Headache or Something More? When to See a Doctor About Your Pain
We’ve all been there. That dull throb behind the eyes, the tension gripping the temples, the relentless pounding that makes the world feel too loud, too bright. Headaches are a ubiquitous part of the human experience, so common that they often blend into the background noise of daily life. For many, they are a fleeting inconvenience, banished by over-the-counter remedies and a moment of quiet. But for others, a headache is a silent question mark, a persistent whisper of anxiety: Is this normal? Or is it something more?
This article is for the knowledgeable reader, the one who understands the intricate dance of the human body and mind, who seeks to differentiate between the benign and the potentially serious. It’s a journey into the nuances of head pain, exploring the vast spectrum from the everyday ache to the urgent alarm, guiding you through the critical moments when a headache ceases to be just a headache and demands the immediate attention of a medical professional. We aim to tell a story not of fear, but of informed vigilance, empowering you to recognize the subtle cues your body might be sending.
The Ubiquitous Ache: A Landscape of Common Headaches
Before delving into the "something more," it’s crucial to acknowledge the sheer prevalence and variety of common, non-life-threatening headaches. Understanding these baseline experiences helps in recognizing deviations.
1. Tension-Type Headaches (TTH): The Everyman’s Burden
The most common type, TTH affects up to 78% of the population at some point. These headaches are often described as a constant, dull ache, pressure, or tightness, like a band squeezing the head. They can affect the forehead, temples, or back of the head and neck. While they can be debilitating, they typically don’t come with the nausea, vomiting, or light/sound sensitivity characteristic of migraines. Stress, poor posture, fatigue, and dehydration are common culprits. They are rarely a cause for serious concern on their own, though chronic tension headaches can significantly impact quality of life.
