Stop a Migraine Before It Starts: Your Emergency Action Plan – A Story of Reclamation
The first tendril of shadow stretched across Elara’s vision, a shimmering, almost imperceptible distortion at the periphery. For years, this was the harbinger of doom, the silent, terrifying overture to hours, sometimes days, of excruciating pain, blinding light sensitivity, and nausea that threatened to empty her very soul. It was a life lived in fear, a constant dance on the edge of a precipice, where every social engagement, every work deadline, every moment of joy was overshadowed by the question: When will the next one strike?
Elara remembered a time before the migraines consumed her. A vibrant architect, she thrived on late nights at the drawing board, the hum of collaboration, the sharp scent of ink and ambition. Then, at 28, the first true migraine hit, a seismic event that shattered her perception of wellness. It wasn’t just a headache; it was a total system shutdown. Her brain felt like a raw nerve, her eyes rebelled against the faintest glimmer, and the world spun in a sickening vortex. The attacks became more frequent, more aggressive, stealing days, weeks, even months from her life. She’d tried everything: over-the-counter pain relievers that laughed in the face of her agony, dietary changes that stripped all joy from eating, acupuncture that offered fleeting peace, even experimental therapies that left her feeling more like a lab rat than a human being. Each failed attempt chipped away at her hope, leaving her stranded in a cycle of pain, recovery, and dread.
Her life shrank. She turned down promotions that required travel, cancelled plans with friends at the last minute, and her once-sparkling apartment became a darkened sanctuary against the encroaching light. The shame, the guilt, the feeling of being a burden – these were almost as debilitating as the physical pain itself. Her family tried to understand, her partner, Mark, was endlessly patient, but how could anyone truly grasp the terror of a brain turning against itself?
Then came the day of the gallery opening. A culmination of months of work, a critical project for her firm, and Elara felt the familiar prickle behind her left eye, the subtle shift in her perception of sound, the sudden, inexplicable exhaustion that felt heavier than any physical exertion. She was surrounded by colleagues, clients, the bright lights of the exhibit hall, the cacophony of excited chatter. Panic seized her. She knew, with a chilling certainty, that she was moments away from being completely incapacitated. The thought of collapsing there, of letting down her team, of once again becoming the "sick one," was unbearable. She fled, stumbling into a cab, the world outside already beginning its malicious assault on her senses. She spent the next two days in a silent, dark room, the migraine raging, leaving her utterly depleted and utterly defeated.
It was in the aftermath of that attack, curled in a ball on her sofa, the phantom throbbing still a cruel reminder, that something shifted within her. This couldn’t be her life. This wouldn’t be her life. She was tired of being a victim. She was tired of the fear. She was tired of the helplessness. She needed a new strategy, not just for managing the attacks, but for stopping them dead in their tracks. She needed an Emergency Action Plan.
Chapter 1: The Genesis of Despair (and the Seeds of Hope)
Elara’s journey had been long and winding, marked by frustrating misdiagnoses and well-meaning but ultimately ineffective advice. General practitioners often dismissed her symptoms as "just headaches," prescribing basic pain relievers that were like bringing a squirt gun to a forest fire. She’d been told it was stress, poor diet, even "all in her head." Each dismissal fueled her isolation.
"It’s like my brain has declared war on the rest of me," she’d confided in Mark once, tears streaming down her face. "And I’m caught in the crossfire."
The turning point came not from a single revelation, but from a cumulative exhaustion with her suffering. After the gallery incident, Mark, seeing the profound despair in her eyes, took the initiative. He researched specialists, not just neurologists, but headache and migraine experts, those who understood the nuanced complexity of the condition. He found Dr. Aris Thorne, renowned for his holistic yet evidence-based approach to migraine management, a physician who treated the person, not just the symptom.
Elara’s first appointment with Dr. Thorne was different. He didn’t rush. He listened intently, letting her pour out years of frustration, fear, and pain. He asked detailed questions about her history, her triggers, her lifestyle. He validated her experience, something few doctors had truly done before.
