The Unseen Tapestry: Weaving Your Headache Triggers
The sudden, unwelcome throb. The dull, persistent ache that settles behind your eyes like an uninvited guest. The searing, incapacitating pain that steals your day, your focus, your very peace. Headaches, in their myriad forms, are a ubiquitous human experience, yet their genesis often remains shrouded in a frustrating veil of mystery. For many, a headache isn’t just a fleeting discomfort; it’s a recurring torment, a perplexing puzzle whose pieces seem scattered across the landscape of daily life.
"Is it my neck, my diet, or my stress?" This tripartite question echoes in the minds of countless sufferers, a desperate attempt to pinpoint the elusive culprit. But what if the answer isn’t a singular, isolated factor, but rather a complex, interwoven tapestry of influences, each thread contributing to the final, painful pattern? To truly understand and manage our headaches, we must become meticulous cartographers of our own physiology, tracing the intricate pathways of cause and effect, recognizing that the journey to relief often begins with a journey of self-discovery.
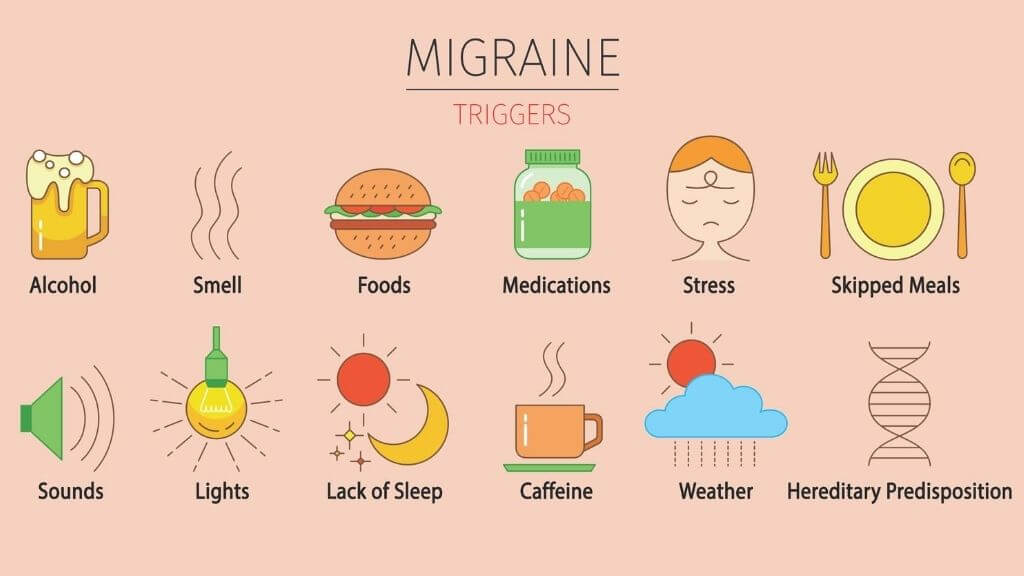
This exploration delves deep into the three most commonly suspected instigators – our posture and musculoskeletal health, the fuel we provide our bodies, and the relentless pressures of modern living. More importantly, it seeks to illuminate the profound synergy between them, revealing how these seemingly disparate elements often conspire to lower our individual pain thresholds, transforming minor irritations into full-blown neurological events.
The Cervical Labyrinth: When Your Neck Calls the Shots
Imagine your head, a weighty orb housing your most vital organ, delicately balanced atop the slender, intricate structure of your cervical spine. This column of seven vertebrae, interspersed with shock-absorbing discs and crisscrossed by a network of muscles, ligaments, and nerves, is a marvel of engineering. Yet, in our increasingly sedentary, tech-driven world, it’s also a common battlefield where the first skirmishes of a headache often begin.
The Anatomy of Strain:
The cervical spine is designed for mobility and support. However, prolonged or repetitive strain can compromise its delicate balance. Consider the suboccipital muscles, a group of four small muscles located at the base of your skull. These tiny powerhouses are responsible for fine movements of the head and are densely packed with proprioceptors, nerve endings that tell your brain where your head is in space. When these muscles become tight, fatigued, or go into spasm due to poor posture, they can refer pain directly into the skull, often felt as a band-like pressure or a throbbing at the back of the head, radiating towards the temples or eyes.
