Zinc and PPIs: A Hidden Risk for Deficiency When Taking Acid-Reducing Medications
The Ubiquity and Efficacy of PPIs: A Medical Marvel
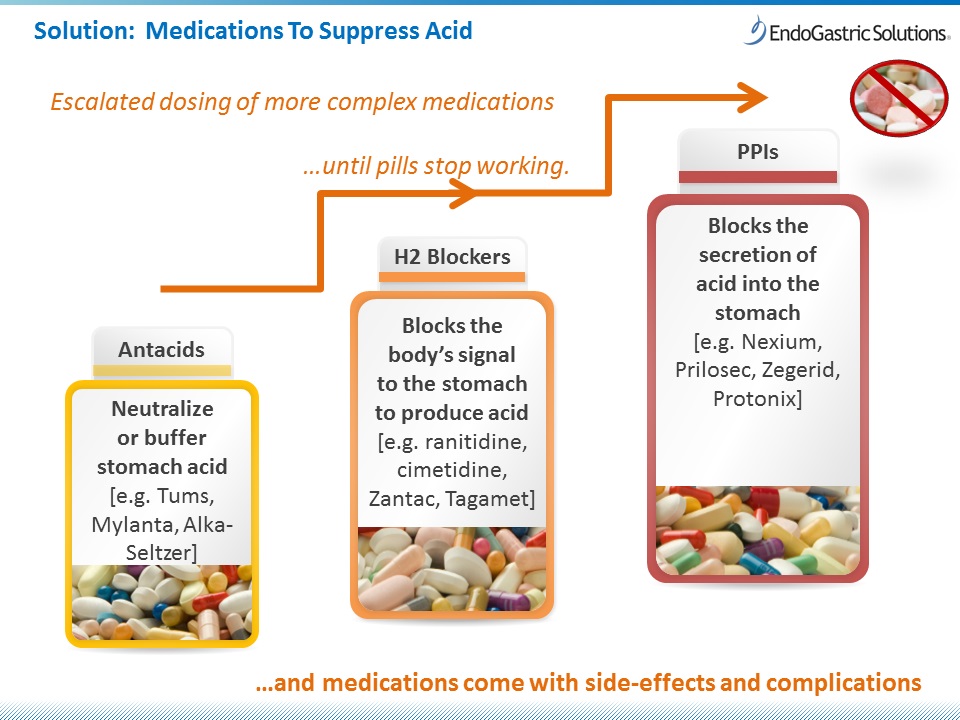
To understand the hidden risk, one must first appreciate the monumental impact of proton pump inhibitors. Introduced in the late 1980s, PPIs like omeprazole, lansoprazole, pantoprazole, esomeprazole, and rabeprazole revolutionized the treatment of acid-related gastrointestinal disorders. Before their advent, conditions like peptic ulcers, gastroesophageal reflux disease (GERD), and Zollinger-Ellison syndrome were often managed with less effective antacids, H2-receptor antagonists, or, in severe cases, even surgery. PPIs changed all that.
Their mechanism of action is elegantly precise: they irreversibly bind to and inhibit the H+/K+-ATPase enzyme, famously known as the "proton pump," located in the parietal cells of the stomach lining. This pump is the final common pathway for acid secretion, actively exchanging potassium ions into the cell for hydrogen ions (protons) expelled into the gastric lumen. By shutting down these pumps, PPIs effectively reduce gastric acid production by up to 95%, providing unparalleled relief from heartburn, promoting ulcer healing, and eradicating Helicobacter pylori in combination therapies.
The success of PPIs has been nothing short of phenomenal. They are among the most prescribed drugs globally, often viewed as a panacea for any upper GI discomfort. Millions rely on them daily, experiencing a significant improvement in their quality of life, freedom from chronic pain, and protection against severe complications like esophageal strictures or bleeding ulcers. Their efficacy is undeniable, and their role in modern gastroenterology is indispensable. Yet, like many powerful tools, their very success has led to widespread, and sometimes prolonged, use, paving the way for unforeseen consequences – the "hidden risks" that emerge only after years of extensive clinical experience and meticulous scientific inquiry.
Zinc: The Unsung Hero of the Human Body
Before delving into the collision, let us introduce the other protagonist in our story: zinc. Unlike the well-publicized calcium or iron, zinc often operates behind the scenes, a true unsung hero among essential trace elements. Despite its modest presence in the body (typically 2-3 grams in an adult), its influence is vast and pervasive. Zinc is not merely a mineral; it is a vital catalyst, a structural component, and a regulatory molecule involved in over 300 enzymatic reactions and more than 2,000 transcription factors. Its biological roles span virtually every major physiological system:
- Immune Function: Zinc is critical for the development and function of immune cells, including T-lymphocytes, B-lymphocytes, and natural killer cells. It plays a role in cytokine production, wound healing, and resistance to infection. Deficiency impairs both innate and adaptive immunity, rendering individuals more susceptible to pathogens.