"Elara," Dr. Thorne said, his voice calm and reassuring, "what you’re experiencing is a complex neurological disorder, not ‘just a headache.’ And while there’s no magic cure, there are incredibly effective strategies to manage and, crucially, to abort attacks before they take hold. We’re going to build you an Emergency Action Plan, a personalized defense system that will empower you to fight back."
The words "fight back" resonated deep within Elara. It wasn’t about enduring anymore; it was about confronting. It was about agency.
Chapter 2: Understanding the Enemy – Prodrome and Aura
Dr. Thorne began by explaining the four phases of a migraine attack: Prodrome, Aura, Attack, and Postdrome. He emphasized that the key to stopping a migraine before it starts lay squarely in understanding and acting during the prodrome and aura phases.
"Think of these as your early warning signs," he explained, gesturing with a pen. "The prodrome can occur hours or even days before the pain begins. It’s your body’s subtle way of telling you a storm is brewing. The aura, if you experience it, is a more distinct neurological event, often visual, that usually precedes the headache phase by minutes to an hour."
Elara had always perceived these early symptoms as mere annoyances, precursors to the inevitable. She’d never considered them windows of opportunity.
"For you, Elara," Dr. Thorne continued, "the first step is meticulous self-observation. We need to identify your specific prodromal symptoms. These vary greatly from person to person."
He handed her a detailed migraine journal. "I want you to track everything. Not just when the migraine hits, but everything leading up to it. Did you feel unusually tired? Irritable? Crave certain foods? Experience neck stiffness? Notice increased sensitivity to light or sound? Even subtle changes in mood or difficulty concentrating."
Elara, initially skeptical, embraced the task with a newfound determination. She began logging every flicker, every nuance. Over weeks, patterns emerged. Her prodrome wasn’t always the same, but common threads appeared:
- Profound fatigue: A sudden, crushing exhaustion that sleep couldn’t alleviate.
- Frequent yawning: Often accompanied by the fatigue, seemingly out of nowhere.
- Mood changes: Irritability, anxiety, or even a strange, almost euphoric feeling.
- Neck stiffness: A tightening sensation, often at the base of her skull.
- Food cravings: Salty snacks, chocolate, things she didn’t usually crave.
- Increased sensitivity: Slight discomfort from bright lights (photophobia) or normal sounds (phonophobia).
- Cognitive fog: Difficulty concentrating, finding words, feeling "out of it."
Then there was the aura. For Elara, it was primarily visual – the shimmering zigzag lines, like heat rising off asphalt, that would expand across her vision, sometimes obscuring her sight partially. She learned to distinguish this distinct neurological event from the more generalized prodromal symptoms. The aura, Dr. Thorne explained, was a clear signal: action is required, now.
"The sooner you intervene," he stressed, "the more effective your treatment will be. Waiting until the pain is established is like trying to put out a house fire after it’s engulfed the entire structure. We want to catch it when it’s just a spark."
This was revolutionary thinking for Elara. She had always waited, hoping it would pass, or worse, steeling herself for the inevitable onslaught. The journal became her trusted ally, a mirror reflecting the intricate dance of her body’s signals. She was learning the enemy’s language.
Chapter 3: Assembling the Arsenal – The EAP Components
With a clear understanding of her warning signs, the next step was to build her personalized arsenal. Dr. Thorne outlined the pillars of an effective Emergency Action Plan.
Pillar 1: Abortive Medications (The Heavy Artillery)
"These are your primary weapons against an impending attack," Dr. Thorne explained. "Their goal is to stop the migraine cascade in its tracks, not just to mask the pain."
-
Triptans: "For many, triptans are the gold standard for acute migraine treatment," he said. "They work by constricting blood vessels in the brain and blocking pain pathways. There are several types – oral tablets, nasal sprays, even injectables. We’ll find the one that works best and fastest for you." He prescribed Elara a fast-acting oral triptan, advising her to take it at the very first sign of prodrome or aura, not to wait for the headache to fully develop. He also explained the potential side effects, like chest tightness or tingling, which were usually mild and temporary. "Don’t be afraid of them," he reassured. "We’ll monitor closely."