Beyond the suboccipitals, the larger muscles of the neck and shoulders – the trapezius, sternocleidomastoid (SCM), and levator scapulae – also play a critical role. Chronic tension in these muscles can create trigger points, hyperirritable spots that, when pressed, elicit pain not only locally but also in distant areas. A trigger point in the upper trapezius, for instance, can refer pain up the side of the head, mimicking a tension headache. Similarly, tightness in the SCM, running from behind the ear down to the collarbone, can refer pain to the forehead, around the eye, and even to the jaw.
The Modern Postural Predicament:
Our digital age has ushered in an epidemic of "tech neck" or "text neck." The average adult head weighs between 10-12 pounds. Tilting your head forward just 15 degrees can increase the effective weight on your neck to 27 pounds. At 60 degrees, it’s a staggering 60 pounds – the equivalent of carrying an 8-year-old child on your neck for hours on end. This sustained forward head posture flattens the natural cervical curve, overstretches posterior neck muscles, and compresses anterior structures. The result is chronic strain, muscle imbalances, and potentially, nerve impingement.
The greater occipital nerve, emerging from the second and third cervical vertebrae, is particularly vulnerable. It travels up the back of the head, supplying sensation to the scalp. When compressed or irritated by tight muscles or misaligned vertebrae, it can cause occipital neuralgia – a sharp, shooting, or burning pain that starts at the base of the skull and radiates over the scalp, often unilateral.
Beyond the Screen:
It’s not just screens that are to blame. Poor ergonomics at work (an ill-adjusted chair, a monitor too high or low), inadequate pillow support during sleep, carrying heavy bags on one shoulder, clenching your jaw (bruxism), or even the lingering effects of an old whiplash injury can all contribute to cervical strain and subsequent headaches. Stress, as we’ll explore, also manifests physically as muscle tension, creating a vicious cycle where a tight neck exacerbates stress, and stress, in turn, tightens the neck further.
Solutions for the Cervical Culprit:
Addressing neck-related headaches requires a multi-pronged approach:
- Ergonomic Assessment: Optimize your workstation. Monitor at eye level, keyboard and mouse within easy reach, feet flat on the floor.
- Posture Awareness: Regular checks throughout the day. Imagine a string pulling the crown of your head upwards.
- Movement Breaks: Stand, stretch, gently mobilize your neck and shoulders every 30-60 minutes.
- Targeted Exercises: Strengthening exercises for deep neck flexors and upper back muscles, stretching for tight neck and chest muscles.
- Manual Therapies: Physical therapy, chiropractic adjustments, massage therapy can help restore mobility, release muscle tension, and alleviate nerve compression.
- Sleep Hygiene: Invest in a supportive pillow that maintains neutral spine alignment.
The Culinary Conundrum: When Food Becomes Foe
The adage "you are what you eat" takes on a particularly poignant meaning when confronting headache triggers. For a significant subset of individuals, certain foods and beverages, or even the lack thereof, can act as potent provocateurs, stirring up a biochemical tempest that culminates in head pain. This isn’t about food allergies in the traditional sense, but rather sensitivities, where specific compounds or the metabolic response they elicit can trigger a cascade of events leading to a headache.
The Usual Suspects and Their Mechanisms:
- Tyramine: Found in aged cheeses, cured meats, fermented foods (sauerkraut, soy sauce), red wine, and some nuts. Tyramine is a naturally occurring amino acid that can affect blood pressure and neurotransmitter levels. In sensitive individuals, particularly those on MAO inhibitor medications or those with a deficiency in the enzyme that breaks down tyramine, it can trigger vasoconstriction followed by vasodilation, a common mechanism in migraine.
- Nitrates/Nitrites: Preservatives commonly found in processed meats like hot dogs, bacon, and deli meats. They cause blood vessels to dilate, which can lead to a "hot dog headache" or aggravate migraines.
