Beyond the Label: The Unseen Tapestry of Zinc Interactions
A Prologue: The Unraveling
Dr. Aris Thorne, a seasoned pharmacologist with a reputation for solving medical enigmas, stared at the latest lab results. His patient, Mrs. Eleanor Vance, a sprightly woman in her late sixties, presented a baffling constellation of symptoms: persistent fatigue, recurrent infections, a curious loss of taste and smell, and oddly, slow-healing skin lesions. Her diet was exemplary, her adherence to prescribed medications – a proton pump inhibitor for reflux, a thiazide diuretic for mild hypertension, and a daily multivitamin – was impeccable. Yet, Eleanor was slowly, inexplicably, declining.
"It’s like a thread is missing from the fabric of her health," Aris mused aloud to his junior colleague, Dr. Lena Sharma. "Every conventional avenue has been explored. What are we overlooking?"
Lena, still buzzing with the idealism of youth, pointed to a subtle anomaly in Eleanor’s trace mineral panel: zinc levels, while technically within the "normal" range, were at the very bottom, consistently. "Could it be subclinical zinc deficiency, Dr. Thorne? Despite the multivitamin?"
Aris nodded slowly, a spark igniting in his eyes. "Subclinical deficiency is often the most insidious. But why? And more importantly, how can a woman taking a multivitamin still be teetering on the edge of a zinc deficit? This isn’t just about what’s on the label, Lena. This is about what’s hidden."
And so began their journey into the intricate, often overlooked world of zinc interactions – a world where seemingly innocuous choices, dietary habits, and prescribed medications can silently conspire to undermine the body’s delicate biochemical balance. It’s a story not just of a single element, but of the profound interconnectedness of biological systems, a narrative of vigilance, scientific detective work, and the constant quest for personalized medicine.
The Architect of Life: Zinc’s Indispensable Role
To truly appreciate the gravity of zinc interactions, one must first grasp the sheer ubiquity and indispensability of this humble trace mineral. Often overshadowed by flashier nutrients, zinc is, in essence, an architect of life, a silent orchestrator involved in over 300 enzymatic reactions and playing structural roles in countless proteins. It is not merely a cofactor; it is an intrinsic component of the machinery that governs cellular function, immunity, and overall well-being.
Consider its diverse portfolio:
- Immune System Sentinel: Zinc is critical for the development and function of immune cells, including T-lymphocytes and natural killer cells. A deficiency can dramatically impair both innate and adaptive immunity, leading to increased susceptibility to infections, much like Eleanor’s recurrent bouts.
- Genetic Guardian: It’s vital for DNA and RNA synthesis, cell division, and protein synthesis. Without adequate zinc, cellular repair and replication falter, impacting everything from wound healing to growth.
- Sensory Steward: Zinc is essential for the function of taste buds and olfactory receptors. Its deficiency can lead to altered or lost senses of taste and smell – another of Eleanor’s perplexing symptoms.
- Antioxidant Ally: As a component of superoxide dismutase (SOD), a powerful antioxidant enzyme, zinc helps protect cells from oxidative damage, a cornerstone of aging and chronic disease.
- Metabolic Maestro: It plays a role in carbohydrate, fat, and protein metabolism, influencing insulin signaling and thyroid function.
- Structural Integrator: Zinc stabilizes cell membranes and is crucial for the structural integrity of various proteins, including those involved in collagen formation, explaining its role in wound healing.
Given this expansive and critical role, even a subtle disruption in zinc homeostasis can ripple through multiple physiological systems, manifesting as a seemingly unrelated array of symptoms. The challenge lies in connecting these disparate threads, in seeing beyond the obvious and delving into the "hidden ingredients" – those dietary components, OTC remedies, and prescription medications that silently sabotage zinc’s vital work.
The Silent Saboteurs: Hidden Ingredients in Our Daily Lives
The concept of "hidden ingredients" often conjures images of obscure chemicals in processed foods. While valid, in the context of zinc interactions, it extends far beyond that, encompassing naturally occurring compounds, seemingly benign supplements, and even the very water we drink. These are the elements that, unbeknownst to us, can diminish zinc’s bioavailability, absorption, or increase its excretion.
1. Dietary Demolishers: The Plant Kingdom’s Double-Edged Sword
Our dietary choices, even the most healthful ones, can sometimes be unwitting antagonists to zinc absorption.
