Electrolytes and Agony: The Chemical Imbalance Behind Dehydration Headaches
The morning after a long flight, a strenuous hike, or perhaps even a celebratory evening, it often strikes with merciless precision: a dull, throbbing ache that settles behind the eyes, presses against the temples, and turns the simplest movements into acts of agony. This is the dehydration headache, a familiar torment for many, yet its underlying mechanisms remain a complex symphony of cellular distress and chemical imbalance. It’s more than just a lack of water; it’s a profound disruption of the body’s delicate internal environment, a story etched in the shifting concentrations of charged particles we call electrolytes. For the knowledgeable mind, understanding this intricate dance of ions and fluid is to peel back the curtain on one of the body’s most common cries for help.
The Grand Orchestra of Life: What Are Electrolytes?
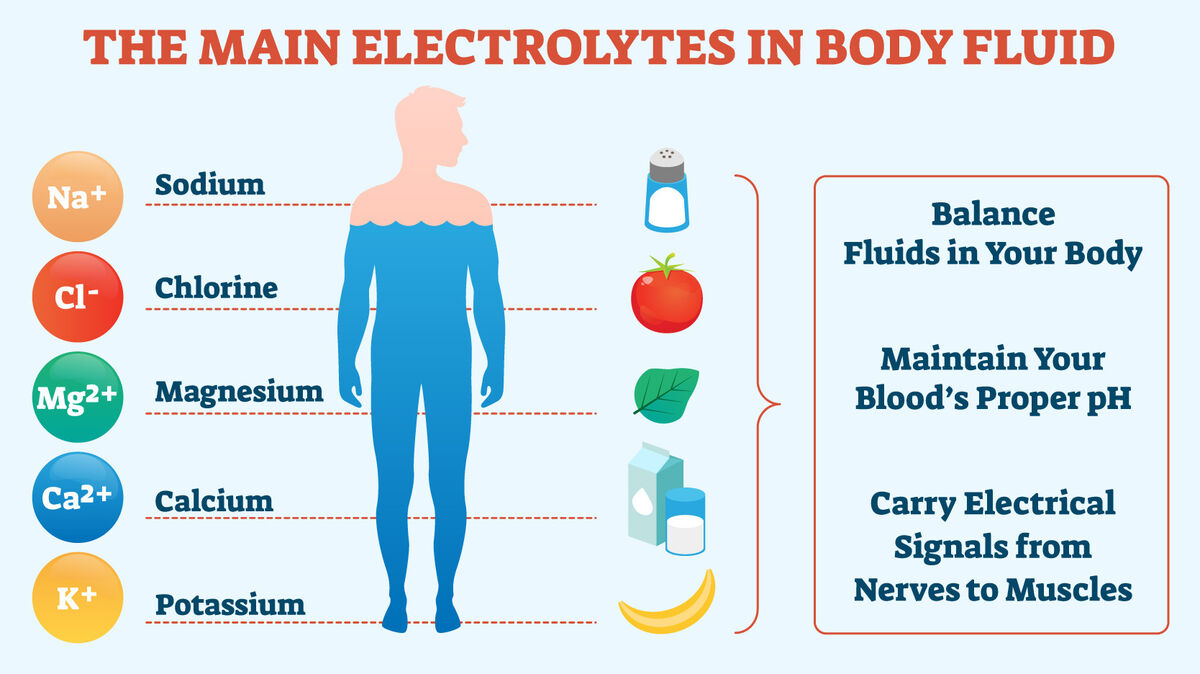
Before we delve into the agony, we must first understand the unsung heroes of our physiology: electrolytes. These are minerals in your body that have an electric charge. They are found in your blood, urine, tissues, and other body fluids. But their mere presence is not enough; their precise balance is paramount for nearly every bodily function. Imagine the human body as a vast, complex city, with every cell a tiny, bustling apartment. Electrolytes are the electrical grid, the plumbing system, and the communication network, all rolled into one. Without them, the city grinds to a halt.
Let’s introduce the principal players in this vital orchestra:
- Sodium (Na+): The Extracellular Maestro. This is the most abundant electrolyte in the extracellular fluid (outside cells). Sodium is the primary determinant of plasma osmolality, dictating where water goes. It’s critical for nerve impulse transmission, muscle contraction, and maintaining blood pressure. The sodium-potassium pump, a molecular marvel found in virtually every cell membrane, actively transports sodium out of the cell and potassium in, creating electrochemical gradients essential for life.