- Enzymatic Activity: As a cofactor, zinc is integral to enzymes involved in metabolism (carbohydrate, protein, lipid), DNA and RNA synthesis, and antioxidant defense (e.g., superoxide dismutase).
- DNA Synthesis and Cell Division: Essential for cell growth, division, and repair, zinc is crucial during periods of rapid growth, such as childhood, pregnancy, and wound healing.
- Neurotransmitter Function and Cognitive Health: Zinc is found in high concentrations in the brain and plays a role in synaptic transmission, neuronal plasticity, and mood regulation. It’s implicated in conditions ranging from depression to neurodegenerative diseases.
- Sensory Function: Zinc is vital for the proper functioning of taste buds and olfactory receptors, explaining why deficiency often leads to altered taste (dysgeusia) and smell (anosmia).
- Hormone Regulation: It influences the production and function of various hormones, including insulin, thyroid hormones, and sex hormones, impacting metabolism, fertility, and reproductive health.
- Skin Integrity and Wound Healing: Zinc is necessary for collagen synthesis, cell proliferation, and anti-inflammatory processes crucial for maintaining healthy skin and facilitating wound repair.
- Antioxidant Defense: It acts as an antioxidant and stabilizes cell membranes, protecting against oxidative stress, a key contributor to aging and chronic disease.
Given its myriad roles, a deficiency in zinc does not manifest as a single, distinct ailment but rather as a constellation of non-specific symptoms, a "silent saboteur" undermining multiple bodily functions. This non-specificity makes zinc deficiency particularly challenging to diagnose, especially when its onset is gradual and its underlying cause, like long-term PPI use, remains unsuspected.
The Collision: How PPIs Impair Zinc Absorption
The stage is set. On one side, the powerful acid-suppressing PPIs; on the other, the indispensable, yet often overlooked, zinc. Their collision point lies in the stomach, specifically in the critical initial step of zinc absorption.
Zinc from dietary sources (red meat, poultry, seafood, legumes, nuts, whole grains) typically exists in various forms, often bound to proteins or complexed with phytates. For zinc to be absorbed in the small intestine, it must first be liberated from these complexes and solubilized into its ionic form (Zn2+). This crucial process is heavily dependent on the acidic environment of the stomach.
Here’s the mechanism of impairment:
- Gastric Acid as a Liberator: Stomach acid (hydrochloric acid) plays a pivotal role in denaturing proteins and breaking down food matrices. This acidic environment facilitates the release of zinc ions from their dietary ligands, making them available for absorption. Without sufficient acid, zinc remains trapped or bound, rendering it biologically unavailable.
- PPIs Neutralize the Environment: By effectively shutting down the proton pumps, PPIs drastically reduce gastric acid secretion, raising the pH of the stomach. This hypochlorhydria (low stomach acid) or achlorhydria (absence of stomach acid) directly impedes the liberation of zinc ions.
- Reduced Solubility and Increased Chelation: In a less acidic environment, zinc’s solubility decreases, and it becomes more prone to binding with other dietary components, particularly phytates (found in grains and legumes) and oxalates, which can chelate zinc, forming insoluble complexes that cannot be absorbed and are instead excreted.
- Potential Impact on Transporters: While gastric acid is the primary factor, some research also suggests that PPIs might indirectly affect the expression or function of zinc transporters (like ZIP4, which imports zinc into enterocytes, or ZnT1, which exports zinc out of enterocytes) in the small intestine. However, the direct impact of altered pH on these transporters is still an area of ongoing investigation.
- Small Intestinal Bacterial Overgrowth (SIBO): Chronic PPI use can also alter the gut microbiome, leading to SIBO. An overgrowth of bacteria in the small intestine can consume nutrients, including zinc, or interfere with its absorption through inflammatory processes or changes in the intestinal milieu.
The result is a subtle, chronic malabsorption of zinc. It’s not an acute poisoning, but rather a slow, steady depletion of the body’s zinc stores, much like a leaky faucet gradually emptying a reservoir. For individuals on short-term PPI therapy, this might not pose a significant risk, as the body’s homeostatic mechanisms can compensate. However, for the millions who use PPIs long-term – often for years or even decades – the cumulative effect can lead to a clinically significant zinc deficiency, often before any overt symptoms manifest.