- Phytates (Phytic Acid): Found abundantly in whole grains, legumes, nuts, and seeds, phytates are nature’s way of storing phosphorus. However, they possess a strong chelating affinity for divalent cations like zinc, iron, and calcium. When ingested, phytates bind to zinc in the gastrointestinal tract, forming insoluble complexes that the body cannot absorb.
- The Story: A health-conscious individual like Eleanor, diligently consuming a diet rich in whole-wheat bread, oats, beans, and lentils, could, paradoxically, be hindering her zinc uptake. While soaking, sprouting, and fermenting these foods can reduce phytate content, many modern preparation methods do not fully eliminate this interaction. This becomes particularly problematic for vegetarians and vegans who rely heavily on these plant-based staples. The "health halo" around these foods often obscures their potential to impact mineral absorption.
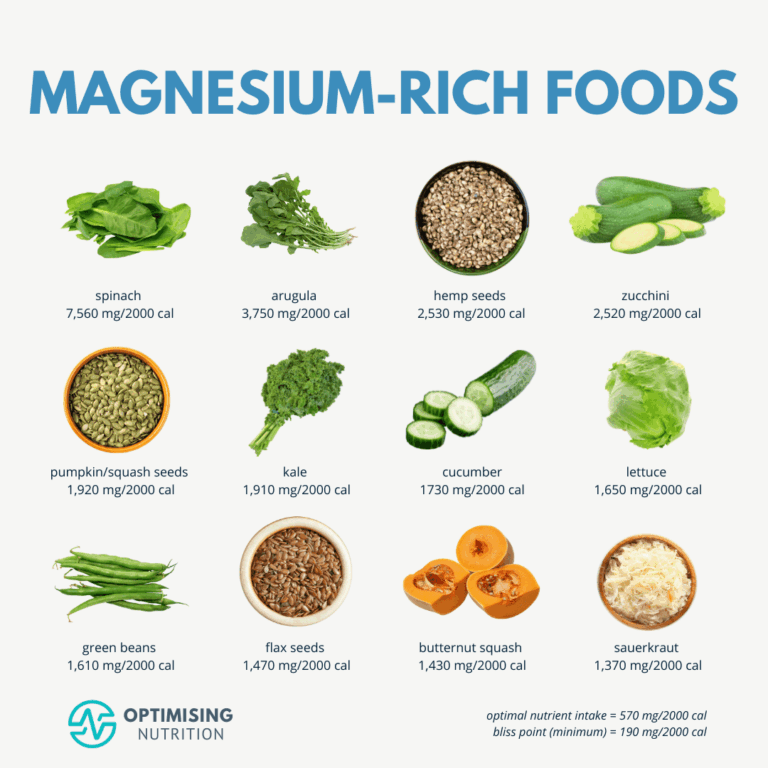
- Oxalates: Present in spinach, rhubarb, beet greens, and cocoa, oxalates can also bind to zinc, forming insoluble salts and impeding absorption. While less potent than phytates, their cumulative effect in a diet rich in these vegetables can be significant.
- Tannins: Found in tea, coffee, and some fruits and legumes, tannins are polyphenolic compounds that can complex with minerals, including zinc, making them less available for absorption. The morning cup of coffee or evening tea, while offering antioxidant benefits, might subtly be interfering with the zinc from breakfast or dinner.
- Dietary Fiber: While crucial for gut health, excessive insoluble fiber can sometimes reduce mineral absorption by accelerating transit time or non-specifically binding to minerals.
2. Mineral Minefields: When Good Intentions Go Awry
The pursuit of optimal health often involves supplementation. However, the mineral kingdom is a delicate ecosystem, and introducing one in excess can disrupt the balance of others.
- Iron Overload: Iron and zinc share common absorption pathways in the intestine. High-dose iron supplements, often prescribed for anemia or taken by women of childbearing age, can competitively inhibit zinc absorption.
- The Story: Eleanor, a diligent multivitamin user, might also be taking an iron supplement based on a previous, mild anemic episode. Unbeknownst to her, the very supplement meant to boost her iron could be subtly undermining her zinc status, especially if taken simultaneously or in close proximity. This highlights the importance of staggered dosing for certain minerals.
- Calcium Overload: While less direct than iron, very high doses of calcium supplements can also interfere with zinc absorption, particularly when phytates are also present, by forming insoluble calcium-zinc-phytate complexes.