- Potassium (K+): The Intracellular Conductor. In contrast to sodium, potassium is predominantly found inside cells. It plays a crucial role in nerve signal transmission, muscle contractions (especially the heart), and maintaining intracellular fluid volume. Its careful balance with sodium across cell membranes is fundamental to cellular excitability and overall function.
- Chloride (Cl-): The Balancing Act. Chloride is the most abundant anion (negatively charged ion) in the extracellular fluid. It works in tandem with sodium to maintain fluid balance and blood pressure. It’s also a crucial component of stomach acid (hydrochloric acid) and plays a role in acid-base balance.
- Magnesium (Mg2+): The Silent Workhorse. Often overlooked, magnesium is a cofactor in over 300 enzymatic reactions in the body. It’s essential for muscle and nerve function, blood glucose control, blood pressure regulation, and bone health. It’s deeply involved in energy production, protein synthesis, and DNA replication. A deficiency can have widespread effects, including contributing to migraines and muscle cramps.
- Calcium (Ca2+): The Structural and Signaling Giant. Known for its role in bone and teeth formation, calcium also serves as a vital signaling molecule. It’s indispensable for muscle contraction, nerve impulse transmission, hormone secretion, and blood clotting. Its concentration in the blood is tightly regulated.
- Bicarbonate (HCO3-): The pH Stabilizer. Though not always top-of-mind, bicarbonate is a critical component of the body’s pH buffering system, ensuring that blood acidity remains within a narrow, life-sustaining range.
Together, these electrolytes maintain the delicate balance known as homeostasis. They enable nerve cells to fire, muscles to contract, the heart to beat rhythmically, and fluids to distribute correctly throughout the body. When this balance is disrupted, particularly by dehydration, the body’s entire system begins to falter, leading to a cascade of distress signals, chief among them the dreaded headache.
The Villain Emerges: Dehydration – More Than Just Thirst
Dehydration is not merely the sensation of thirst; it is a state where the body lacks sufficient water to carry out its normal physiological functions. It’s a deficit in total body water, which can arise from inadequate fluid intake, excessive fluid loss, or a combination of both. Think of the body as a carefully irrigated garden. When the water supply dwindles, the plants begin to wilt, their functions compromised.
Causes of dehydration are manifold:
- Insufficient Intake: Simply not drinking enough water, especially during physical activity, hot weather, or when preoccupied.
- Excessive Loss:
- Sweating: During exercise, fever, or exposure to high temperatures.
- Vomiting and Diarrhea: Common in gastrointestinal illnesses, leading to rapid fluid and electrolyte depletion.
- Increased Urination: Due to certain medications (diuretics), uncontrolled diabetes (osmotic diuresis), or conditions like diabetes insipidus.
- Burns: Extensive burns can lead to significant fluid loss through damaged skin.
The body’s initial response to water loss is sophisticated. Osmoreceptors in the hypothalamus, the brain’s control center, detect an increase in plasma osmolality (the concentration of solutes in the blood). This triggers two crucial responses: the sensation of thirst, compelling us to drink, and the release of Antidiuretic Hormone (ADH), also known as vasopressin, from the pituitary gland. ADH signals the kidneys to conserve water, producing more concentrated urine.
However, if fluid intake doesn’t match fluid loss, these compensatory mechanisms eventually become overwhelmed. As the body continues to lose water, plasma volume decreases, leading to a reduction in blood pressure. The heart compensates by beating faster, trying to maintain adequate circulation. Blood becomes thicker, making it harder for the heart to pump, and the delivery of oxygen and nutrients to tissues, including the brain, becomes less efficient. This escalating physiological stress sets the stage for the dramatic electrolyte imbalances that underpin the dehydration headache.
The Cascade of Imbalance: Electrolytes Under Duress
When dehydration takes hold, the precise concentrations of electrolytes within and outside our cells begin to shift dramatically. This is where the story of agony truly begins. The most immediate and impactful consequence of simple water deprivation is often hypernatremia – an elevated concentration of sodium in the blood.
Here’s how it unfolds: As water is lost from the body, the remaining extracellular fluid becomes more concentrated. Since sodium is the primary determinant of extracellular osmolality, its concentration rises. This creates an osmotic gradient: the extracellular fluid is now "saltier" than the fluid inside the cells. In a desperate attempt to restore equilibrium, water is drawn out of cells and into the extracellular space. This cellular dehydration affects every cell in the body, but its impact on the brain is particularly profound and painful.