-
CGRP Receptor Antagonists (Gepants): "These are a newer class of abortive medications," he continued, "and they work differently than triptans, by blocking the CGRP peptide, which plays a crucial role in migraine pain transmission. They can be very effective, especially for those who don’t respond to triptans or have cardiovascular concerns." He gave Elara a prescription for a gepant as a potential alternative or rescue medication if the triptan wasn’t fully effective.
-
Over-the-Counter Options (NSAIDs & Combination Analgesics): "For very mild attacks, or as a bridge while waiting for a triptan to kick in, simple NSAIDs like ibuprofen or naproxen can be helpful," Dr. Thorne advised. "Some people also find combination analgesics containing acetaminophen, aspirin, and caffeine effective, but be cautious with caffeine intake to avoid medication overuse headache." Elara knew from bitter experience that these were often insufficient for her severe attacks, but she understood their place in the broader strategy.
-
Anti-Nausea Medications (Antiemetics): "Nausea and vomiting are common and debilitating migraine symptoms," he noted. "Having an antiemetic on hand, like ondansetron or metoclopramide, can be crucial, especially if your migraines often involve severe GI upset. Taking it alongside your abortive medication can improve absorption and comfort."
Pillar 2: Non-Pharmacological Interventions (The Supportive Troops)
"Medication is powerful, but it’s not the only tool," Dr. Thorne emphasized. "These supportive measures can significantly enhance the effectiveness of your abortive medications and provide comfort."
- Rest in a Dark, Quiet Room: "This is paramount. As soon as you feel the prodrome, seek refuge. Minimize sensory input. Lie down in a cool, dark, silent space."
- Cold/Heat Packs: "Many find relief from a cold pack on the forehead or neck, which can constrict blood vessels and numb pain. Others prefer heat for neck stiffness. Experiment to see what works for you."
- Hydration & Electrolytes: "Dehydration can worsen a migraine. Keep water or an electrolyte drink readily available."
- Strategic Caffeine: "While too much caffeine can be a trigger or lead to rebound headaches, a small amount at the very beginning of a prodrome can sometimes help, especially if you regularly consume caffeine. But this is a delicate balance."
- Mindfulness & Relaxation Techniques: "Deep breathing, guided meditation, or progressive muscle relaxation can help calm your nervous system, reduce stress, and potentially lessen the severity of the attack. Even just five minutes can make a difference."
- Acupressure/Massage: "Gentle pressure on specific points, or a light massage of the temples and neck, can offer some relief for muscle tension and pain."
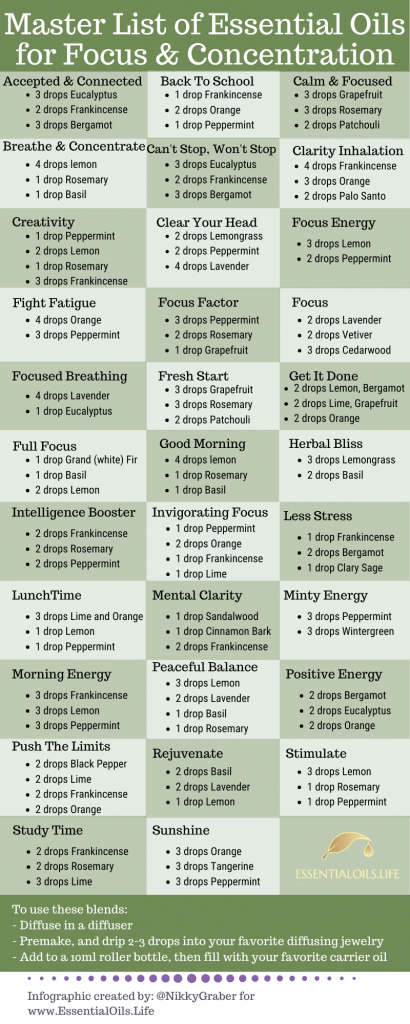
- Essential Oils: "Some people find certain essential oils, like peppermint (diluted and applied to temples) or lavender (diffused or inhaled), to be soothing and helpful for mild symptoms, but use with caution and test for sensitivity."