- Sulfites: Used as preservatives in dried fruits, wine, and some processed foods. While more commonly associated with asthma symptoms, they can trigger headaches in sensitive individuals.
- Histamine: Found in fermented foods, aged cheeses, wine, beer, and some fish. Individuals with histamine intolerance lack sufficient diamine oxidase (DAO), the enzyme responsible for breaking down histamine in the gut. High histamine levels can cause vasodilation and trigger headache symptoms.
- Caffeine: A double-edged sword. While caffeine can acutely relieve some headaches by constricting blood vessels, withdrawal from regular caffeine consumption is a notorious headache trigger. Even a slight delay in your morning coffee can precipitate a throbbing headache as blood vessels rebound and dilate excessively.
- Artificial Sweeteners (Aspartame, Sucralose): Though research is mixed and individual responses vary, some people report headaches after consuming products containing artificial sweeteners. The proposed mechanisms include effects on neurotransmitters or a general inflammatory response.
- Monosodium Glutamate (MSG): A flavor enhancer found in many processed foods, Chinese cuisine, and some snacks. While the existence of "MSG symptom complex" is debated, a subset of individuals consistently reports headaches, facial flushing, and other symptoms after consuming MSG.
- Alcohol: Especially red wine, due to its combination of histamines, sulfites, and tyramine. The dehydrating effect of alcohol also plays a significant role.
- Chocolate: A common anecdotal trigger, though its role is complex. It contains phenylethylamine, which can affect blood vessel tone, and caffeine. However, cravings for chocolate often precede a migraine attack, suggesting it might be a symptom rather than a cause.
Beyond Specific Foods: The Broader Nutritional Landscape:
- Dehydration: Perhaps the simplest and most overlooked dietary trigger. Even mild dehydration can decrease blood volume, affecting blood flow to the brain and leading to a dull, persistent headache.
- Blood Sugar Fluctuations: Skipping meals, consuming high-sugar foods that lead to a rapid spike and crash in blood glucose, or poorly managed diabetes can all trigger headaches. Hypoglycemia (low blood sugar) deprives the brain of its primary fuel, glucose, leading to irritation and pain.
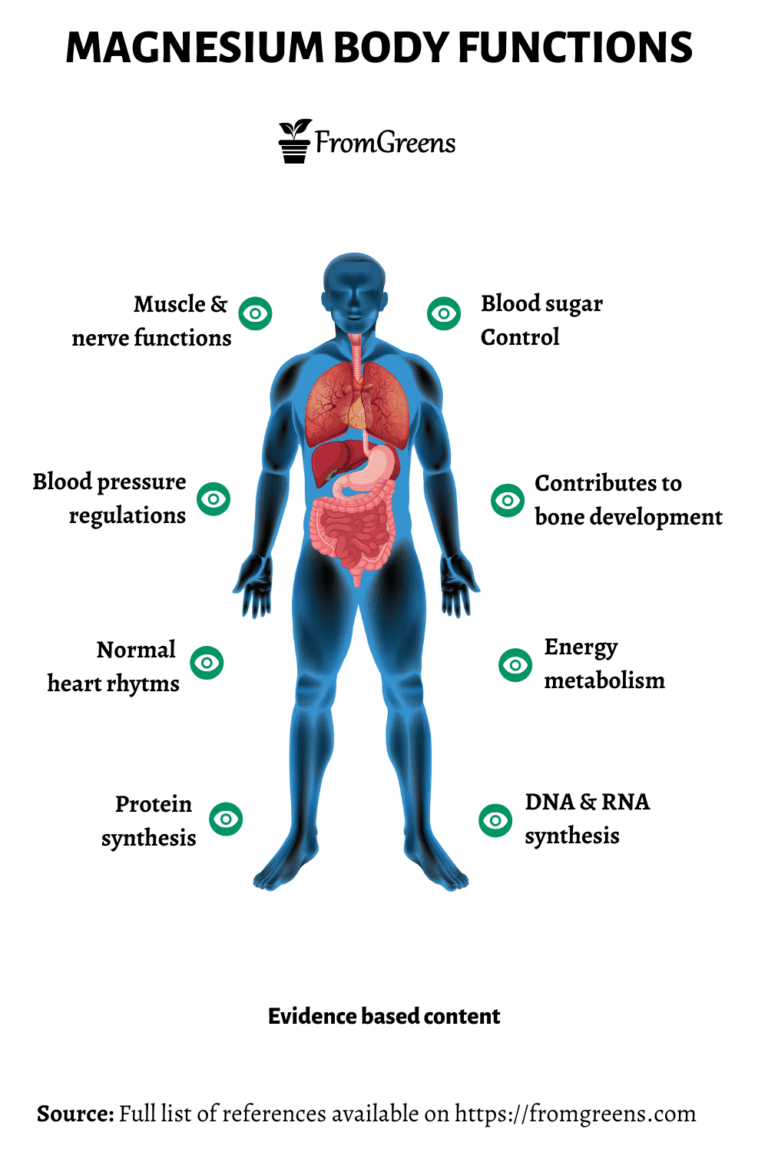
- Micronutrient Deficiencies: While less direct, chronic deficiencies in magnesium, riboflavin (Vitamin B2), CoQ10, and certain B vitamins have been linked to an increased susceptibility to migraines and headaches. These nutrients play roles in energy metabolism and neurological function.
The Dietary Detective: Tracking and Elimination:
Identifying dietary triggers is a meticulous process that requires patience. A detailed headache diary (more on this later) is crucial, documenting not just headache onset and severity but also all food and drink consumed in the 24-48 hours prior. Once potential culprits are identified, an elimination diet can be undertaken under professional guidance. This involves strictly removing the suspected food(s) for a period (e.g., 2-4 weeks), followed by systematic reintroduction to observe if symptoms return. This process demands discipline and careful monitoring to accurately pinpoint triggers.
The Stress Symphony: The Mind-Body Overture of Pain
Of all the potential headache triggers, stress is arguably the most pervasive and insidious. It doesn’t just "cause" headaches; it acts as a powerful amplifier, a conductor of a painful symphony that leverages our physiological responses to life’s demands. In our always-on, hyper-connected world, chronic stress has become a default state for many, and our bodies, designed for acute fight-or-flight responses, are struggling to cope with this relentless pressure.
The Physiological Cascade of Stress:
When we perceive a threat – be it a looming deadline, a difficult conversation, or a traffic jam – our sympathetic nervous system springs into action. This "fight-or-flight" response involves:
- Hormone Release: The hypothalamus-pituitary-adrenal (HPA) axis activates, flooding the body with stress hormones like cortisol and adrenaline.
- Increased Muscle Tension: Muscles throughout the body, particularly in the neck, shoulders, and jaw, involuntarily tense up in preparation for action. This directly feeds into the cervical labyrinth discussed earlier.
- Altered Blood Flow: Blood is shunted away from non-essential functions (like digestion) towards large muscle groups. This can affect cerebral blood flow.
- Neurotransmitter Imbalance: Chronic stress can deplete neurotransmitters like serotonin, which plays a critical role in mood, sleep, and pain regulation. Low serotonin levels are strongly implicated in migraine pathogenesis.
The Many Faces of Stress-Induced Headaches:
- Tension Headaches: The most common form of headache, often directly linked to stress. They are characterized by a dull, aching pain, a feeling of tightness or pressure around the forehead, temples, or back of the head, often described as a "vice-like" sensation. Muscle tension in the neck and shoulders is a hallmark.
- Migraines: While not solely caused by stress, stress is a significant trigger for migraine attacks in many sufferers. The fluctuations in stress levels – particularly the "let-down" headache that occurs when a period of intense stress abruptly ends – can be particularly potent. This rebound effect is thought to be due to rapid changes in neurochemical levels.
- Cluster Headaches: Though less common, stress can exacerbate or trigger cluster headache cycles in susceptible individuals.