- Copper Competition: This is a classic example of mineral antagonism. Zinc and copper share transporters (e.g., DMT1, CTR1, metallothionein) and compete for absorption. High-dose zinc supplementation (e.g., for immune support during a cold) can induce copper deficiency over time, and conversely, excessive copper can impair zinc absorption. This delicate balance underscores the need for careful consideration in mineral supplementation strategies.
3. Environmental & Lifestyle Factors: Unseen Pressures
Beyond food and supplements, other "hidden ingredients" from our environment and lifestyle can also influence zinc status.
- Alcohol Consumption: Chronic alcohol intake is a significant factor in zinc deficiency. Alcohol increases urinary zinc excretion and can also impair intestinal absorption and hepatic storage of zinc. The lifestyle choices of a patient, though seemingly unrelated to their symptoms, can be powerful determinants of micronutrient status.
- Heavy Metals: Exposure to heavy metals like cadmium and lead can interfere with zinc metabolism and displace it from its binding sites, disrupting its physiological functions. While less common, it’s a factor to consider in certain occupational or environmental exposures.
- EDTA (Ethylenediaminetetraacetic Acid): While used therapeutically as a chelating agent for heavy metal poisoning, EDTA is also used as a food additive (e.g., in canned foods, dressings) to prevent discoloration. Its strong chelating properties can bind to dietary zinc, reducing its bioavailability.
The Pharmacological Labyrinth: Drug Classes and Zinc Interactions
The most complex and often overlooked "hidden ingredients" are the very medications designed to improve health. The intricate dance between xenobiotics (drugs) and endogenous micronutrients is a vast field of study, and zinc, being so central to cellular function, is particularly susceptible to these pharmacological perturbations. Dr. Thorne knew this was where the true detective work lay for Eleanor.
1. The Antibiotic Arsenal: Collateral Damage to Absorption
Certain classes of antibiotics, while vital for fighting infections, are notorious for their ability to chelate divalent cations, including zinc.
- Tetracyclines (e.g., Doxycycline, Minocycline): These broad-spectrum antibiotics form stable, insoluble complexes with zinc in the gastrointestinal tract. This chelation significantly reduces the absorption of both the antibiotic and the zinc.
- The Story: A patient like Eleanor, who might have been prescribed doxycycline for a skin infection or a respiratory issue, could experience a temporary, but significant, dip in zinc absorption. If this happens repeatedly or in an already marginally deficient individual, the cumulative effect can be detrimental. The advice to avoid dairy products (calcium) with tetracyclines is well-known, but the same caution often isn’t extended to zinc-containing foods or supplements.
- Quinolones (e.g., Ciprofloxacin, Levofloxacin): Similar to tetracyclines, quinolone antibiotics also chelate zinc (and other divalent cations like magnesium and calcium). This interaction reduces the bioavailability of both the drug and the mineral.
- The Story: If Eleanor had taken ciprofloxacin for a urinary tract infection, this interaction could have further exacerbated her zinc deficit. The standard clinical advice emphasizes separation from antacids and dairy, but often overlooks the broader implication for other mineral-rich foods or supplements.
Mechanism: Chelation. The antibiotic molecules possess functional groups that can bind to metal ions, forming a complex that is too large or too insoluble to be absorbed across the intestinal wall.
Clinical Implication: Patients on these antibiotics should be advised to take zinc supplements or zinc-rich foods at least 2-4 hours before or after their medication dose to minimize interaction.
2. Gastric Acid Modulators: Altering the pH Balance
Many drugs alter the pH of the stomach, which can profoundly impact the solubility and subsequent absorption of minerals. Zinc, in its ionized form, is more readily absorbed.
- Proton Pump Inhibitors (PPIs) (e.g., Omeprazole, Pantoprazole) and H2 Receptor Blockers (e.g., Ranitidine, Famotidine): These medications reduce gastric acid production, raising stomach pH. While effective for acid reflux, this altered environment can decrease the solubility of zinc salts, hindering their absorption.
- The Story: Eleanor’s chronic use of a PPI for reflux suddenly takes on a new significance. For years, this medication, essential for her comfort, might have been silently chipping away at her zinc status by creating an environment less conducive to its absorption. This is a classic example of a chronic medication causing a subtle, long-term micronutrient depletion that goes unnoticed until symptoms become pronounced.
- Antacids (e.g., Aluminum Hydroxide, Calcium Carbonate): Over-the-counter antacids rapidly neutralize stomach acid. While a short-term solution for heartburn, chronic use can mirror the effects of PPIs, reducing zinc solubility and potentially chelating it (especially aluminum-containing antacids).