While sodium takes center stage, other electrolytes are also affected:
- Potassium: While severe dehydration often leads to hypernatremia, potassium levels can be more complex. In cases of significant gastrointestinal losses (vomiting, diarrhea), hypokalemia (low potassium) can occur due to direct loss. However, in pure water deprivation, potassium levels might appear relatively normal initially, but its intracellular-extracellular balance can be disturbed as cells shrink. Aldosterone, a hormone released in response to decreased blood volume, promotes sodium reabsorption but also potassium excretion, potentially exacerbating potassium losses.
- Magnesium and Calcium: These electrolytes, vital for countless cellular processes, can also be affected by prolonged or severe dehydration. Changes in blood volume and kidney function can alter their excretion and reabsorption, leading to subtle or significant imbalances that contribute to the overall malaise and neurological symptoms.
The "ripple effect" of these imbalances is crucial. A shift in one electrolyte often triggers compensatory changes in others, attempting to maintain neutrality and function. But these compensatory mechanisms have their limits. When the electrolyte balance is severely disrupted, cellular functions become impaired, leading to the symptoms we associate with dehydration, including the headache.
The Brain’s Cry for Help: Unraveling the Dehydration Headache
The brain, encased within the rigid confines of the skull, is exquisitely sensitive to changes in its fluid environment. It floats in cerebrospinal fluid (CSF), cushioned from impacts. But this protective arrangement also makes it vulnerable to volume changes. The dehydration headache is not a simple pain; it is a complex neurological response to cellular distress, primarily driven by a phenomenon known as cerebral shrinkage.
1. Cerebral Shrinkage: The Primary Culprit
As discussed, when dehydration leads to hypernatremia, the extracellular fluid becomes hypertonic (more concentrated). According to the principles of osmosis, water moves from an area of lower solute concentration to an area of higher solute concentration to equalize the osmotic pressure. This means water is drawn out of the brain cells and into the surrounding extracellular fluid. As brain cells lose water, the brain itself subtly shrinks.
This seemingly minor volume change has dramatic consequences. The brain is anchored within the skull by meninges (protective membranes like the dura mater) and by bridging veins that connect the brain’s surface to the venous sinuses embedded in the dura. When the brain shrinks, it pulls away from the dura mater and stretches these pain-sensitive structures. The nociceptors (pain receptors) embedded in the dura mater and the walls of the bridging veins are activated, sending signals that the brain interprets as pain. This stretching and tension are believed to be a major source of the characteristic throbbing, diffuse pain of a dehydration headache.
2. Vascular Mechanisms: A Convoluted Dance
Beyond structural changes, dehydration profoundly impacts the cerebral vasculature:
- Vasoconstriction and Vasodilation: Initially, dehydration can lead to compensatory cerebral vasoconstriction to maintain blood pressure and perfusion. However, prolonged dehydration can impair this regulation. The brain’s attempt to compensate for reduced blood flow or localized hypoxia might lead to a rebound vasodilation. The stretching of pain receptors in the walls of dilated blood vessels can contribute to the throbbing quality of the headache.
- Adenosine Accumulation: Under metabolic stress, such as that induced by reduced blood flow and cellular dehydration, cells release adenosine. Adenosine is a potent vasodilator, meaning it widens blood vessels. While this might seem beneficial for blood flow, excessive vasodilation can trigger pain receptors. Furthermore, adenosine is known to play a role in pain perception and has been implicated in other types of headaches, including migraines. Its accumulation in the dehydrated brain could amplify pain signals.
- Inflammation: Dehydration can induce a low-grade inflammatory state throughout the body, including the brain. The release of pro-inflammatory cytokines can sensitize pain pathways and contribute to the overall feeling of malaise and headache.
3. Neurotransmitter Imbalance: The Chemical Scream
The delicate balance of neurotransmitters, the chemical messengers of the brain, is also susceptible to electrolyte imbalances and osmotic stress.
- Serotonin: This neurotransmitter is well-known for its role in mood, sleep, and appetite, but also for its complex involvement in migraine pathophysiology. Dehydration can disrupt serotonin regulation, potentially contributing to headache pain or even triggering migraine-like symptoms in susceptible individuals.
- Magnesium and NMDA Receptors: Magnesium plays a critical role in modulating NMDA receptors, which are involved in pain transmission and neuronal excitability. A reduction in intracellular magnesium due to dehydration could lead to increased neuronal excitability and enhanced pain perception.
- Other Neurotransmitters: The overall osmotic stress and altered cellular function can broadly impact the synthesis, release, and reuptake of various neurotransmitters, further disrupting normal brain function and contributing to pain.