Pillar 3: Lifestyle & Preventative Measures (The Long-Term Strategy)
While the EAP focused on acute intervention, Dr. Thorne stressed that it existed within a larger framework of migraine management.
- Consistent Sleep Schedule: "Irregular sleep is a major trigger. Aim for 7-9 hours of consistent sleep, even on weekends."
- Regular Meals & Hydration: "Skipping meals or dehydration can drop blood sugar and trigger attacks."
- Stress Management: "Stress doesn’t cause migraines, but it’s a huge trigger. Incorporate stress-reducing activities like yoga, meditation, or hobbies."
- Regular Exercise: "Moderate, consistent exercise can reduce migraine frequency and severity, but avoid overexertion, especially if you’re prone to exercise-induced migraines."
- Trigger Identification & Avoidance: "Continue with your migraine journal. Identifying and minimizing exposure to personal triggers (foods, smells, weather changes, hormonal fluctuations) is crucial."
- Preventative Medications: "For those with frequent or severe migraines, daily preventative medications (like beta-blockers, certain antidepressants, anti-seizure medications, or the newer CGRP monoclonal antibodies) can significantly reduce the number and intensity of attacks. We’ll consider these if your EAP alone isn’t enough to reclaim your quality of life."
Elara felt a surge of hope she hadn’t experienced in years. This wasn’t just a list of drugs; it was a comprehensive, multi-faceted strategy. She had an understanding of the enemy, and now, she had a detailed battle plan.
Chapter 4: The First Test – A Real-Life Scenario
The true test of the EAP came two weeks later. Elara was deep in a complex design review, the air thick with the murmur of voices and the hum of projectors. Suddenly, a familiar wave of exhaustion washed over her, heavier than usual. She yawned, involuntarily, a deep, sighing yawn that felt profoundly unsatisfying. Then, the subtle stiffness at the base of her neck. Her internal alarm bells began to clang. Prodrome.
Her immediate instinct, honed by years of suffering, was to ignore it, to push through, to hope it would pass. But Dr. Thorne’s words echoed in her mind: "Don’t wait. Treat early. Don’t let the migraine take hold."
She excused herself from the meeting, her heart pounding. Her colleagues, used to her occasional abrupt departures, barely noticed. Elara walked briskly to her office, her emergency kit already prepared and waiting in her desk drawer: a foil-wrapped triptan, an anti-nausea pill, a small bottle of water, and an eye mask.
She took a deep breath, fighting the urge to rationalize, to minimize. Is it really starting? Maybe it’s just stress. But the journal, the patterns she’d observed, screamed otherwise. This was it.
With a resolve she hadn’t known she possessed, she swallowed the triptan and the anti-nausea medication with a gulp of water. She then made a conscious decision: she wouldn’t just medicate; she would activate the full EAP.
She sent a quick email to her team, vaguely citing "not feeling well" and promising to catch up later. She then dimmed the lights in her office, pulled down the blinds, and put on her eye mask. She leaned back in her chair, pressing a cool gel pack to her forehead. She closed her eyes and focused on her breath, slowly inhaling to a count of four, holding for seven, and exhaling for eight, just as Dr. Thorne had taught her. She felt the tension in her shoulders, her jaw, and consciously relaxed each muscle.
Minutes stretched into what felt like an eternity. The initial symptoms were still there, a low thrum of discomfort. The shimmer in her peripheral vision began to appear, a faint, ghostly outline. Aura. But this time, it felt different. Less terrifying, more manageable. She was already ahead of it.
Then, gradually, subtly, a shift occurred. The throbbing that usually escalated to a crescendo of agony simply… didn’t. The nausea, which typically became a churning tempest, remained a distant whisper. The shimmering lines in her vision faded, receding like a tide. The profound exhaustion began to lift, replaced by a gentle weariness, not the debilitating kind.
An hour later, Elara carefully removed her eye mask. The world wasn’t a hostile glare. The sounds of the office, once an unbearable din, were now just background noise. The pain, usually a searing inferno, was a faint, almost forgettable ache, easily dismissed.