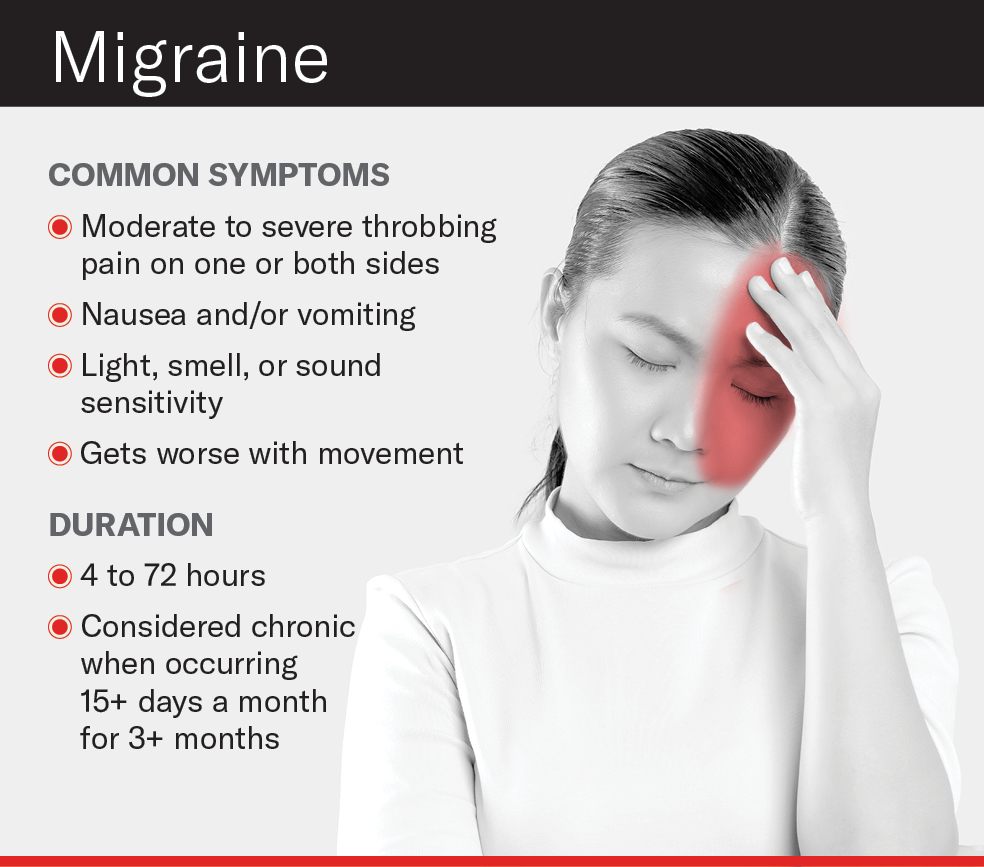
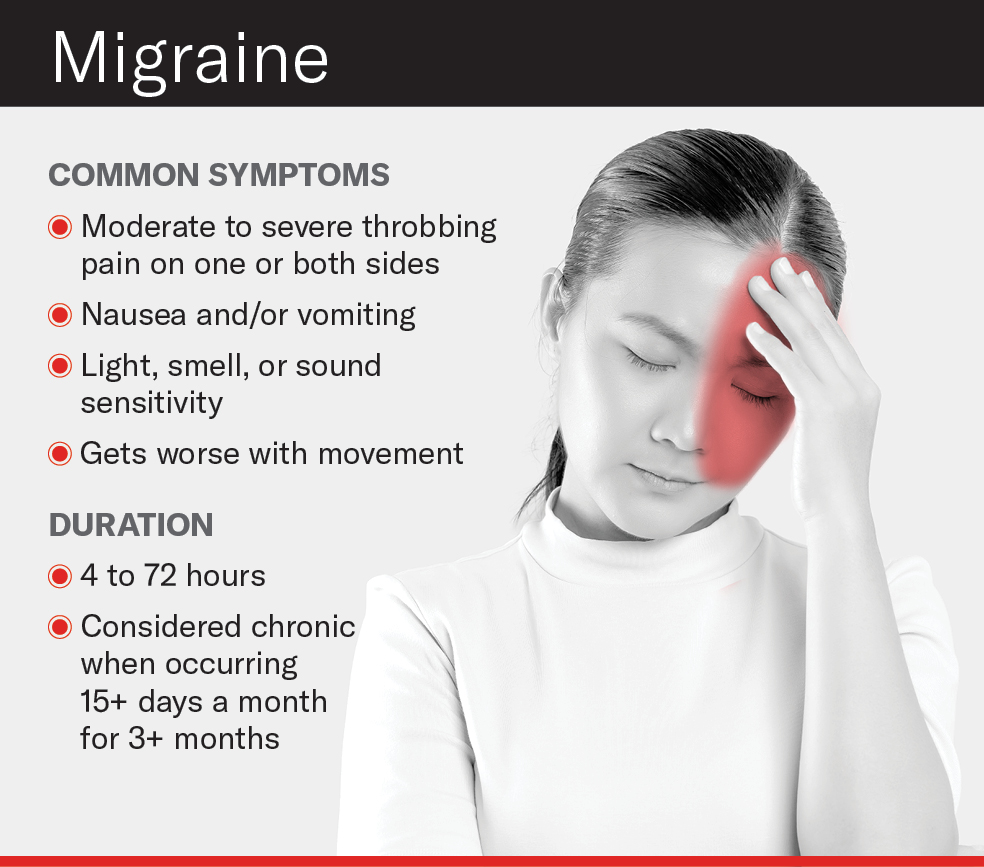
2. Migraine: More Than Just a Bad Headache
Migraines are a complex neurological disorder, not merely a severe headache. Affecting approximately 1 billion people worldwide, they are characterized by moderate to severe throbbing pain, often on one side of the head, accompanied by nausea, vomiting, and extreme sensitivity to light (photophobia) and sound (phonophobia). Some individuals experience an "aura" – transient neurological symptoms like visual disturbances (flashing lights, zigzag lines) – preceding the pain phase. Migraines typically last from 4 to 72 hours and can be profoundly disabling. While the pain is intense, a long-standing history of characteristic migraines, without new or changing symptoms, is generally not indicative of a "something more" scenario.
3. Cluster Headaches: The "Suicide Headaches"
These are rare but excruciatingly painful. Cluster headaches are characterized by severe, unilateral pain, typically around or behind one eye. The pain is often described as stabbing or burning and is accompanied by autonomic symptoms on the affected side, such as a drooping eyelid, tearing, redness of the eye, nasal congestion, or a runny nose. Attacks occur in "clusters" lasting weeks or months, followed by remission periods. The intensity of the pain is such that they’re sometimes called "suicide headaches." While terrifyingly painful, the pattern of cluster headaches, once diagnosed, is usually distinct and not typically a sign of acute intracranial pathology unless the pattern dramatically changes.