4. The "Thirst" Signal as Pain: Some theories suggest that the brain interprets the intense physiological distress and the strong drive to rehydrate as a form of pain. The same hypothalamic regions that register thirst are also intimately connected with pain pathways, blurring the lines between these distinct sensations.
In essence, the dehydration headache is the brain’s multi-faceted scream for water. It’s a combination of physical tension from shrinking tissues, vascular chaos, and chemical dysregulation, all converging to create a profoundly unpleasant experience.
Beyond the Headache: Other Symptoms and Their Roots
The headache is often the most prominent symptom, but it rarely travels alone. Dehydration is a systemic problem, and its other manifestations are equally rooted in the disruption of fluid and electrolyte balance:
- Fatigue and Lethargy: Reduced blood volume means less efficient oxygen and nutrient delivery to muscles and organs, leading to a profound sense of tiredness. Cellular dehydration impairs metabolic processes, further depleting energy reserves.
- Dizziness and Lightheadedness (Orthostatic Hypotension): When blood volume is low, the body struggles to maintain blood pressure, especially when changing positions (e.g., standing up quickly). This sudden drop in blood pressure, known as orthostatic hypotension, leads to transient cerebral hypoperfusion, causing dizziness and lightheadedness.
- Muscle Cramps: This is a classic symptom directly linked to electrolyte imbalances, particularly of sodium, potassium, and magnesium. These ions are crucial for proper muscle contraction and relaxation. When their concentrations are out of whack, muscles can involuntarily seize up.
- Cognitive Impairment and Irritability: Brain cells, deprived of water and operating in a chemically imbalanced environment, cannot function optimally. This manifests as difficulty concentrating, impaired memory, slower reaction times, and increased irritability.
- Dry Mouth and Decreased Urine Output: These are direct indicators of the body’s attempts to conserve water. Reduced saliva production leads to dry mouth, and the kidneys, under the influence of ADH, produce less, more concentrated urine.
- Increased Heart Rate: As mentioned, the heart works harder to pump a reduced volume of thicker blood, trying to maintain adequate circulation throughout the body.
The interconnectedness of these symptoms paints a clear picture: dehydration is not a localized issue but a systemic crisis, with the headache being just one of its most potent warning signals.
The Body’s Resilience and the Path to Recovery
Despite the profound distress dehydration can cause, the body possesses remarkable resilience. The path to recovery, however, is not simply about gulping down large quantities of water. For a truly effective and safe recovery, understanding the principles of rehydration is key.
The immediate goal is to replenish lost fluids and restore electrolyte balance.
- Water Alone vs. Electrolyte Solutions: For mild to moderate dehydration, plain water is often sufficient, as the kidneys will work to re-establish electrolyte balance from existing reserves. However, for more significant dehydration, especially if accompanied by substantial electrolyte losses (e.g., through heavy sweating, vomiting, or diarrhea), water alone might not be enough and can, in rare cases, even exacerbate hyponatremia if rapidly consumed in large volumes.
- Oral Rehydration Solutions (ORS): These specially formulated solutions are the gold standard for treating moderate to severe dehydration. They contain precise amounts of water, sodium, potassium, chloride, and glucose. The glucose is crucial because it facilitates the co-transport of sodium and water across the intestinal lining, speeding up rehydration. This scientific design makes ORS far more effective than plain water or sugary drinks for rapid electrolyte and fluid restoration.
- Slow and Steady Rehydration: For severe dehydration, especially when there has been a prolonged period of hypernatremia, rehydration must be gradual. Rapid correction of hypernatremia can cause a sudden shift of water back into brain cells, leading to cerebral edema (brain swelling), which can be more dangerous than the dehydration itself. The body needs time to safely adjust its osmotic gradients.
- Prevention is Key: Proactive hydration is the best defense. This means consistently drinking fluids throughout the day, increasing intake during exercise, hot weather, or illness. Understanding individual needs is important; athletes, individuals in hot climates, and those with certain medical conditions will require more fluids.