The Silent Sabotage: Manifestations of Zinc Deficiency
The insidious nature of PPI-induced zinc deficiency lies in its non-specific and often delayed symptom presentation. The body has remarkable compensatory mechanisms, and zinc stores are not depleted overnight. This means that symptoms may emerge gradually, often years into PPI therapy, making the causal link difficult to establish without a high index of suspicion. Patients and even clinicians may attribute these vague complaints to aging, stress, or other co-morbidities. This is the "silent sabotage" at play.
The manifestations can be widespread, reflecting zinc’s diverse physiological roles:
- Immune Compromise: This is one of the most common and concerning effects. Patients may experience increased frequency and severity of infections (colds, flu, pneumonia), slower recovery from illness, and impaired vaccine response. Wounds may heal poorly, and skin infections can become more persistent.
- Dermatological Issues: Zinc is crucial for skin health. Deficiency can lead to various skin conditions, including persistent rashes (often mistaken for eczema or psoriasis), dry and flaky skin, acne that doesn’t respond to conventional treatments, and slow wound healing. Hair loss (alopecia) and brittle nails are also common.
- Gastrointestinal Distress: Paradoxically, while PPIs are used for GI issues, long-term use leading to zinc deficiency can exacerbate or introduce new GI problems. This includes chronic diarrhea, malabsorption of other nutrients, and increased intestinal permeability ("leaky gut"). The gut-immune axis is heavily dependent on zinc, and its deficiency can perpetuate a vicious cycle of inflammation.
- Neurological and Psychological Symptoms: Zinc plays a role in neurotransmission and brain function. Deficiency can manifest as fatigue, lethargy, impaired memory and concentration ("brain fog"), mood disturbances (irritability, anxiety, depression), and even peripheral neuropathy.
- Sensory Impairments: Altered taste (dysgeusia) and smell (anosmia) are classic, though often ignored, symptoms of zinc deficiency. Food may taste bland, metallic, or simply "off," leading to reduced appetite and potentially further nutritional deficiencies.
- Reproductive Health: In men, zinc is essential for sperm production and testosterone synthesis, and deficiency can lead to reduced libido and infertility. In women, it can affect ovarian function and fetal development during pregnancy.
- Growth Retardation: In children, severe zinc deficiency can lead to stunted growth and delayed sexual maturation. While less common in adults, chronic low-grade deficiency can still impact tissue repair and regeneration.
- Ocular Health: Zinc is found in high concentrations in the eye, particularly the retina. Deficiency can contribute to impaired night vision and potentially accelerate age-related macular degeneration.
The challenge lies in recognizing this constellation of symptoms as a potential sign of zinc deficiency, especially in a patient who has been on PPIs for an extended period. The elderly are particularly vulnerable due to often lower dietary intake, multiple co-morbidities, and polypharmacy, which can further complicate diagnosis.
The Diagnostic Dilemma and Clinical Challenges
Diagnosing zinc deficiency is notoriously difficult, primarily because serum zinc levels, the most commonly available test, do not accurately reflect total body zinc stores. Zinc is primarily an intracellular mineral, tightly regulated by homeostatic mechanisms. When dietary intake is insufficient, the body initially mobilizes zinc from less critical tissues (like bone or muscle) to maintain serum levels within the normal range. Therefore, a "normal" serum zinc level does not necessarily rule out a functional deficiency or ongoing depletion.
More accurate, but less routinely available, diagnostic methods include:
- Erythrocyte or Leukocyte Zinc: These tests can provide a better indicator of intracellular zinc status but are more complex and expensive.
- Urinary Zinc Excretion: While useful for monitoring zinc status, it can be influenced by renal function and other factors.
- Hair Zinc Analysis: Can reflect long-term zinc status but is subject to external contamination and variability.
- Functional Tests: Observing improvement in symptoms or immune markers after zinc supplementation can be a practical diagnostic approach, though not a direct measure of deficiency.
Given these diagnostic limitations, clinicians must rely heavily on a high index of suspicion, a thorough patient history (including medication review and dietary habits), and an understanding of the risk factors. For patients on long-term PPI therapy, particularly those presenting with unexplained fatigue, recurrent infections, skin issues, or altered taste/smell, zinc deficiency should be on the differential diagnosis.
Navigating the Solution: Management and Mitigation
Once PPI-induced zinc deficiency is suspected or confirmed, a multi-pronged approach is necessary, always under medical supervision. The goal is to restore zinc levels, alleviate symptoms, and critically, re-evaluate the necessity of ongoing PPI therapy.