4. Sinus Headaches: The Pressure Cooker
Often confused with migraines, sinus headaches are caused by inflammation or infection in the sinuses, the air-filled cavities behind the cheekbones, forehead, and nose. The pain is typically felt as pressure or fullness in the face, forehead, or around the eyes, often worse when bending forward. They are usually accompanied by other sinus symptoms like nasal congestion, discharge, and fever. While uncomfortable, they are rarely dangerous, responding to antibiotics or decongestants.
These common headache types form the baseline, the expected. It is when the pattern shifts, when new symptoms emerge, or when the pain deviates from its known character that our vigilance must sharpen.
The Shifting Sands: When a Headache Becomes a Red Flag
The human body is a master of communication, often through subtle signals. When it comes to headaches, certain characteristics or accompanying symptoms should immediately elevate the pain from a common nuisance to a potential medical emergency. These are the "red flags" that even the most knowledgeable individual should never ignore.
1. The "Thunderclap" Headache: A Sudden, Brutal Assault
Imagine a serene sky suddenly ripped apart by a deafening clap of thunder. This analogy perfectly describes the "thunderclap headache" – an abrupt, explosive onset of the worst headache of your life, reaching its peak intensity within seconds to minutes. This is not a gradual build-up; it’s an instantaneous, brutal assault.
- Why it’s concerning: A thunderclap headache is a classic symptom of a subarachnoid hemorrhage (SAH), often caused by a ruptured cerebral aneurysm. Blood spilling into the subarachnoid space irritates the meninges, leading to this characteristic pain. Other causes can include cerebral venous thrombosis, spontaneous intracranial hypotension, or a reversible cerebral vasoconstriction syndrome (RCVS). Regardless of the specific cause, a thunderclap headache demands immediate emergency medical evaluation. Do not wait.
2. The "Worst Headache of My Life" (WOHL): A Subjective but Critical Marker
While related to the thunderclap, the WOHL doesn’t necessarily have to be thunderclap-fast in onset. It’s a subjective measure, but a crucial one. If a patient, particularly one with a history of headaches, states that this current headache is unequivocally the worst they have ever experienced, it warrants serious investigation.
- Why it’s concerning: This phrase often signals a significant underlying pathology, including SAH, ischemic stroke, hemorrhagic stroke, or other acute intracranial events. The subjective experience of "worst ever" indicates a departure from the individual’s pain baseline, suggesting a new and potentially dangerous process.
3. Headache Accompanied by Neurological Deficits: The Body’s Distress Signals
Our brains control every aspect of our being. When a headache coincides with new neurological symptoms, it’s a clear indication that something is amiss within the central nervous system.
-
Symptoms to watch for:
- Weakness or numbness: In an arm, leg, or one side of the face.
- Difficulty speaking or understanding speech (aphasia): Slurred words, inability to find words, or trouble comprehending others.
- Vision changes: Sudden loss of vision, double vision (diplopia), blurred vision, or visual field defects.
- Loss of balance or coordination (ataxia): Stumbling, difficulty walking straight.
- Confusion or disorientation: Sudden inability to recognize familiar people or places, or to follow simple commands.
- Seizures: New onset of seizures.
- Personality or behavioral changes: Especially if sudden and uncharacteristic.
-
Why it’s concerning: These symptoms strongly suggest an underlying structural or functional problem in the brain, such as a stroke (ischemic or hemorrhagic), a brain tumor, abscess, multiple sclerosis exacerbation, or other space-occupying lesions.
4. Headache with Fever, Stiff Neck, and Altered Mental Status: The Infection Alarm
When a headache is accompanied by fever, a stiff neck (meningismus), and changes in alertness or behavior, it points to a serious infection.
- Why it’s concerning: This triad of symptoms is highly suggestive of meningitis (inflammation of the meninges, the protective membranes surrounding the brain and spinal cord) or encephalitis (inflammation of the brain itself). Both are medical emergencies requiring urgent diagnosis and treatment with antibiotics or antivirals to prevent severe neurological damage or death.
