in the fight against hypertension, or high blood pressure – a condition that silently damages arteries and significantly increases the risk of heart attack, stroke, and kidney disease. The regulation of blood pressure is a complex physiological dance involving the nervous system, hormones, and the intricate mechanics of blood vessels. Magnesium, once again, emerges as a critical choreographer in this elaborate performance.
Its influence on blood pressure can be understood through several key mechanisms:
-
Vascular Tone and Vasodilation: The primary way magnesium impacts blood pressure is through its direct effect on the smooth muscle cells lining blood vessels. Much like in the heart, magnesium acts as a natural calcium channel blocker in vascular smooth muscle cells. Calcium influx into these cells triggers contraction, leading to vasoconstriction (narrowing of blood vessels) and an increase in blood pressure. By limiting calcium entry, magnesium promotes the relaxation of vascular smooth muscle, leading to vasodilation (widening of blood vessels) and a subsequent decrease in blood pressure. This effect is akin to loosening a constricting band, allowing blood to flow more freely and with less resistance.
-
Nitric Oxide Synthesis: Magnesium plays a crucial role in the production of nitric oxide (NO), a potent vasodilator. NO is a signaling molecule produced by endothelial cells (the inner lining of blood vessels) that signals the surrounding smooth muscle cells to relax. Magnesium is a cofactor for the enzyme nitric oxide synthase (eNOS), which catalyzes NO production. Adequate magnesium levels ensure robust NO synthesis, contributing to healthy vasodilation and flexible, responsive blood vessels. Conversely, magnesium deficiency can impair NO production, leading to increased vascular tone and elevated blood pressure.
-
Counteracting Vasoconstrictors: The body produces several powerful vasoconstrictors, such as endothelin-1 and angiotensin II, which can raise blood pressure. Magnesium helps to blunt the effects of these potent chemicals. It can directly inhibit the release of endothelin-1 and reduce the sensitivity of blood vessels to angiotensin II, thereby mitigating their pressor effects. This antagonistic action adds another layer of protection against excessive vasoconstriction.
-
Renin-Angiotensin-Aldosterone System (RAAS) Modulation: The RAAS is a hormonal system that plays a central role in regulating blood pressure and fluid balance. Angiotensin II, a key component of RAAS, not only causes vasoconstriction but also stimulates aldosterone release, which promotes sodium and water retention, further increasing blood pressure. There is evidence that magnesium can modulate various components of the RAAS, potentially dampening its overall activity and contributing to blood pressure control. While the exact mechanisms are still being elucidated, it appears magnesium can influence renin secretion and reduce the sensitivity to angiotensin II.
-
Insulin Sensitivity and Metabolic Syndrome: The connection between insulin resistance, metabolic syndrome, and hypertension is well-established. Magnesium is intimately involved in glucose metabolism and insulin signaling. It acts as a cofactor for enzymes involved in glucose utilization and improves insulin sensitivity. In individuals with insulin resistance, cells become less responsive to insulin, leading to higher blood sugar levels and often, compensatory increases in insulin production. High insulin levels can contribute to hypertension by promoting sodium retention, increasing sympathetic nervous system activity, and fostering vascular stiffness. By improving insulin sensitivity, magnesium indirectly helps to lower blood pressure in individuals prone to metabolic syndrome.
In essence, magnesium serves as a powerful natural antihypertensive agent, working through multiple pathways to relax blood vessels, enhance endothelial function, and counter the forces that would otherwise elevate blood pressure. It doesn’t just treat symptoms; it addresses fundamental physiological imbalances that contribute to hypertension. For those struggling with or at risk of high blood pressure, magnesium is not merely a supplement but a foundational component of a holistic strategy for cardiovascular well-being.
The Silent Epidemic: Magnesium Deficiency
Given magnesium’s pervasive and critical roles, one might assume that maintaining adequate levels would be a top priority. However, the reality is starkly different. Magnesium deficiency, often referred to as a "silent epidemic," is alarmingly common, affecting a significant portion of the global population, particularly in industrialized nations. The insidious nature of this deficiency lies in its often subtle and non-specific symptoms, making it difficult to diagnose and frequently overlooked by healthcare professionals.
Several factors contribute to this widespread deficiency:
-
Modern Diet: Our modern Western diet, rich in processed foods, refined grains, and sugars, is notoriously low in magnesium. Processing often strips foods of their mineral content. For instance, milling whole wheat into white flour removes up to 80% of its magnesium. The reliance on highly processed foods means many individuals consume diets that are calorie-dense but nutrient-poor.