The Interplay with Sleep and Lifestyle:
Stress profoundly disrupts sleep patterns. Insomnia, restless sleep, or oversleeping (especially on weekends, a form of stress "let-down") can all trigger headaches. Lack of quality sleep impairs the body’s ability to repair and restore itself, leading to increased inflammation and a lower pain threshold.
Moreover, stress often leads to maladaptive coping mechanisms that, in themselves, become headache triggers. Stress eating (often leading to consumption of high-sugar, processed foods), increased alcohol intake, or neglecting regular meals (leading to blood sugar fluctuations) create a dangerous synergy with dietary triggers. Skipping exercise due to feeling overwhelmed or adopting poor posture while hunched over tasks for long hours further compounds the problem.
Strategies for Stress Management:
Mitigating stress-related headaches requires a holistic approach to managing the demands of life:
- Mindfulness and Meditation: Regular practice can alter brain pathways, reducing the physiological stress response.
- Regular Exercise: A powerful stress reliever, exercise releases endorphins, improves circulation, and helps dissipate muscle tension.
- Cognitive Behavioral Therapy (CBT): Can help individuals identify and reframe negative thought patterns and develop healthier coping strategies.
- Boundary Setting: Learning to say no, delegating tasks, and creating clear divisions between work and personal life are crucial.
- Time Management: Prioritizing tasks and avoiding procrastination can reduce feelings of overwhelm.
- Hobbies and Relaxation Techniques: Engaging in enjoyable activities, deep breathing exercises, progressive muscle relaxation, and spending time in nature can all help regulate the nervous system.
- Sleep Hygiene: Establishing a consistent sleep schedule, creating a conducive sleep environment, and avoiding screens before bed.
The Interwoven Threads: The Symphony of Synergy
The truly illuminating insight in tracing headache triggers lies not in isolating neck, diet, or stress, but in recognizing their profound interconnectedness. Seldom does a headache arise from a single, pristine cause. More often, it is the cumulative effect, the subtle interplay of several factors, that pushes an individual past their unique "trigger threshold" and into the realm of pain. This is where the metaphor of the unseen tapestry truly comes alive.
Imagine Sarah, a diligent professional. She’s been under immense pressure at work (stress), leading to prolonged hours hunched over her laptop with poor posture (neck strain). In her haste, she often skips lunch or grabs a quick, sugary snack (dietary imbalance, blood sugar crash). The combination of chronic muscle tension in her neck and shoulders, coupled with the neurochemical effects of stress and the metabolic disruption from her diet, lowers her overall pain threshold. A minor trigger that she might normally shrug off – a slight change in barometric pressure, a whiff of strong perfume – now becomes the final thread that pulls the tapestry taut, resulting in a debilitating migraine.
Or consider Mark, a devoted father. He’s trying a new, restrictive diet (dietary change) that has him feeling slightly dehydrated and irritable. He’s also sleeping poorly due to anxiety about his child’s upcoming exams (stress). One evening, he settles down to watch a movie, adopting a slouched position on the couch (neck strain). The confluence of these factors – the physiological strain from dehydration and stress-induced sleep deprivation, combined with the muscle tension from poor posture – creates a perfect storm. What might have been a mild, fleeting tension in his head now escalates into a full-blown, throbbing headache that lasts for hours.
The Trigger Threshold Concept:
Each individual possesses a unique physiological pain threshold. This threshold isn’t static; it fluctuates based on internal and external factors. When we are well-rested, hydrated, nutritionally balanced, and relatively stress-free, our threshold is high. We can encounter minor irritants without developing a headache. However, when we are sleep-deprived, stressed, consuming trigger foods, and holding tension in our neck, our threshold drops significantly. It takes far less to push us over the edge into pain.
This cumulative effect explains why some headaches seem to appear "out of nowhere." It wasn’t a single, dramatic event, but rather a slow accumulation of smaller stressors, dietary indiscretions, and postural habits that gradually eroded the body’s resilience. The final "trigger" might be something seemingly innocuous, but it was merely the last straw on a camel already burdened.