She wasn’t 100%. She felt a lingering fatigue, a sense of having narrowly averted something catastrophic. But she hadn’t collapsed. She hadn’t spent two days in bed. She hadn’t lost her work. She had stopped it.
A wave of profound relief washed over her, followed by an exhilarating sense of empowerment. She had fought back, and she had won, or at least, secured a decisive victory. This wasn’t just a blunted attack; it was a reclaiming of her life, a defiant stand against the tyranny of migraine.
Chapter 5: Refinement and Resilience – Adapting the Plan
The first successful intervention was a revelation, but Elara quickly learned that the EAP wasn’t a magic bullet that worked identically every time. Migraines, like chameleons, could adapt and present in different forms.
A few weeks later, she experienced another prodrome, but this time, the triptan seemed less effective. The pain started to build, albeit slowly, and the nausea lingered stubbornly. Instead of despair, Elara felt a different emotion: curiosity. She consulted her journal, noting the specific symptoms and the partial success of her initial plan.
At her next follow-up, she discussed this with Dr. Thorne. "It wasn’t a complete failure," she explained, "but it wasn’t a total win either. The pain was maybe a 5 out of 10, instead of a 9, but it was still there."
Dr. Thorne nodded. "Excellent observation, Elara. This is precisely why the EAP is a living document. Not all attacks are the same, and your body’s response can vary. We have options. Perhaps a different triptan, one with a slightly different pharmacokinetic profile, might work better for you. Or we can consider using the gepant as a first-line abortive in certain scenarios, especially if you have lingering nausea. We could also add a second dose of your antiemetic."
They adjusted her plan. She now carried two different types of abortive medications, a triptan and a gepant, giving her flexibility. She also learned to distinguish between different "flavors" of prodrome. Sometimes, the neck stiffness was more pronounced; other times, the cognitive fog was dominant. She started to associate these nuances with the likely severity of the impending attack, allowing her to tailor her initial response.
The psychological shift was perhaps the most profound change. The constant fear began to recede. She still experienced prodromal symptoms, but they no longer triggered the same debilitating panic. Instead, they were signals, prompts for action. She was no longer waiting for the storm; she was actively preparing for it, sometimes even diverting it entirely.
She found herself saying "yes" to life again. A weekend trip with Mark, a challenging new project at work, an evening out with friends. She knew the risk was still there, but she also knew she had a powerful tool in her pocket, a shield against the worst of it. The EAP wasn’t a cure, but it was a bridge back to normalcy, a way to reclaim the vibrant, ambitious woman she used to be. She learned to be compassionate with herself, understanding that even with the best plan, some migraines would break through. On those days, she allowed herself to rest, to recover, without the crushing weight of guilt. She had fought her best fight, and that was enough.
Conclusion: A Story of Reclamation
Elara, now 35, still lives with migraine. It is a part of her, a neurological predisposition that will likely always be there. But it no longer defines her. The dark cloud that once hung perpetually over her life has dissipated, replaced by the clear skies of proactive management. Her Emergency Action Plan isn’t just a list of medications and techniques; it’s a testament to her resilience, her dedication, and the power of informed self-advocacy.
She understands now that stopping a migraine before it starts isn’t about eradicating the potential for an attack, but about interrupting its devastating trajectory. It’s about recognizing the earliest whispers of discomfort and acting decisively, armed with knowledge and the right tools. It’s about transforming fear into preparedness, helplessness into empowerment.
Her story is a beacon of hope for countless others who suffer in silence. It’s a powerful reminder that while migraines can be debilitating, they don’t have to dictate the terms of your existence. By understanding your unique triggers and prodromal signs, by partnering with knowledgeable healthcare providers, and by meticulously crafting and diligently executing your own personalized Emergency Action Plan, you too can reclaim your life from the shadow of migraine. Don’t wait. Don’t suffer. Seek help, learn your body’s signals, and build your arsenal. The power to stop a migraine before it starts is not a fantasy; it is a tangible reality, waiting for you to seize it.