-
Soil Depletion: Agricultural practices over decades have led to significant depletion of magnesium and other minerals in our soils. Crops grown in mineral-depleted soil naturally contain less magnesium, meaning even "healthy" foods may provide less of this vital mineral than they once did.
-
Chronic Diseases and Medications: Many common chronic conditions can either increase magnesium requirements or lead to its excessive loss. Diabetes, Crohn’s disease, celiac disease, and kidney disease are just a few examples. Furthermore, a plethora of commonly prescribed medications can deplete magnesium levels. Diuretics (often prescribed for hypertension), proton pump inhibitors (for acid reflux), certain antibiotics, and chemotherapy drugs can all interfere with magnesium absorption or increase its excretion.
-
Lifestyle Factors: Stress, both physical and psychological, increases the body’s demand for magnesium. High alcohol consumption leads to increased urinary excretion of magnesium. Excessive caffeine intake can also contribute to losses. Even strenuous exercise can deplete magnesium stores, as it’s used in muscle contraction and energy production.
-
Diagnostic Challenges: Diagnosing magnesium deficiency is notoriously difficult. The standard serum magnesium test, which measures the magnesium circulating in the blood, is often a poor indicator of total body magnesium stores. Since less than 1% of the body’s magnesium is in the blood, serum levels can appear normal even when significant intracellular depletion exists. The body tightly regulates serum magnesium within a narrow range, often at the expense of drawing magnesium from bones and tissues, masking a true deficiency. More accurate tests, such as red blood cell magnesium levels or magnesium loading tests, are less commonly performed.
The symptoms of magnesium deficiency can range from mild and non-specific to severe and debilitating. Early signs often include muscle cramps, twitching, fatigue, weakness, anxiety, irritability, and insomnia. As the deficiency progresses, more serious issues can emerge, directly impacting the cardiovascular system: increased risk of arrhythmias, elevated blood pressure, and even exacerbation of conditions like heart failure. The silent nature of this epidemic means that many individuals are living with suboptimal magnesium levels, unknowingly increasing their vulnerability to chronic diseases, particularly those affecting the heart. Understanding these contributing factors and diagnostic challenges is the first step in addressing this widespread and impactful nutrient gap.
Magnesium in Practice: From Prevention to Intervention
Given the widespread prevalence of magnesium deficiency and its profound implications for cardiovascular health, the practical application of this knowledge becomes paramount. Integrating magnesium into both preventive strategies and clinical interventions is a powerful approach to fostering a healthier heart.
Dietary Sources: The Foundation of Prevention
The most natural and often preferred way to ensure adequate magnesium intake is through a nutrient-dense diet. Emphasizing whole, unprocessed foods is key. Excellent dietary sources of magnesium include:
- Leafy Green Vegetables: Spinach, kale, Swiss chard are powerhouse sources.
- Nuts and Seeds: Almonds, cashews, pumpkin seeds, chia seeds, flax seeds are rich in magnesium.
- Legumes: Black beans, lentils, chickpeas.
- Whole Grains: Brown rice, oats, whole wheat (though less than unprocessed forms).
- Avocados: A delicious and healthy source.
- Dark Chocolate: Yes, a little dark chocolate (70% cocoa or higher) can contribute to your magnesium intake!
- Bananas: A good source, along with other essential electrolytes.
- Fatty Fish: Salmon, mackerel.
Incorporating these foods regularly into meals can significantly boost magnesium intake and lay a strong foundation for cardiovascular health. Cooking methods matter; boiling can leach some minerals, so steaming or roasting is often preferred.
Supplementation: Bridging the Gap
While diet is fundamental, supplementation often becomes necessary, especially for individuals with diagnosed deficiency, chronic conditions, medication use, or those unable to meet their needs through diet alone. The world of magnesium supplements can be complex, with various forms offering different bioavailability and specific benefits:
- Magnesium Citrate: A common and well-absorbed form, often used for its laxative effect in higher doses.
- Magnesium Glycinate/Bisglycinate: Highly bioavailable and generally well-tolerated, less likely to cause digestive upset. Often favored for its calming effects and for those with sensitive stomachs.
- Magnesium Malate: Often recommended for muscle pain and fatigue, as malic acid is involved in energy production.
