Curbing the Cramps: How Increasing Magnesium Intake Can Silence Muscle Spasms
The sudden, unbidden tightening. The relentless grip that seizes a muscle, twisting it into a knot of excruciating pain. For many, this isn’t an occasional nuisance but a recurring torment, disrupting sleep, sidelining athletic pursuits, and casting a shadow over daily comfort. Muscle cramps are a common affliction, yet their precise mechanisms and effective solutions often remain shrouded in a fog of folk remedies and hit-or-miss strategies. But what if the key to silencing these spasms lies not in complex pharmaceuticals or elaborate therapies, but in a humble, yet profoundly powerful mineral: magnesium?
This is the story of magnesium, the unsung hero in the symphony of our cellular mechanics, and its profound ability to bring peace to overactive muscles. It’s a story of discovery, of understanding the intricate dance of electrolytes, and of empowering individuals to reclaim control over their bodies. For the knowledgeable individual seeking not just relief, but comprehension, let us embark on a journey to unravel the mystery of muscle cramps and illuminate the transformative role of increased magnesium intake.
The Uninvited Guest: Understanding the Anatomy of a Cramp
Before we introduce our hero, magnesium, we must first understand the antagonist: the muscle cramp itself. Imagine the scene: you’re asleep, comfortably nestled, when suddenly, your calf muscle locks up, sending a searing jolt through your leg. Or perhaps you’re mid-marathon, pushing your limits, and your hamstring decides to stage a revolt. These are not mere twitches; they are sustained, involuntary contractions of a muscle or part of a muscle, often intensely painful, and frequently accompanied by visible hardening or bulging of the affected muscle.
Physiologically, a cramp is a malfunction of the neuromuscular junction. This is the critical communication point where a nerve fiber meets a muscle fiber. Normally, an electrical signal travels down the nerve, triggering the release of a chemical messenger (neurotransmitter, primarily acetylcholine) that tells the muscle to contract. After contraction, another signal or enzyme ensures relaxation. In a cramp, this delicate balance is disrupted. The muscle either receives an overstimulated signal, or it fails to receive the signal to relax, or both. The result is a prolonged, uncontrolled contraction that can last from seconds to minutes, leaving residual soreness and tenderness.
Cramps aren’t a monolithic phenomenon; they manifest in various forms:
- Nocturnal Leg Cramps: Perhaps the most common and disruptive, these typically occur in the calf or foot muscles during sleep, often waking sufferers with intense pain. Their etiology is frequently idiopathic (unknown), but dehydration, electrolyte imbalances, prolonged sitting, and certain medications are suspected contributors.
- Exercise-Associated Muscle Cramps (EAMC): A familiar foe for athletes, EAMC strikes during or immediately after physical exertion. Historically, it was solely attributed to dehydration and electrolyte loss through sweat. However, current research suggests a significant role for neuromuscular fatigue, where the nervous system loses its ability to properly regulate muscle contraction and relaxation. Electrolyte imbalances, including magnesium, still play a crucial supporting role.
- Rest Cramps: These can occur at any time, not necessarily during sleep or exercise, and might be indicative of underlying nutritional deficiencies or medical conditions.
- Dystonia and Tetany: While distinct from common muscle cramps, these conditions involve sustained muscle contractions or spasms and can sometimes be confused with severe cramping. Tetany, in particular, is often associated with severe electrolyte disturbances, including hypomagnesemia (low magnesium).
The impact of chronic cramping is far-reaching. Beyond the immediate agony, it leads to sleep deprivation, anxiety about future episodes, limitations on physical activity, and a general reduction in quality of life. Many sufferers feel helpless, trying various remedies with inconsistent results, yearning for a reliable solution.
Enter Magnesium: The Master Mineral
Now, let us introduce our protagonist: magnesium. This isn’t just another mineral; it’s a fundamental workhorse, a true "master mineral" involved in over 300 enzymatic reactions in the human body. Its omnipresence underscores its critical importance to virtually every physiological process.
Magnesium is the fourth most abundant mineral in the body, with about 60% stored in bones, 27% in muscle, and 6-7% in other cells, with less than 1% circulating in the blood. This distribution is crucial to understand, as serum magnesium levels (what’s typically measured in a blood test) may not accurately reflect total body magnesium stores.
Its functions are vast and varied:
- Energy Production: Magnesium is essential for the creation of adenosine triphosphate (ATP), the body’s primary energy currency. Without adequate magnesium, our cells cannot produce energy efficiently.