Mechanism: Altered gastric pH. Zinc absorption is optimal in an acidic environment where zinc ions are readily released from food complexes. Reducing stomach acidity can hinder this process.
Clinical Implication: For patients on long-term PPIs or H2 blockers, regular monitoring of zinc status and consideration of zinc supplementation, potentially in a chelated form less reliant on gastric acid, is warranted. Staggering antacid use from zinc-rich meals is also advisable.
3. Diuretics: Flushing Away Vital Minerals
Diuretics, commonly prescribed for hypertension and edema, increase the excretion of water and electrolytes, but some can also increase the urinary excretion of trace minerals.
- Thiazide Diuretics (e.g., Hydrochlorothiazide): While primarily affecting sodium and chloride reabsorption, thiazides can also increase the urinary excretion of zinc.
- The Story: Eleanor’s thiazide diuretic, a staple for her mild hypertension, adds another layer to her zinc deficit. The very drug meant to protect her cardiovascular health could be quietly depleting a mineral essential for her immune function and other vital processes.
- Loop Diuretics (e.g., Furosemide): These powerful diuretics also increase the excretion of various minerals, including zinc, due to their action on the renal tubules.
Mechanism: Increased urinary excretion. Diuretics interfere with the reabsorption of minerals in the kidneys, leading to their loss in urine.
Clinical Implication: Long-term use of diuretics, especially in elderly or at-risk populations, necessitates monitoring of electrolyte and trace mineral levels. Supplementation may be required.
4. ACE Inhibitors: A Complex Relationship
Angiotensin-converting enzyme (ACE) inhibitors (e.g., Lisinopril, Enalapril) are cornerstones in managing hypertension and heart failure. Their interaction with zinc is more nuanced.
- Zinc Depletion/Redistribution: ACE inhibitors can potentially increase urinary zinc excretion and/or redistribute zinc within the body, leading to decreased plasma zinc levels. The ACE enzyme itself contains zinc, and some theories suggest that ACE inhibitors might complex with zinc, altering its bioavailability or leading to its increased excretion.
- Altered Taste (Dysgeusia): A known side effect of ACE inhibitors, dysgeusia, often manifests as a metallic or blunted taste. This side effect is also a hallmark of zinc deficiency, leading to speculation that the drug-induced taste disturbance might be mediated, in part, by its effect on zinc.
- The Story: Eleanor’s loss of taste and smell, initially attributed to aging, could be a confluence of factors: her low zinc status and the potential impact of her ACE inhibitor on zinc metabolism. This highlights the synergistic nature of these interactions.
Mechanism: Complex; possibly increased urinary excretion, altered zinc metabolism, or direct interaction with zinc-dependent enzymes.
Clinical Implication: While not all patients on ACE inhibitors experience zinc depletion, monitoring for taste disturbances and considering zinc status in symptomatic individuals is prudent.
5. Other Notable Drug Classes
- Corticosteroids (e.g., Prednisone): Long-term corticosteroid use can lead to increased urinary zinc excretion and decreased plasma zinc levels. They can also affect zinc distribution and cellular uptake.
- Chelating Agents (e.g., Penicillamine): Used in conditions like Wilson’s disease (copper overload) or rheumatoid arthritis, penicillamine is designed to bind metals. While beneficial for its intended purpose, it is non-specific and can lead to significant zinc depletion if not carefully managed.
- Immunosuppressants (e.g., Cyclosporine): Used in organ transplant patients, cyclosporine has been associated with altered trace element metabolism, including zinc.
- Oral Contraceptives: Some studies suggest that oral contraceptives can alter zinc metabolism, though findings are mixed and the clinical significance is often debated.
- Anticonvulsants (e.g., Valproate): Certain anticonvulsant medications can affect the metabolism of various trace elements, including zinc, potentially leading to lower plasma levels.
The Clinical Detective: Navigating the Interconnected Web
The case of Eleanor Vance, and countless others like her, underscores the immense challenge in identifying and managing these hidden interactions. It’s a journey that demands clinical acumen, a deep understanding of biochemistry and pharmacology, and an empathetic ear for the patient’s narrative.
1. Beyond the Lab Norms: The Subclinical Spectrum
One of the greatest hurdles is the interpretation of laboratory results. Plasma zinc levels, while commonly measured, are not always a reliable indicator of total body zinc status due to tightly regulated homeostatic mechanisms. A "normal" plasma zinc might mask a subclinical deficiency, especially when symptoms point strongly towards it. Tissue zinc levels (e.g., in hair or white blood cells) can offer a more accurate picture but are not routinely available.