- Re-evaluating PPI Therapy (Deprescribing): This is perhaps the most crucial step. Many patients are on PPIs long-term without a clear, ongoing indication. PPIs are often initiated for acute conditions (e.g., H. pylori eradication, stress ulcer prophylaxis) and then continued indefinitely without periodic review. For these patients, a supervised deprescribing strategy may be appropriate. This involves gradually tapering the PPI dose to prevent rebound acid hypersecretion, which can cause severe heartburn and lead patients to restart the medication. Lifestyle modifications (dietary changes, weight loss, elevating the head of the bed) can support this process.
- Dietary Interventions: Increasing dietary intake of zinc-rich foods is a foundational strategy. Excellent sources include:
- Animal Sources: Red meat (beef, lamb, pork), poultry (chicken, turkey), oysters (exceptionally high), other seafood (crab, lobster). Animal sources contain highly bioavailable zinc.
- Plant Sources: Legumes (lentils, chickpeas, beans), nuts (cashews, almonds), seeds (pumpkin, sesame), whole grains, dairy products, eggs. Plant-based zinc absorption can be hindered by phytates, but soaking, sprouting, and fermentation can reduce phytate content.
- Zinc Supplementation: For those with confirmed deficiency or high risk, dietary changes alone may not be sufficient. Zinc supplementation can be highly effective.
- Forms: Various forms are available, including zinc gluconate, zinc picolinate, zinc citrate, and zinc sulfate. Zinc picolinate is often touted for better absorption, though more research is needed.
- Dosage: Doses typically range from 15-30 mg elemental zinc per day for deficiency, with higher doses used for short periods under medical guidance. Excessive zinc intake can lead to copper deficiency and other adverse effects, so careful monitoring is essential.
- Timing: Zinc supplements are best taken with food to minimize gastrointestinal upset, but away from iron supplements, which can compete for absorption.
- Monitoring: Regular monitoring of zinc levels (if reliable tests are available and clinically indicated) and symptom improvement is crucial. This helps adjust supplementation doses and assess the effectiveness of interventions.
- Addressing Co-factors: Ensure adequate intake of other nutrients that support zinc metabolism and overall gut health, such as B vitamins, magnesium, and vitamin D.
Broader Implications and Future Directions
The story of PPIs and zinc deficiency is more than just an isolated medical anecdote; it reflects broader themes in modern healthcare:
- The Double-Edged Sword of Therapeutic Success: Powerful drugs, while offering immense benefits, often come with unforeseen long-term consequences that only emerge with widespread and prolonged use. This underscores the need for continuous pharmacovigilance and critical evaluation of medication necessity.
- The Importance of Micronutrients: This narrative highlights the often-underestimated role of essential micronutrients in maintaining health. Their deficiencies can have widespread and debilitating effects, often masked by non-specific symptoms.
- The Challenge of Polypharmacy: Many patients on long-term PPIs are also on multiple other medications, increasing the risk of drug-nutrient interactions and complex symptom presentations.
- Patient Empowerment and Education: Patients need to be informed about the potential risks of long-term PPI use and encouraged to discuss their medication regimen with their healthcare providers regularly. Awareness of potential symptoms of zinc deficiency can prompt earlier investigation.
- Need for Robust Research: While observational studies and case reports have established a clear link, larger, prospective, randomized controlled trials are needed to precisely quantify the risk of zinc deficiency in various PPI user populations, identify specific risk factors, and determine optimal screening and management strategies.
In conclusion, the widespread reliance on proton pump inhibitors, while offering immense therapeutic benefits for acid-related disorders, carries a hidden risk for zinc deficiency. This silent sabotage, orchestrated by the chronic suppression of gastric acid, can gradually deplete the body of an essential micronutrient, leading to a myriad of non-specific symptoms that compromise immune function, skin integrity, cognitive health, and overall well-being.
For the knowledgeable audience, this story serves as a critical reminder that even the most effective medications are not without their nuanced complexities. It calls for a paradigm shift from indefinite PPI prescription to thoughtful, evidence-based use, regular re-evaluation, and proactive monitoring for potential nutrient deficiencies. It underscores the profound interconnectedness of our physiological systems and the delicate balance required to maintain health. By bringing this hidden risk into the light, we empower both clinicians and patients to make more informed decisions, ensuring that the quest for relief from one ailment does not inadvertently pave the way for another, silently undermining the very foundations of health. The tale of zinc and PPIs is a compelling argument for vigilance, holistic understanding, and a renewed appreciation for the unsung heroes of our biochemistry.