- Protein Synthesis: It’s a key component in the synthesis of proteins and nucleic acids, the building blocks of life.
- Nerve Function: Magnesium plays a critical role in nerve impulse transmission and the regulation of neuronal excitability. It helps stabilize nerve membranes.
- Blood Glucose Control: It influences insulin secretion and sensitivity, impacting blood sugar regulation.
- Blood Pressure Regulation: Magnesium contributes to maintaining healthy blood pressure by relaxing blood vessels.
- Bone Health: Along with calcium and vitamin D, magnesium is vital for bone formation and strength.
- DNA and RNA Synthesis: It’s integral to the replication and repair of our genetic material.
Given this extensive portfolio, it’s hardly surprising that magnesium would have a profound impact on muscle function. It’s not just a bystander; it’s a conductor in the intricate symphony of muscle contraction and relaxation.
The Neuromuscular Symphony: Magnesium’s Baton
To truly appreciate magnesium’s power against cramps, we must delve into its specific mechanisms within the neuromuscular system. Think of muscle contraction and relaxation as a finely choreographed dance, with various ions playing distinct roles.
1. The Calcium Antagonist: Ensuring Relaxation
This is perhaps magnesium’s most critical role in preventing cramps. Calcium is the primary ion responsible for muscle contraction. When a nerve signal arrives at the muscle, it triggers the release of calcium ions into the muscle cell. These calcium ions bind to specific proteins within the muscle fibers (troponin and tropomyosin), initiating a cascade of events that cause the muscle fibers to slide past each other, resulting in contraction.
Magnesium, in essence, acts as a natural calcium channel blocker. It competes with calcium for binding sites on these muscle proteins. When magnesium levels are adequate, it can effectively occupy some of these binding sites, preventing excessive calcium influx and thus promoting muscle relaxation. Without sufficient magnesium, calcium can flood the muscle cells unimpeded, leading to prolonged, uncontrolled contractions – precisely what a cramp is. Magnesium ensures that after the command to contract, the muscle also receives the command, and has the means, to relax. It’s the cellular bouncer that prevents calcium from overstaying its welcome.
2. ATP and Energy Metabolism: Powering Both Contraction and Relaxation
As mentioned, magnesium is indispensable for ATP production. While we often associate ATP with the energy required for muscle contraction, it’s equally vital for muscle relaxation. The active pumping of calcium ions out of the muscle cell, which is necessary for relaxation, is an energy-intensive process that requires ATP. If magnesium deficiency impairs ATP production, muscles may lack the energy needed to properly reset and relax after contraction, leading to sustained spasms. Magnesium ensures that the muscle has the fuel for both parts of the cycle.
3. Nerve Impulse Transmission: Stabilizing the System
Magnesium also plays a crucial role in stabilizing nerve membranes. It helps regulate the flow of other ions, such as sodium and potassium, across nerve cell membranes, which is essential for maintaining proper electrical potential. By stabilizing these membranes, magnesium helps prevent hyperexcitability of nerves. When nerves become overly excitable, they can fire erratically or excessively, sending inappropriate or overly strong signals to muscles, predisposing them to spasms and cramps. Magnesium acts like a dimmer switch, toning down overzealous nerve signals.
4. Electrolyte Balance: The Broader Picture
Magnesium doesn’t operate in a vacuum. It interacts synergistically with other electrolytes, particularly potassium and sodium, which are also critical for nerve and muscle function. Magnesium deficiency can disrupt the balance of these other electrolytes, further contributing to neuromuscular irritability. For instance, magnesium is required for the proper functioning of the sodium-potassium pump, an enzyme critical for maintaining the electrical gradient across cell membranes.
In essence, magnesium is the conductor ensuring harmony in the neuromuscular orchestra. When its levels are optimal, signals flow smoothly, contractions are controlled, and relaxation is complete. When magnesium is deficient, the orchestra becomes discordant, leading to the jarring, painful cacophony of a muscle cramp.
The Silent Scarcity: Why Magnesium Deficiency is So Common
Given magnesium’s profound importance, one might assume deficiencies would be rare. Unfortunately, the opposite is true. Magnesium deficiency, or hypomagnesemia, is surprisingly prevalent, with estimates suggesting that a significant portion of the population (up to 75% by some measures) may not be meeting their daily recommended intake. This silent scarcity is a complex issue rooted in several modern lifestyle factors:
- Soil Depletion: Decades of intensive farming practices have stripped essential minerals, including magnesium, from agricultural soils. Foods grown today may contain significantly less magnesium than those grown generations ago.