Dr. Thorne’s decision to focus on Eleanor’s consistently low-normal zinc, combined with her symptom profile, was key. It’s a testament to the idea that clinical context often trumps isolated numerical values.
2. The Power of a Comprehensive History
The cornerstone of identifying these interactions lies in a meticulous patient history. This goes far beyond current medications and major diagnoses. It delves into:
- Dietary Habits: Detailed food intake, including frequency of whole grains, legumes, specific vegetables, and consumption of coffee/tea/alcohol.
- Supplement Use: Every over-the-counter supplement, herbal remedy, and multivitamin.
- Past Medication History: Even drugs taken years ago could have contributed to a gradual depletion.
- Lifestyle Factors: Smoking, alcohol, environmental exposures.
- Symptom Onset and Duration: Correlating symptoms with the initiation of new medications or dietary changes.
3. Interdisciplinary Collaboration: A Team Effort
Solving these complex cases often requires a collaborative approach. Pharmacists can provide invaluable insights into drug-drug and drug-nutrient interactions. Registered dietitians can meticulously analyze dietary patterns and suggest modifications. Laboratory specialists can help interpret nuanced trace element results. The "story" of the patient becomes a collective narrative, pieced together by multiple experts.
4. The Art of Deprescribing and Re-evaluating
For Eleanor, Dr. Thorne and Lena embarked on a careful re-evaluation of her medication regimen. Was the PPI still absolutely necessary at its current dose? Could the diuretic be adjusted or replaced? They explored staggering her multivitamin and any potential iron supplements away from meals and other medications. They also provided detailed dietary counseling, not to eliminate healthy foods, but to optimize preparation methods and timing.
5. Personalized Medicine: The Ultimate Goal
Ultimately, the journey "beyond the label" is a quest for personalized medicine. No two patients are identical, and their unique genetic makeup, lifestyle, comorbidities, and medication profiles create a bespoke biochemical environment. Understanding these hidden interactions moves us closer to tailoring interventions that are not just safe and effective but also optimized for each individual’s specific needs, preventing unintended consequences.
The Road Ahead: Research and Future Perspectives
The intricate dance between zinc and its myriad interactors is a field of ongoing discovery. Future research will undoubtedly shed more light on:
- Nutrigenomics and Pharmacogenomics: How individual genetic variations influence zinc metabolism, absorption, and susceptibility to drug-induced depletion. This could lead to personalized risk assessments.
- Advanced Diagnostic Tools: Development of more accurate and accessible biomarkers for assessing functional zinc status, moving beyond reliance on plasma levels.
- Drug Design: Pharmaceutical companies increasingly consider potential drug-nutrient interactions during drug development, aiming to design molecules with fewer such unintended consequences.
- Enhanced Clinical Guidelines: Integrating comprehensive guidelines for screening, monitoring, and managing drug-nutrient interactions into standard clinical practice.
- Patient Education Tools: Developing intuitive and accessible resources that empower patients to understand potential interactions and advocate for their health.
Conclusion: The Unseen Tapestry
Mrs. Eleanor Vance, under the watchful eye of Dr. Thorne and Dr. Sharma, slowly began to regain her vitality. Her fatigue lessened, her infections became less frequent, and a faint appreciation for the subtle flavors of her food returned. It wasn’t a single magic bullet, but a meticulous unraveling of the hidden threads that had silently, relentlessly, been pulling at her zinc status.
Her story is a microcosm of a larger truth: that our biological systems are an unseen tapestry, woven with countless threads of nutrients, enzymes, hormones, and external influences. What appears on the label – be it a food ingredient list or a drug prescription – is merely a small part of the story. The true narrative unfolds in the complex, dynamic interactions occurring beneath the surface.
To truly care for health, we must cultivate a mindset of vigilance, curiosity, and a willingness to look "beyond the label." We must embrace the complexity, understanding that even the most essential elements, like zinc, can be compromised by seemingly innocuous choices. In this interconnected world, knowledge of these hidden ingredients and drug classes is not merely academic; it is a vital tool in the pursuit of genuine well-being, a continuous journey of discovery where every thread, no matter how small, holds profound significance. The story of zinc reminds us that in the grand orchestra of the human body, every player, and every interaction, matters.