The 3-Hour Fix: Deconstructing the Dehydration Headache and Its Rapid Relief
The relentless throb, a dull pressure behind the eyes, the subtle nausea, and the insidious fatigue – the dehydration headache is a universally recognized antagonist. It’s a familiar foe that strikes with a particular vengeance after a long flight, a strenuous workout, an evening of revelry, or simply a day of insufficient fluid intake. We’ve all been there, cursing our forgetfulness or our circumstances, desperately seeking respite.
But what if relief wasn’t a distant hope, but a tangible, achievable goal within a surprisingly short timeframe? What if we told you that for many, the journey from the throes of a dehydration headache to a state of equilibrium and comfort could be accomplished in as little as three hours? This isn’t a miraculous cure-all for every headache, nor is it an excuse to ignore the early warning signs of dehydration. Instead, it’s a scientifically grounded understanding of the body’s remarkable capacity for self-correction when given the right tools, promptly applied.
This article delves deep into the anatomy of the dehydration headache, dissecting its physiological origins, exploring the nuanced mechanics of rehydration, and ultimately, constructing a narrative around the achievable "3-Hour Fix." Our journey will be one of understanding, empowering you not just to alleviate the immediate discomfort, but to truly comprehend the intricate dance of fluids and electrolytes that keeps our bodies, and particularly our brains, functioning optimally. Prepare to transform your approach to this common affliction, moving from passive suffering to proactive, informed relief.
Part 1: The Enemy Unmasked – What is a Dehydration Headache?
To truly appreciate the speed of recovery, we must first understand the depth of the problem. A dehydration headache is not merely a symptom; it is a complex physiological protest from a brain under duress. Unlike tension headaches or migraines, its roots are fundamentally tied to fluid dynamics and cellular homeostasis.
Imagine the brain, a delicate organ, suspended within the skull, cushioned by cerebrospinal fluid (CSF). This fluid acts as a protective buffer, absorbing shocks and maintaining a stable environment. When dehydration sets in, the body prioritizes maintaining blood volume, often drawing water from other compartments, including the brain. This isn’t a dramatic shrinkage, but a subtle yet significant reduction in brain volume. The brain, now slightly less buoyant, can exert a gentle pull on the meninges – the pain-sensitive membranes that encase it. This pulling, stretching, and subtle friction against the skull’s inner surface are key contributors to the characteristic dull, aching pain.
Beyond this mechanical stress, dehydration wreaks havoc on the intricate chemical balance within the brain. The brain’s cells, like all cells, rely on a precise concentration of electrolytes – sodium, potassium, chloride, magnesium – to facilitate nerve impulse transmission and maintain cellular integrity. Dehydration disrupts this delicate osmolality, leading to a shift in fluid between intracellular and extracellular spaces. Neurons, exquisitely sensitive to changes in their environment, can become irritable or function suboptimally, further contributing to the headache sensation.
Furthermore, dehydration often leads to a decrease in overall blood volume. The body’s compensatory response involves vasoconstriction in some areas to maintain blood pressure, but ironically, this can sometimes be followed by reactive vasodilation, particularly in the cerebral blood vessels. The swelling and throbbing of these blood vessels within the confined space of the skull can also contribute significantly to the pulsatile nature of many dehydration headaches. The intricate vascular network surrounding the brain is highly sensitive to changes in blood flow and pressure, and even subtle shifts can trigger nociceptive (pain) pathways.
It’s also worth noting the role of antidiuretic hormone (ADH), also known as vasopressin. In a dehydrated state, ADH levels rise, prompting the kidneys to reabsorb more water. While this is crucial for conserving fluid, the systemic effects of altered hormone levels can also influence neurological function and contribute to the overall malaise.
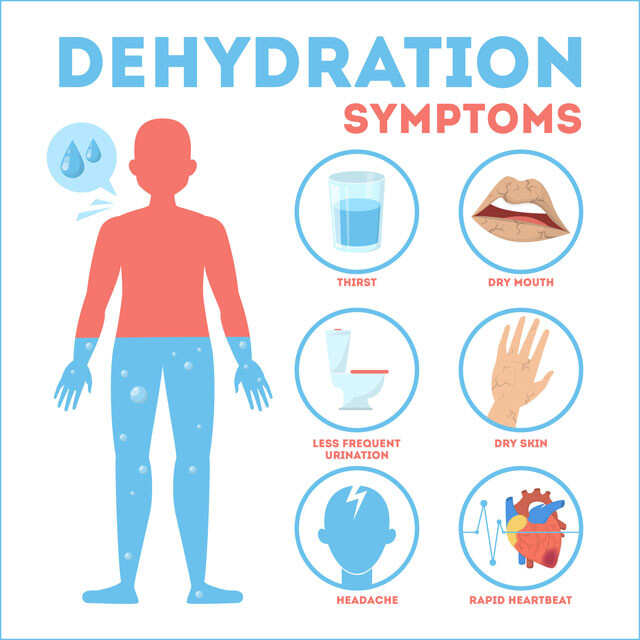
In essence, the dehydration headache is a symphony of discomfort orchestrated by:
- Mechanical Stress: Brain volume reduction leading to meningeal traction.