- Magnesium L-Threonate: A newer form that shows promise in crossing the blood-brain barrier, potentially benefiting cognitive function, though its cardiovascular effects are less specifically studied compared to other forms.
- Magnesium Oxide: While it contains a high percentage of elemental magnesium, its bioavailability is relatively low. Often used as an antacid or laxative.
- Magnesium Sulfate (Epsom Salts): Primarily used externally in baths for muscle relaxation or intravenously in acute medical settings. Oral absorption is poor.
- Magnesium Taurate: Combines magnesium with taurine, an amino acid that also supports cardiovascular health. This combination may offer synergistic benefits for heart rhythm and blood pressure.
Dosage and Considerations: The recommended daily allowance (RDA) for adults typically ranges from 310-420 mg, depending on age and sex. However, therapeutic doses for specific conditions may be higher, always under medical supervision.
Potential Side Effects: The most common side effect of oral magnesium supplementation is diarrhea, especially with forms like citrate or oxide, or at higher doses. This can often be mitigated by choosing a more bioavailable form like glycinate or by dividing doses throughout the day.
Contraindications: Magnesium supplementation should be approached with caution in individuals with kidney impairment, as they may have difficulty excreting excess magnesium, leading to hypermagnesemia, which can be dangerous. Always consult a healthcare professional before starting any new supplement regimen, particularly if you have underlying health conditions or are taking medications.
Clinical Applications: Magnesium as a Therapeutic Tool
Beyond daily prevention, magnesium has a well-established role in acute clinical settings:
- Acute Myocardial Infarction (Heart Attack): Intravenous magnesium is sometimes used in post-MI patients, particularly those with arrhythmias or magnesium deficiency, to stabilize heart rhythm and reduce complications.
- Eclampsia and Pre-eclampsia: Magnesium sulfate is the gold standard treatment for preventing and managing seizures in pregnant women with severe pre-eclampsia and eclampsia, demonstrating its powerful neuroprotective and vasodilatory effects.
- Asthma: IV magnesium is used in severe acute asthma exacerbations to relax bronchial smooth muscles.
- Torsades de Pointes: As mentioned, IV magnesium is the first-line treatment for this life-threatening ventricular arrhythmia.
- Migraine Headaches: Magnesium supplementation, particularly magnesium oxide or citrate, has shown efficacy in preventing migraine attacks in some individuals.
For chronic conditions like hypertension and heart failure, magnesium supplementation, when appropriate, can be a valuable adjunct to conventional therapy. Its ability to relax blood vessels, improve endothelial function, and stabilize heart rhythm directly addresses key pathophysiological mechanisms of these diseases. The story of magnesium in practice is one of empowering individuals through dietary choices and, when necessary, targeted supplementation and clinical intervention, to bolster the heart’s resilience and maintain its lifelong symphony.
Beyond the Heart: Magnesium’s Wider Symphony
While our focus has been on magnesium’s indispensable role in maintaining a steady beat and blood pressure, its influence reverberates throughout the entire body, affecting numerous other systems. Understanding these broader implications further solidifies magnesium’s status as a fundamental determinant of overall health and well-being. It is truly a master conductor for the body’s entire physiological orchestra.
-
Bone Health: Magnesium is intricately linked with calcium and vitamin D metabolism. Approximately 60% of the body’s magnesium is stored in bone, playing a crucial role in bone structure and density. It’s essential for the conversion of vitamin D into its active form and helps regulate parathyroid hormone, both of which are critical for calcium homeostasis. Chronic magnesium deficiency can contribute to osteoporosis and increase the risk of fractures, demonstrating that strong bones require more than just calcium.
-
Muscle Function and Relaxation: Beyond the heart, magnesium is vital for the proper function of all muscles, including skeletal muscles. It acts as a natural muscle relaxant, counteracting calcium’s role in muscle contraction. Magnesium deficiency often manifests as muscle cramps, spasms, restless legs syndrome, and general muscle weakness. Athletes, in particular, may benefit from adequate magnesium intake to support muscle recovery and prevent cramps.
-
Nervous System Health: Anxiety, Depression, and Sleep: Magnesium plays a significant role in neurotransmitter function and nerve transmission. It helps regulate GABA (gamma-aminobutyric acid), an inhibitory neurotransmitter that promotes relaxation and reduces anxiety. Magnesium deficiency can lead to increased nerve excitability, anxiety, irritability, poor sleep quality, and even contribute to symptoms of depression. Supplementation with forms like magnesium glycinate is often recommended for its calming effects and ability to promote restful sleep. Its ability to modulate stress hormones and reduce neuronal hyperexcitability underscores its importance for mental and emotional well-being.