- Processed Foods: The modern diet is often rich in highly processed foods, which are notoriously poor sources of magnesium. Refining grains, for example, removes the magnesium-rich germ and bran.
- Chronic Stress: Stress, both physical and psychological, can increase magnesium excretion from the body. The "fight or flight" response demands more magnesium for energy and nerve function, leading to depletion if not replenished.
- Certain Medications: Diuretics, proton pump inhibitors (for acid reflux), antibiotics, and some chemotherapy drugs can interfere with magnesium absorption or increase its excretion.
- Alcohol Consumption: Alcohol acts as a diuretic, increasing the excretion of magnesium through the kidneys. Chronic alcohol abuse is a significant risk factor for deficiency.
- Gastrointestinal Issues: Conditions like Crohn’s disease, celiac disease, and chronic diarrhea can impair magnesium absorption.
- Diabetes: Individuals with diabetes often have increased magnesium excretion through the kidneys, especially if blood sugar is poorly controlled.
- Aging: As we age, magnesium absorption may decrease, and kidney function can become less efficient at conserving magnesium.
- Excess Calcium Intake: While calcium is vital, an excessively high intake without adequate magnesium can further exacerbate magnesium deficiency symptoms, as these two minerals need to be balanced.
The symptoms of magnesium deficiency extend far beyond muscle cramps. They can be subtle and wide-ranging, often mimicking other conditions, making diagnosis challenging. Besides muscle cramps and spasms, signs can include:
- Fatigue and Weakness: Due to impaired energy production.
- Anxiety and Depression: Magnesium plays a role in neurotransmitter regulation and stress response.
- Insomnia and Sleep Disturbances: Its calming effect on the nervous system is compromised.
- Headaches and Migraines: Often linked to neurological excitability.
- Heart Palpitations or Arrhythmias: Magnesium is crucial for proper heart muscle function.
- Numbness and Tingling: Due to nerve hyperexcitability.
- High Blood Pressure: Impaired blood vessel relaxation.
Given the prevalence of deficiency and the broad spectrum of its manifestations, it becomes clear why addressing magnesium intake is a powerful, foundational step toward better health, especially for those plagued by muscle spasms.
The Narrative Arc: From Suffering to Solution
Imagine the story of Sarah, a vibrant 45-year-old marketing executive. Her days are a blur of meetings, deadlines, and the occasional yoga class she squeezes in for sanity. But her nights are often punctuated by the searing pain of leg cramps. She wakes in agony, rubbing her calves, groaning in frustration. Sometimes it’s her foot, curling into an impossible knot. She’s tried everything: stretching before bed, drinking more water, even those bizarre "cramp relief" lotions. Nothing provides consistent relief. The fear of another cramp begins to overshadow the joy of sleep, leaving her perpetually tired and irritable.
Sarah’s story is the story of countless individuals. The desperate search for relief, the trial-and-error approach, the feeling of helplessness against an unseen force. Her doctor initially suggested potassium, then simply shrugged, advising more stretching. It wasn’t until a friend, a health-conscious marathon runner, casually mentioned magnesium that a new path opened up.
"Have you looked into magnesium?" her friend asked. "It helped me with my post-run cramps."
Skeptical but desperate, Sarah began to research. She learned about magnesium’s role in muscle relaxation, its common deficiency, and the subtle ways it impacts the body. The pieces started to click. She ate a reasonably healthy diet, but processed snacks were a frequent companion, and her stress levels were perpetually high. Could something so simple be the answer?
This moment of discovery – the realization that a fundamental nutritional imbalance might be the root cause – is the turning point for many. It’s the shift from passively enduring to actively understanding and implementing a solution.
Sarah started by consciously incorporating more magnesium-rich foods into her diet: a handful of almonds as a snack, spinach in her morning smoothie, a square of dark chocolate after dinner. She also decided to try a magnesium supplement, choosing a well-absorbed form.
The change wasn’t instantaneous, but it was perceptible. Within a week, the cramps became less frequent, less intense. Within a month, the nights of agony were replaced by unbroken sleep. The fear began to recede. Sarah felt a quiet revolution happening within her body, a sense of control returning. Her energy levels improved, her anxiety lessened, and she found herself feeling more grounded. The silence in the night, once a luxury, became her norm.
Strategic Magnesium Intake: Reclaiming Control
Sarah’s journey highlights the power of strategic magnesium intake. For those seeking to curb their cramps and embrace the full benefits of this mineral, a two-pronged approach – dietary and supplemental – is often the most effective.