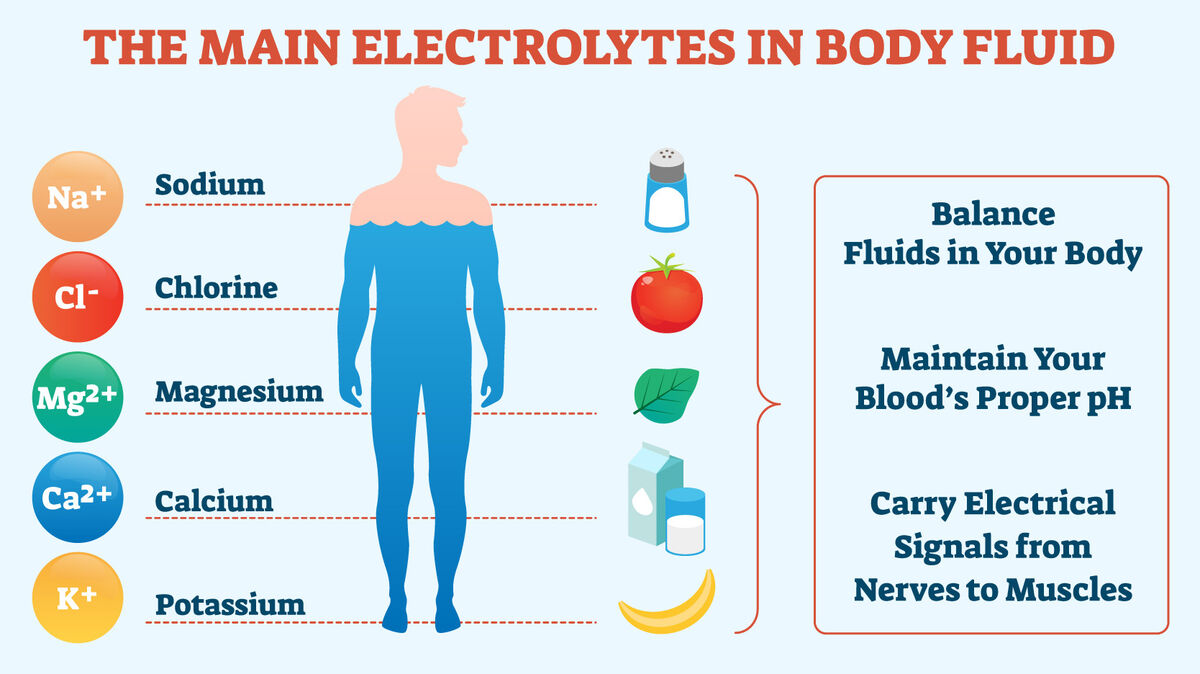
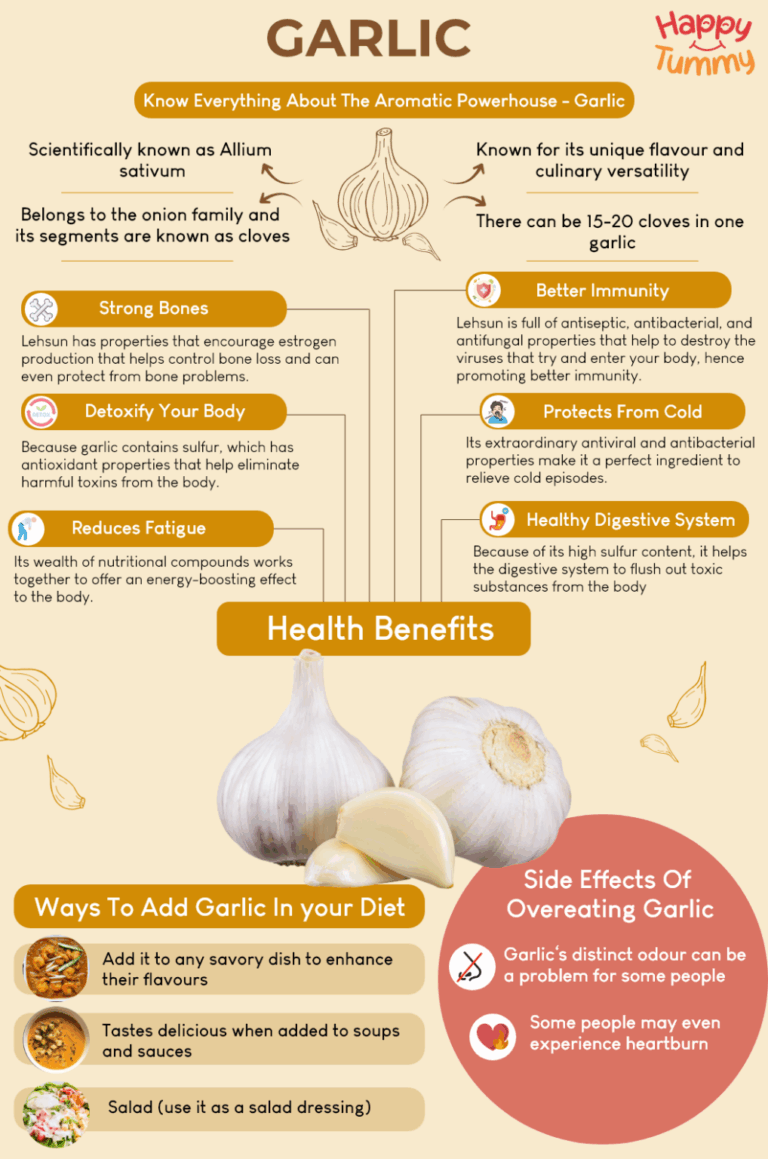
Dietary Sources of Electrolytes: While ORS are for acute correction, a balanced diet is crucial for maintaining electrolyte homeostasis long-term.