-
Energy Production: As mentioned earlier, magnesium is essential for ATP production, the body’s primary energy currency. Every molecule of ATP requires magnesium to be biologically active. Without sufficient magnesium, the body’s energy factories (mitochondria) cannot function efficiently, leading to chronic fatigue, low stamina, and a general feeling of malaise. For those struggling with unexplained tiredness, magnesium deficiency is often a culprit.
-
Diabetes Management: Magnesium’s role in insulin sensitivity extends its impact to diabetes prevention and management. It is a cofactor for enzymes involved in carbohydrate metabolism and helps cells respond more effectively to insulin. Individuals with type 2 diabetes often have lower magnesium levels, and deficiency can worsen insulin resistance, making blood sugar control more challenging. Magnesium supplementation has been shown in some studies to improve glycemic control and reduce the risk of developing type 2 diabetes.
-
Migraine Prevention: For individuals suffering from chronic migraines, magnesium has emerged as a promising prophylactic treatment. Its mechanisms of action in migraine prevention are thought to include its ability to relax blood vessels in the brain, modulate neurotransmitter release, and reduce neuronal hyperexcitability, all of which are implicated in migraine pathophysiology.
-
Inflammation: Chronic low-grade inflammation is a driver of many chronic diseases, including cardiovascular disease. Magnesium has anti-inflammatory properties, helping to reduce markers of inflammation throughout the body. By participating in numerous antioxidant defense systems, it helps protect cells from oxidative stress, another key contributor to disease progression.
This broader view of magnesium’s functions paints a comprehensive picture of a mineral that is not just vital for the heart, but for the harmonious operation of the entire human system. Its deficiency, therefore, doesn’t just impact one organ; it can cascade into a myriad of health issues, subtly undermining well-being across multiple domains.
The Future of Heart Health: A Magnesium-Rich Paradigm
As we conclude our journey into the world of magnesium, the story that emerges is one of profound importance, subtle power, and often, tragic oversight. Magnesium is not a magic bullet, but it is an indispensable foundational nutrient, a quiet conductor that orchestrates the heart’s steady beat and regulates the delicate balance of blood pressure. Its presence ensures the smooth flow of electrical impulses, the relaxation of blood vessels, and the efficient functioning of countless cellular processes vital for cardiovascular health.
The challenge lies in the silent nature of its deficiency and the prevailing focus on more visible symptoms and interventions. For too long, magnesium has remained in the shadows, its pivotal role underestimated or misunderstood. Yet, the scientific evidence is clear and compelling: magnesium deficiency is a pervasive issue with serious implications for heart health, contributing to arrhythmias, hypertension, and overall cardiovascular vulnerability.
The future of heart health, particularly for a knowledgeable audience, must embrace a magnesium-rich paradigm. This means:
- Elevating Dietary Awareness: Empowering individuals to make informed food choices, prioritizing magnesium-rich whole foods, and understanding how modern diets and agricultural practices impact nutrient density.
- Rethinking Diagnostic Approaches: Moving beyond reliance on serum magnesium alone and advocating for more accurate assessments of intracellular magnesium status when deficiency is suspected.
- Integrating Magnesium into Clinical Practice: For healthcare providers, this means considering magnesium deficiency as a potential underlying factor in patients presenting with arrhythmias, hypertension, heart failure, and other cardiovascular complaints, especially in the context of chronic medication use or specific disease states. It also involves judicious use of magnesium supplementation as an adjunct therapy where appropriate.
- Promoting Holistic Wellness: Recognizing that magnesium’s benefits extend far beyond the heart, influencing bone health, muscle function, mental well-being, energy levels, and metabolic health. A holistic approach to health naturally incorporates adequate magnesium intake.
The heart, our tireless symphony, deserves the best care and the most supportive environment. Magnesium, its quiet best friend, stands ready to play its essential role, ensuring the rhythm remains steady, the pressure stays balanced, and the music of life continues to play on, strong and true. It is time for us to acknowledge this unsung hero, to embrace its power, and to invite it fully into the narrative of cardiovascular well-being. By doing so, we not only protect our hearts but enrich the entirety of our lives.