1. Dietary Sources: The Foundation
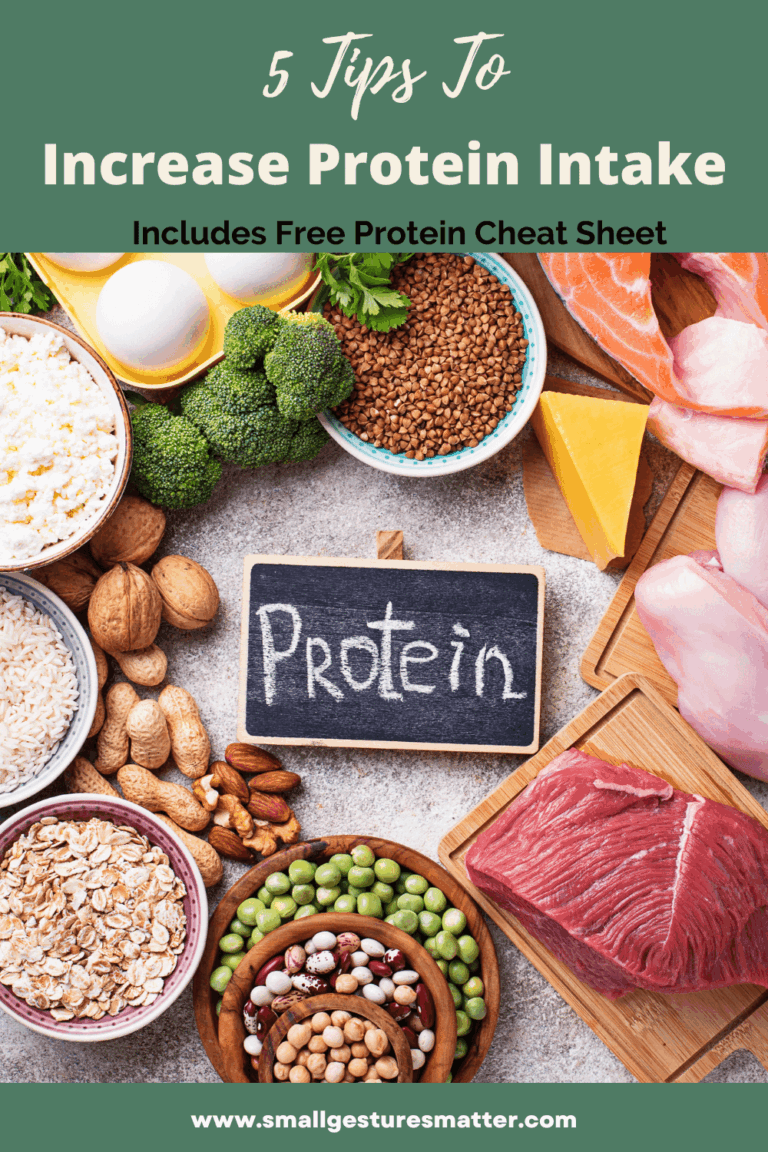
Food should always be the primary source of nutrients. Nature provides an abundance of magnesium-rich options:
- Leafy Green Vegetables: Spinach, kale, Swiss chard. These are packed with chlorophyll, which has a magnesium atom at its core.
- Nuts and Seeds: Almonds, cashews, pumpkin seeds, chia seeds, flax seeds. Excellent for snacking or adding to meals.
- Legumes: Black beans, lentils, chickpeas. Versatile and nutrient-dense.
- Whole Grains: Brown rice, quinoa, oats, whole wheat. Unlike refined grains, they retain their magnesium-rich germ and bran.
- Dark Chocolate: Yes, a delicious source! Look for varieties with 70% cocoa or higher.
- Avocados: A good source of healthy fats and magnesium.
- Bananas: While known for potassium, they also provide a decent amount of magnesium.
- Fatty Fish: Salmon, mackerel, halibut.
- Tofu: A plant-based protein source with good magnesium content.
Incorporating a variety of these foods into your daily diet is the first, crucial step. Aim for a diverse, whole-food-centric eating pattern.
2. Supplementation: When and How
Despite best efforts, dietary intake alone may not be sufficient for everyone, especially those with increased needs, compromised absorption, or persistent symptoms. This is where magnesium supplementation can be incredibly beneficial. However, not all magnesium supplements are created equal. Bioavailability – how well the body can absorb and utilize the magnesium – varies significantly between different forms.