- Sodium: Found in table salt, processed foods, and many natural foods.
- Potassium: Abundant in fruits (bananas, oranges), vegetables (spinach, potatoes), legumes, and dairy.
- Magnesium: Rich sources include leafy green vegetables, nuts, seeds, whole grains, and dark chocolate.
- Calcium: Dairy products, fortified plant milks, leafy greens, and fish with edible bones.
Complexities and Nuances: When It’s More Than Just Dehydration
While the mechanisms of dehydration headaches are well-established, it’s important to acknowledge the nuances and potential overlaps with other conditions.
- Distinguishing from Other Headache Types: Dehydration headaches often present as a dull, diffuse, bilateral pain, sometimes with a throbbing quality. However, they can sometimes mimic tension headaches or even trigger migraines in susceptible individuals. Migraines, for instance, are often unilateral, more severe, and accompanied by other symptoms like aura, nausea, and sensitivity to light and sound. A thorough understanding of one’s own headache patterns is crucial.
- The Interplay with Caffeine Withdrawal: Many individuals consume caffeine regularly, which is a diuretic. Abrupt cessation of caffeine can lead to withdrawal headaches, often confused with dehydration headaches. While caffeine withdrawal can also exacerbate dehydration, the primary mechanism of the withdrawal headache is related to cerebral blood vessel dilation and adenosine signaling, making it a distinct entity, though sometimes co-occurring.
- Underlying Medical Conditions: Certain medical conditions can predispose individuals to dehydration or mimic its symptoms. Diabetes insipidus, for example, causes excessive urination due to a problem with ADH, leading to severe dehydration. Kidney disease can impair the body’s ability to regulate fluid and electrolytes. Uncontrolled diabetes mellitus can cause osmotic diuresis and significant fluid loss. Always consider that persistent or severe symptoms might point to an underlying medical issue requiring professional attention.
- The Dangers of Over-Hydration (Hyponatremia): While rare in healthy individuals, excessive water intake, especially in a short period, can lead to hyponatremia (low blood sodium). This occurs when the body’s sodium is diluted, causing water to move into cells, including brain cells, leading to cerebral edema. This condition can be life-threatening, particularly in endurance athletes who over-hydrate with plain water without sufficient electrolyte replenishment. It underscores the importance of balanced fluid intake.
Conclusion: The Story’s End – A Deeper Understanding
The agony of a dehydration headache, that relentless pounding behind the eyes, is far more than a simple nuisance. It is the body’s sophisticated, multi-layered chemical alarm system, a narrative woven from the intricate dance of fluids and electrolytes. From the moment water loss concentrates the extracellular fluid, triggering the subtle shrinkage of brain cells and the stretching of delicate membranes, to the complex vascular and neurotransmitter dysregulations, the story of this common affliction is one of profound physiological disruption.
The master regulator, sodium, dictates the osmotic shifts that draw water from within our very neurons. Potassium, magnesium, and calcium, vital for cellular electricity and function, find their delicate balance disturbed. The brain, our command center, responds with a cascade of pain signals – structural tension, vascular chaos, and chemical imbalance – all converging to demand rehydration.
For the knowledgeable, this understanding transforms a mere symptom into a compelling insight into the body’s exquisite design and its vulnerabilities. It empowers us not only to reach for a glass of water but to appreciate the intricate cellular symphony that plays within us every moment. Prevention, through mindful hydration and a balanced diet rich in electrolytes, becomes not just a habit, but an act of respect for the remarkable chemical orchestration that sustains life itself. The story of electrolytes and agony is a reminder that even in our most common discomforts, there lies a universe of scientific wonder waiting to be explored.