Inflammation: The Unifying Theme:
Chronic stress, poor dietary choices (especially inflammatory foods like processed sugars, unhealthy fats), and even chronic muscle tension can all contribute to systemic inflammation. While inflammation is a vital immune response, chronic low-grade inflammation can sensitize pain pathways, making the body more susceptible to headache pain. Stress hormones, dietary components, and even mechanical stress on tissues can modulate inflammatory markers, creating a feedback loop that sustains or exacerbates headache frequency and intensity.
Becoming the Cartographer: Charting Your Pain Landscape
The path to understanding your headaches is an active, investigative one. You must become a detective, meticulously gathering clues, identifying patterns, and testing hypotheses. This journey demands patience, self-awareness, and often, professional guidance.
The Indispensable Headache Diary:
This is your primary tool. For at least 4-8 weeks, diligently record:
- Date and Time of Headache Onset: When did it start?
- Severity: On a scale of 1-10.
- Location and Type of Pain: Frontal, temporal, occipital, pulsating, dull, sharp, band-like.
- Associated Symptoms: Nausea, light sensitivity (photophobia), sound sensitivity (phonophobia), aura, numbness, visual disturbances, neck stiffness.
- Potential Triggers (in the 24-48 hours prior):
- Diet: Every food and drink consumed, noting any unusual items.
- Sleep: Hours slept, quality of sleep.
- Stress Levels: Rate daily stress (1-10), note specific stressors.
- Physical Activity: Type, intensity.
- Posture: Prolonged screen time, specific activities.
- Environmental Factors: Weather changes, strong smells, bright lights.
- Hormonal Factors: For women, menstrual cycle phase.
- Medications/Remedies Used: What worked, what didn’t?
- Relief Measures: What helped alleviate the pain?
Over time, this diary will reveal invaluable patterns. You might notice that headaches consistently follow a night of poor sleep and a morning coffee on an empty stomach. Or that they frequently appear after a particularly stressful meeting and prolonged computer work. The diary doesn’t just identify triggers; it also highlights effective coping strategies.
When to Seek Professional Guidance:
While self-monitoring is powerful, it’s crucial to know when to involve healthcare professionals:
- Sudden, Severe Headache: The "worst headache of your life," especially if accompanied by neurological symptoms like weakness, numbness, vision changes, or confusion.
- Headaches with Fever, Stiff Neck, Rash: Could indicate meningitis or other serious conditions.
- Headaches After Head Injury: Even a mild one.
- New Headache Pattern After Age 50: Any new or significantly different headache presentation.
- Increasing Frequency or Severity: Headaches becoming more frequent, longer-lasting, or more painful.
- Headaches Affecting Daily Life: If they significantly impact work, relationships, or quality of life.
A primary care physician is often the first point of contact, who can rule out serious underlying conditions. Referral to a neurologist specializing in headache disorders is common for chronic or severe cases. A physical therapist or chiropractor can address musculoskeletal imbalances. A registered dietitian can guide you through elimination diets safely and effectively. A psychologist or therapist can provide tools for stress management and cognitive behavioral therapy.
The journey to understanding your headaches is often a collaborative one, involving a team of experts who can interpret your headache diary, perform diagnostic tests, and offer tailored interventions.
Conclusion: Embracing the Complexity, Empowering the Self
The question "Is it your neck, your diet, or your stress?" is, in essence, a simplification of a far more intricate reality. It is rarely one, but often a sophisticated interplay of all three, woven into a unique pattern by your individual physiology, genetics, and lifestyle. Your headache is not merely a symptom; it is often a profound message from your body, a signal that something in your internal or external environment is out of balance.
By becoming a meticulous observer of your own body, a diligent cartographer of your daily habits, and an active participant in your healing journey, you transform from a passive recipient of pain into an empowered manager of your health. The unseen tapestry of your headache triggers may be complex, but with awareness, patience, and the right support, you can learn to decipher its threads, unravel its knots, and ultimately, reclaim your peace from the relentless grip of pain. This isn’t just about managing symptoms; it’s about understanding and optimizing your holistic well-being, one careful thread at a time.