Here are some common forms and their characteristics, crucial for a knowledgeable audience:
- Magnesium Citrate: One of the most common and bioavailable forms. It’s often used for its mild laxative effect, which can be beneficial for those with constipation, but can cause diarrhea in higher doses.
- Magnesium Glycinate (or Bisglycinate): Highly absorbable and generally well-tolerated, with a low risk of digestive upset. The glycine amino acid also has calming properties, making it an excellent choice for improving sleep and reducing anxiety, alongside muscle relaxation. Often considered the preferred form for addressing cramps and promoting overall well-being.
- Magnesium Malate: Often recommended for individuals with muscle pain, fatigue, and fibromyalgia. The malic acid can help with energy production. It’s well-absorbed and gentle on the stomach.
- Magnesium L-Threonate: This unique form has shown promise for its ability to cross the blood-brain barrier, making it potentially beneficial for cognitive function. While not directly targeted at muscle cramps, it can contribute to overall neurological health.
- Magnesium Taurate: Combines magnesium with the amino acid taurine, which also has calming effects and supports cardiovascular health. Good for heart health and muscle function.
- Magnesium Oxide: A very common and inexpensive form, but it has poor bioavailability (only about 4% absorption). Its primary use is as a laxative due to its osmotic effect in the gut. Not ideal for addressing systemic magnesium deficiency or muscle cramps.
- Magnesium Sulfate (Epsom Salts): Used topically in baths. While some magnesium can be absorbed through the skin, the extent and efficacy for systemic relief are debated. It can provide localized muscle relaxation and is generally safe.
Dosage and Timing:
The Recommended Dietary Allowance (RDA) for magnesium varies by age and sex, generally ranging from 310-420 mg per day for adults. However, therapeutic doses for addressing deficiency and symptoms like cramps may be higher, often ranging from 200-400 mg of elemental magnesium from supplements, in addition to dietary intake.
It’s often recommended to divide doses throughout the day to optimize absorption and minimize digestive upset. Taking magnesium in the evening can be particularly beneficial for nocturnal cramps and promoting sleep.
Factors Enhancing Absorption:
- Vitamin D: Adequate vitamin D levels are crucial for magnesium absorption and utilization.
- Vitamin B6: Some studies suggest B6 can enhance magnesium absorption.
- Selenium: Works synergistically with magnesium.
Safety and Considerations: A Responsible Approach
While magnesium is incredibly beneficial, it’s not without considerations. A knowledgeable approach demands respect for individual physiology and potential interactions.
Potential Side Effects: The most common side effect of oral magnesium supplementation, particularly in higher doses or with poorly absorbed forms like magnesium oxide, is diarrhea or loose stools. This is usually a sign that the dose is too high for your body. Reducing the dose or switching to a more bioavailable form (like glycinate or malate) can alleviate this.
Contraindications:
- Kidney Disease: Individuals with impaired kidney function should be extremely cautious with magnesium supplementation. Kidneys are responsible for excreting excess magnesium, and in compromised kidneys, magnesium can accumulate to toxic levels (hypermagnesemia), which can be dangerous.
- Heart Conditions: While magnesium is beneficial for heart health, individuals with severe heart block or other serious cardiac arrhythmias should consult their doctor before supplementing.
- Medication Interactions: Magnesium can interact with certain medications:
- Antibiotics: Some antibiotics (e.g., tetracyclines, quinolones) can have their absorption reduced by magnesium. Take magnesium supplements at least 2 hours apart from these medications.
- Diuretics: Some diuretics (e.g., loop and thiazide diuretics) can increase magnesium excretion, while potassium-sparing diuretics can increase magnesium retention.
- Proton Pump Inhibitors (PPIs): Long-term use of PPIs can lead to magnesium deficiency by reducing stomach acid needed for absorption.
- Blood Pressure Medications: Magnesium can have a blood-pressure-lowering effect, so combining it with antihypertensives might lead to excessively low blood pressure.
The Indispensable Role of a Healthcare Professional:
It cannot be stressed enough: always consult with a healthcare professional before starting any new supplement regimen, especially if you have underlying health conditions or are taking medications. A doctor can help assess your individual needs, rule out other causes of cramps, recommend appropriate forms and dosages, and monitor for potential interactions or side effects. While magnesium is a natural solution, it is a powerful one and should be approached with informed caution.