5. Headache Following Head Trauma: The Aftermath of Impact
Any headache that develops or worsens after a blow to the head, even a seemingly minor one, should be evaluated.
- Why it’s concerning: Head trauma can lead to various intracranial injuries, including concussion, epidural hematoma, subdural hematoma, or intracerebral hemorrhage. These can cause pressure on the brain, leading to headache, confusion, vomiting, and loss of consciousness. The symptoms may not appear immediately, sometimes developing hours or even days after the injury, making vigilance crucial.
6. New Headache in an Older Adult (Over 50-60 Years Old): Age-Related Vulnerabilities
As we age, our physiological landscape changes, and so do the potential causes of headaches. A new-onset headache in an individual over 50 or 60 should prompt a higher index of suspicion.
- Why it’s concerning: In this demographic, new headaches can be indicative of conditions like temporal arteritis (giant cell arteritis), a serious inflammatory condition of blood vessels that can lead to blindness if untreated. They can also be a sign of a brain tumor, subdural hematoma (even from minor trauma due to brain atrophy), stroke, or glaucoma. The vascular system also becomes more vulnerable to conditions like carotid artery dissection.
7. Headache in Immunocompromised Individuals or Those with Cancer: Compromised Defenses
Patients with weakened immune systems (due to HIV/AIDS, organ transplantation, chemotherapy, or chronic corticosteroid use) or a history of cancer are at increased risk for specific types of headache-causing conditions.
- Why it’s concerning: Immunocompromised individuals are susceptible to opportunistic infections in the brain (e.g., toxoplasmosis, cryptococcal meningitis, progressive multifocal leukoencephalopathy). Cancer patients, especially those with primary tumors that tend to metastasize to the brain (lung, breast, melanoma, kidney, colon), may develop headaches due to brain metastases or carcinomatous meningitis.
8. Headache that Worsens with Coughing, Straining, or Changes in Position: The Pressure Gauge
A headache that is significantly aggravated by activities that increase intracranial pressure (ICP), such as coughing, sneezing, bending over, or straining during a bowel movement, or one that changes dramatically with position (e.g., much worse when lying down or standing up), is a red flag.
- Why it’s concerning: This pattern can indicate increased intracranial pressure from a mass lesion (tumor, abscess), hydrocephalus, or venous sinus thrombosis. Conversely, headaches that are only present when upright and relieved by lying down can suggest spontaneous intracranial hypotension (a cerebrospinal fluid leak).
9. Headache with Vision Loss, Jaw Claudication, or Scalp Tenderness: Temporal Arteritis Alarm
Specific to older adults, a new headache accompanied by these symptoms is a medical emergency.
- Why it’s concerning: This constellation strongly suggests temporal arteritis (giant cell arteritis). This autoimmune inflammation of medium- and large-sized arteries can lead to irreversible blindness if the ophthalmic artery is affected. Jaw claudication (pain in the jaw when chewing) and tenderness over the temporal artery are highly specific signs.
10. Headache that is Progressively Worsening or Changing in Character: The Insidious Creep
Unlike the sudden thunderclap, some serious conditions manifest with a headache that gradually, but relentlessly, gets worse over days, weeks, or months, or changes its established pattern.
- Why it’s concerning: A progressive headache, especially if it becomes more frequent, more severe, or shifts in its location or quality, can be a symptom of a growing brain tumor, subdural hematoma, or hydrocephalus. It’s the deviation from the norm, the persistent march of pain, that signals a need for evaluation.
The Diagnostic Journey: What Happens When You Seek Help?
When you present to a doctor with a concerning headache, their primary goal is to differentiate between benign causes and those that require urgent intervention. This involves a systematic approach:
1. The History: Unraveling the Story of Your Pain
This is often the most critical part of the evaluation. The doctor will ask detailed questions, aiming to reconstruct the "story" of your headache:
- Onset: When did it start? Was it sudden or gradual?
- Location: Where is the pain felt? Is it unilateral or bilateral?
- Character: What does it feel like? (Throbbing, sharp, dull, pressure, burning).
- Intensity: How severe is it on a scale of 1-10? How does it compare to previous headaches?
- Duration: How long does it last?
- Frequency: How often do you get it?
- Aggravating/Relieving Factors: What makes it worse or better? (Light, sound, movement, medication).