- Osmotic Dysregulation: Imbalance of electrolytes affecting neuronal function.
- Vascular Changes: Altered cerebral blood flow and vasodilation.
- Systemic Distress: The overall impact of fluid depletion on vital organ systems.
Understanding these underlying mechanisms is crucial, as it illuminates why strategic rehydration is so effective and why simply popping a painkiller offers only superficial, temporary relief. We’re not just masking a symptom; we’re addressing the core physiological imbalance.
Part 2: The Silent Saboteurs – Causes and Risk Factors
While "not drinking enough water" is the primary culprit, the pathways to dehydration are varied and often insidious. A knowledgeable audience understands that dehydration isn’t just about thirst; it’s about the net loss of fluids and electrolytes from the body, exceeding intake.
Common Culprits:
- Strenuous Physical Activity: Especially in hot or humid environments. Sweating is the body’s cooling mechanism, but it comes at the cost of significant fluid and electrolyte loss. Athletes are particularly susceptible, as their fluid needs are dramatically increased.
- Environmental Factors: Prolonged exposure to high temperatures, low humidity, or high altitudes can accelerate fluid loss through sweat and respiration.
- Alcohol Consumption: Alcohol is a diuretic. It inhibits the release of ADH, causing the kidneys to excrete more water than they reabsorb, leading to increased urination and rapid fluid depletion. This is a primary reason for the dreaded "hangover headache."
- Illness: Vomiting, diarrhea, and fever all lead to significant fluid and electrolyte loss. Vomiting expels fluids directly, diarrhea prevents absorption, and fever increases metabolic rate and evaporative cooling.
- Certain Medications: Diuretics prescribed for conditions like hypertension or heart failure intentionally increase urine output, making adequate fluid intake paramount. Some antihistamines or decongestants can also have drying effects.
- Caffeine: While often debated, caffeine can have a mild diuretic effect, particularly in individuals not accustomed to it or consumed in large quantities. More significantly, it can mask thirst cues, leading to under-hydration.
- Age: Both the very young and the elderly are at higher risk. Infants have a higher surface-area-to-volume ratio, leading to greater evaporative loss, and their thirst mechanisms are less developed. Older adults often have a diminished sense of thirst, reduced kidney function, and may be on medications that affect fluid balance.
- Poor Hydration Habits: Simply neglecting to drink water throughout the day, especially when engrossed in work or activities, is a common, often underestimated, cause.
Recognizing these risk factors is the first step in prevention. Understanding when and why your body might be losing more fluid than usual allows for proactive measures, potentially averting the headache altogether.
Part 3: The Race Against Time – Understanding the 3-Hour Window
Here lies the crux of our discussion: the "3-Hour Fix." This isn’t an arbitrary number plucked from thin air; it represents a realistic, achievable timeframe for significant relief from a moderate dehydration headache through strategic rehydration. It’s a testament to the body’s efficient mechanisms for fluid absorption and distribution.
The Physiology of Rapid Rehydration:
- Ingestion and Gastric Emptying: The moment you swallow water or an electrolyte solution, it begins its journey. The stomach typically empties fluids relatively quickly, though factors like temperature, osmolarity, and volume can influence this. Cool, hypotonic (lower concentration than blood) or isotonic (same concentration) fluids are generally absorbed faster.
- Small Intestine Absorption: This is where the magic happens. The small intestine is the primary site of water and electrolyte absorption. Its vast surface area, lined with villi and microvilli, is incredibly efficient. Water moves passively via osmosis, driven by osmotic gradients created by the active transport of electrolytes, particularly sodium. Oral Rehydration Solutions (ORS) are specifically formulated to optimize this process, providing glucose to facilitate sodium and water co-transport.
- Circulation and Distribution: Once absorbed into the bloodstream, fluids are rapidly circulated throughout the body. Within minutes, blood volume begins to normalize. This improved circulation aids in delivering water and electrolytes to thirsty cells.
- Cellular Rehydration: As blood osmolality decreases (becomes less concentrated) due to increased water content, the osmotic gradient reverses. Water then moves from the blood into the interstitial fluid and, crucially, into the dehydrated cells, including those in the brain. This re-establishes cell volume and reduces the mechanical stress on the meninges.