Beyond Magnesium: A Holistic Perspective
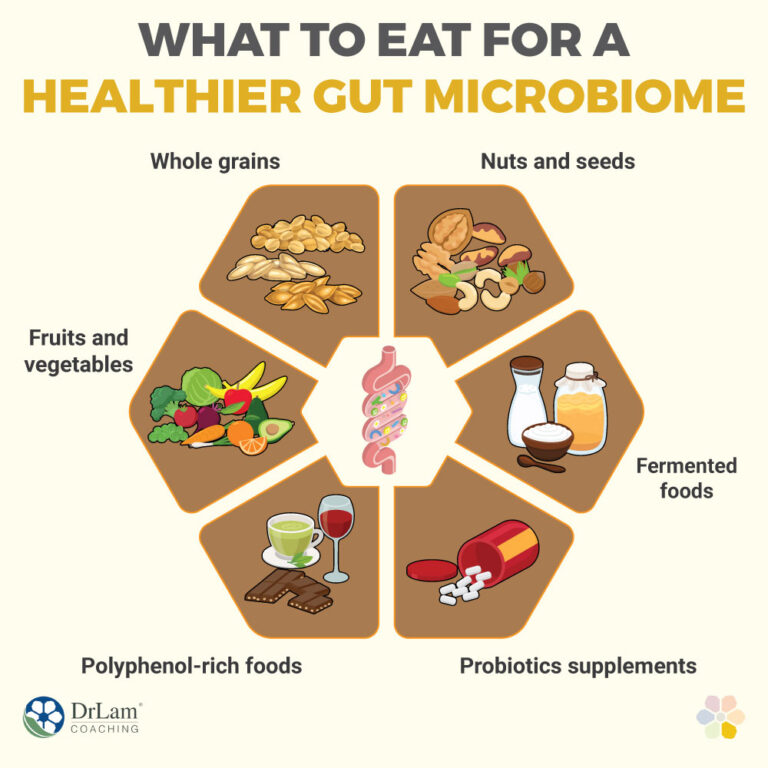
While magnesium stands out as a primary player in the fight against muscle cramps, it’s important to remember that the body is an interconnected system. A holistic approach often yields the best and most sustainable results.
- Hydration: Dehydration is a classic cramp trigger. Ensure adequate fluid intake throughout the day, especially during and after exercise. Water infused with a pinch of sea salt or a small amount of electrolyte powder can be beneficial.
- Other Electrolytes: While magnesium is key, sodium and potassium also play vital roles. Ensure your diet provides adequate potassium (bananas, potatoes, avocados, leafy greens) and that you’re not excessively restricting sodium, particularly if you’re an active individual who sweats a lot.
- Stretching and Flexibility: Regular stretching, especially of muscles prone to cramping, can improve flexibility and reduce muscle tightness. Gentle stretches before bed can be particularly helpful for nocturnal cramps.
- Warm-up and Cool-down: For exercise-associated cramps, proper warm-up before activity and a gradual cool-down afterwards can help prepare and recover muscles.
- Ergonomics and Posture: Prolonged sitting or standing in awkward positions can contribute to muscle fatigue and cramping. Adjust your workspace and take regular breaks to move.
- Address Underlying Medical Conditions: If cramps are persistent, severe, or accompanied by other concerning symptoms, it’s crucial to rule out underlying medical conditions such as peripheral artery disease, nerve compression, thyroid disorders, or diabetes.
Magnesium is a powerful piece of the puzzle, but it rarely acts alone. By integrating increased magnesium intake with these other healthy lifestyle practices, individuals can create a robust defense against the tyranny of muscle spasms.
Conclusion: Embracing the Silence
The story of muscle cramps is often one of frustration and pain, a battle against an invisible enemy. But with the knowledge of magnesium’s profound role, this narrative can shift dramatically towards one of empowerment and relief. Understanding how this humble mineral acts as a cellular bouncer, a nerve stabilizer, and an energy enabler transforms it from a mere supplement into a key player in our quest for physical well-being.
For the knowledgeable audience, the evidence is compelling: increasing magnesium intake, through a diet rich in whole foods and judicious supplementation when necessary, offers a scientifically sound and often profoundly effective strategy for silencing muscle spasms. It’s about restoring balance, providing the body with the fundamental tools it needs to function optimally, and allowing the neuromuscular symphony to play in perfect harmony.
The journey from suffering to silence is a personal one, and it begins with curiosity, understanding, and a willingness to explore the profound impact of foundational nutrition. By embracing the power of magnesium, we can reclaim our nights, enhance our athletic performance, and ultimately, live lives free from the sudden, unbidden grip of the cramp. The quiet revolution begins within, with the humble, yet mighty, mineral magnesium.