- Associated Symptoms: Any nausea, vomiting, visual changes, weakness, numbness, fever, stiff neck, etc.?
- Past Medical History: Any history of migraines, head trauma, cancer, immunocompromise, or other chronic conditions?
- Medications: What medications are you currently taking? Any recent changes?
- Family History: Any family history of aneurysms, migraines, or other neurological conditions?
2. The Physical and Neurological Examination: Looking for Clues
The doctor will perform a thorough physical exam, including vital signs (blood pressure, heart rate, temperature) and a comprehensive neurological examination. This exam assesses:
- Mental Status: Alertness, orientation, memory, speech.
- Cranial Nerves: Vision, eye movements, facial sensation and movement, hearing, swallowing, tongue movement.
- Motor System: Strength, tone, coordination, gait.
- Sensory System: Sensation to touch, pain, temperature, vibration.
- Reflexes: Deep tendon reflexes.
- Cerebellar Function: Balance and coordination.
- Fundoscopy: Examination of the back of the eye (optic disc) to check for papilledema, which can indicate increased intracranial pressure.
- Meningeal Signs: Checking for neck stiffness (e.g., Kernig’s and Brudzinski’s signs) to rule out meningitis.
3. Investigations: Peeking Inside the Brain
If the history and exam raise concerns, imaging or other tests may be ordered.
- Computed Tomography (CT) Scan: A rapid imaging technique often used in emergency settings. It’s excellent for detecting acute bleeding (e.g., SAH, hemorrhagic stroke), large tumors, or skull fractures.
- Magnetic Resonance Imaging (MRI) Scan: Provides more detailed images of brain tissue, excellent for identifying tumors, abscesses, demyelinating diseases (like MS), ischemic strokes, and subtle structural abnormalities. It’s often preferred for non-acute, concerning headaches.
- Lumbar Puncture (LP) / Spinal Tap: If meningitis, encephalitis, or SAH (with a negative CT) is suspected, a sample of cerebrospinal fluid (CSF) is collected. Analysis can reveal infection, blood, or abnormal cells.
- Blood Tests: May be used to check for infection, inflammation (e.g., ESR for temporal arteritis), or other systemic conditions that could cause headaches.
- Magnetic Resonance Angiography (MRA) or CT Angiography (CTA): Used to visualize blood vessels in the brain, helpful for detecting aneurysms, dissections, or other vascular abnormalities.
- Electroencephalogram (EEG): Less common for headache diagnosis itself, but may be used if seizures are suspected.
The "Something More": A Deeper Dive into Serious Conditions
To truly understand "when to worry," it’s helpful to have a basic grasp of the serious conditions that manifest with headache as a primary symptom.
1. Stroke (Ischemic or Hemorrhagic): The Brain Under Attack
A stroke occurs when blood flow to a part of the brain is interrupted (ischemic) or when a blood vessel ruptures and bleeds into the brain (hemorrhagic). Headaches are more common with hemorrhagic strokes, often described as sudden and severe. Ischemic strokes can also cause headache, especially if large vessels are involved. The key is the accompanying neurological deficits (weakness, speech changes, vision loss) that are acute in onset.
2. Cerebral Aneurysm (Ruptured or Unruptured): The Silent Bomb
An aneurysm is a weak, bulging spot in a blood vessel wall. An unruptured aneurysm often causes no symptoms, but if it ruptures, it leads to a subarachnoid hemorrhage, characterized by the classic "thunderclap" headache, often with neck stiffness, nausea, and loss of consciousness. Early detection of unruptured aneurysms is crucial, as they can sometimes be treated before rupture.
3. Brain Tumor: The Insidious Invader
Headaches caused by brain tumors are often progressive, meaning they gradually worsen over time. They might be worse in the morning, awaken the patient from sleep, or be aggravated by coughing or straining. The headache is typically not the only symptom; neurological deficits, seizures, or personality changes often accompany it. The type and location of the tumor influence the specific symptoms.
4. Meningitis and Encephalitis: The Brain’s Fiery Battle
As discussed, these infections of the brain and its surrounding membranes cause severe headache, fever, stiff neck, and altered mental status. They are life-threatening conditions requiring immediate medical attention.
5. Temporal Arteritis (Giant Cell Arteritis): The Threat to Vision
This inflammatory disease primarily affects arteries in the head and neck, most commonly the temporal arteries. It causes a new-onset, often throbbing headache, typically on one side of the head, often accompanied by scalp tenderness, jaw pain with chewing (claudication), and potential vision loss. It is a medical emergency due to the risk of permanent blindness.
6. Idiopathic Intracranial Hypertension (Pseudotumor Cerebri): Pressure Without a Tumor
This condition involves increased pressure within the skull, mimicking a brain tumor, but without an actual tumor. It primarily affects overweight women of childbearing age. Symptoms include chronic headache (often worse with straining), pulsatile tinnitus (a whooshing sound in the ears), and visual disturbances due to swelling of the optic nerve (papilledema). While not immediately life-threatening, it can cause permanent vision loss if untreated.
7. Carbon Monoxide Poisoning: The Invisible Killer
Often overlooked, carbon monoxide (CO) is a colorless, odorless gas. Exposure can cause headaches, nausea, dizziness, and confusion. It’s crucial to consider CO poisoning in cases of new-onset headaches affecting multiple people in the same location (e.g., a household). Prompt diagnosis and removal from the source are vital.
8. Hydrocephalus: The Fluid Buildup
Hydrocephalus is a condition in which excess cerebrospinal fluid (CSF) accumulates in the brain’s ventricles, leading to increased intracranial pressure. This can cause headaches, nausea, vomiting, vision problems, and cognitive changes. It can be congenital or acquired due to infection, trauma, or tumors.
The Psychological Burden: Navigating Uncertainty
Beyond the physical pain, the "something more" question carries a significant psychological burden. The internet is a double-edged sword, offering both information and anxiety. Self-diagnosis can lead to unnecessary panic, but ignoring genuine red flags can have dire consequences.
It’s natural to feel anxious when confronted with unusual symptoms. The fear of the unknown, of a life-altering diagnosis, is profound. This is why a trusting relationship with your healthcare provider is paramount. They are trained to navigate this complex landscape, to interpret the subtle clues, and to guide you through the diagnostic process with empathy and expertise.
Remember, the vast majority of headaches are benign. The purpose of this article is not to induce panic, but to equip you with the knowledge to discern when vigilance is warranted. Trusting your instincts, especially when something feels "off," is a powerful tool in advocating for your own health.
Empowerment Through Vigilance: Your Role in the Story
You are an active participant in your healthcare story. Here’s how you can empower yourself:
- Know Your Baseline: Understand your typical headache patterns. What triggers them? How severe are they? What helps? This knowledge is invaluable when describing a new or changed headache.
- Keep a Headache Diary: For recurrent headaches, a diary can be immensely helpful. Note the date, time, severity, location, associated symptoms, potential triggers, and medications taken. This provides objective data for your doctor.
- Communicate Clearly: When speaking with your doctor, be precise. Use descriptive language for your pain. Be honest about all symptoms, even seemingly unrelated ones. Don’t downplay your concerns.
- Trust Your Gut: If you feel that something is seriously wrong, even if you can’t articulate why, seek medical attention. Doctors are trained to listen to these intuitions, which are often rooted in subconscious recognition of changes in your body.
- Don’t Hesitate: For any of the red flag symptoms mentioned, do not delay. Go to the emergency room or call for emergency medical services immediately. Time is often critical in preventing permanent damage in many of these conditions.
- Seek Second Opinions: If you feel your concerns are not being adequately addressed, or if a diagnosis doesn’t feel right, don’t hesitate to seek a second opinion.
Conclusion: The Art of Discernment
The story of headaches is a complex tapestry, woven with threads of common discomfort and the stark reality of serious illness. For the knowledgeable individual, the goal is not to live in perpetual fear of every ache, but to cultivate a discerning eye, to understand the language of the body.
The majority of headaches will remain just that – headaches, a transient inconvenience. But for a select few, they are harbingers, silent alarms signaling a deeper, more urgent narrative. By understanding the red flags, by knowing when to listen intently to your body, and by seeking timely professional help, you transform from a passive recipient of pain into an informed advocate for your health. The difference between a simple headache and "something more" can be profound, and recognizing that distinction is an act of self-preservation, a testament to the power of informed vigilance.