- Renal Adjustment: Concurrently, the kidneys, under the influence of decreasing ADH levels, begin to excrete excess solutes and normalize electrolyte balance. While this takes longer for full homeostatic regulation, the immediate influx of water begins the process of fluid balance restoration.
Why 3 Hours?
- Initial Absorption (0-30 minutes): Significant fluid absorption occurs within the first half-hour. You’ll often feel an immediate sense of relief from thirst and dry mouth, and the body’s internal alarms begin to quiet.
- Circulatory and Cellular Impact (30-90 minutes): Over the next hour, enough fluid has been absorbed and distributed to significantly impact blood volume, reduce blood osmolality, and initiate cellular rehydration, particularly in sensitive tissues like the brain. The headache often starts to recede from a sharp throb to a dull ache.
- Substantial Resolution (90-180 minutes): By the end of the third hour, for most cases of moderate dehydration, the body has had sufficient time to absorb and integrate enough fluid to largely resolve the primary physiological triggers of the headache. Brain volume has been largely restored, electrolyte balance is significantly improved, and vascular irritation has subsided. While complete, deep cellular rehydration and full electrolyte normalization might take longer, the symptomatic relief is profound.
Important Caveats:
- Severity of Dehydration: This timeframe applies best to moderate dehydration. Severe dehydration, often accompanied by confusion, lethargy, or inability to keep fluids down, requires immediate medical attention and may necessitate intravenous fluids.
- Individual Variability: Metabolic rate, kidney function, body composition, and initial hydration status all play a role. Some individuals may experience relief sooner, others slightly later.
- Type of Fluid: As we’ll discuss, the type of fluid consumed significantly impacts absorption efficiency. Plain water is good, but electrolyte-rich solutions are often superior for rapid recovery.
- Accompanying Factors: If the headache is compounded by severe sleep deprivation, extreme heat stress, or other underlying conditions, the relief might be less immediate or complete.
The "3-Hour Fix" is not a magic bullet, but rather a realistic expectation based on the body’s efficient physiological responses to targeted rehydration. It’s about empowering yourself with knowledge to leverage these natural mechanisms for rapid recovery.
Part 4: The Arsenal of Relief – Strategic Rehydration
Armed with the knowledge of why dehydration causes headaches and how quickly the body can respond, the next step is to understand what to drink and how to drink it for optimal and rapid relief. This isn’t just about guzzling water; it’s about smart rehydration.
What to Drink: The Right Fluids for the Job
-
Oral Rehydration Solutions (ORS): The Gold Standard
- Why: ORS, like those endorsed by the WHO, are scientifically formulated to contain the precise balance of electrolytes (sodium, potassium, chloride) and glucose. Glucose facilitates the co-transport of sodium and water across the intestinal wall, maximizing absorption efficiency. This makes them significantly more effective than plain water for rapid rehydration, especially when electrolyte depletion is a concern (e.g., after heavy sweating, vomiting, or diarrhea).
- Examples: Pedialyte, generic ORS packets.
-
Electrolyte-Enhanced Water:
- Why: Many sports drinks offer electrolytes, but often come with excessive sugar. Look for options with lower sugar content or make your own by adding a pinch of salt and a squeeze of citrus to water. The aim is to provide enough electrolytes to aid absorption without overwhelming the system with sugar.
- Examples: Smartwater, coconut water (natural electrolytes, but often low in sodium; may need supplementation), diluted fruit juice (provides some sugar and potassium, but dilute to avoid hyperosmolarity).
-
Plain Water:
- Why: The fundamental requirement. If nothing else is available, plain water is always better than nothing. However, for significant dehydration, especially with headache, plain water alone can sometimes dilute existing electrolytes further, temporarily exacerbating the problem or slowing recovery. It’s effective for mild dehydration or as a complement to electrolyte intake.
- Tip: If using plain water, consider adding a very small amount of salt (1/4 teaspoon per liter) and a squeeze of lemon or lime for a simple, homemade electrolyte booster.
What to Avoid (or Limit):
- Sugary Drinks: Sodas, fruit punches, and highly sweetened sports drinks can be hypertonic (higher concentration than blood). This can draw water into the intestine from the bloodstream, temporarily worsening dehydration and potentially causing nausea or diarrhea.
- Alcohol: A diuretic that will exacerbate dehydration.
- Excessive Caffeine: Can have a mild diuretic effect and may contribute to a different type of headache when consumed in excess or withdrawn from. While a small amount might be okay if accustomed to it, it’s not a rehydration strategy.
How to Drink: The Art of Strategic Sips
- Sip, Don’t Chug: Guzzling large volumes of fluid quickly can overwhelm the stomach, leading to nausea, vomiting, or simply inefficient absorption. It can also cause a rapid drop in blood sodium concentration (hyponatremia) in rare, extreme cases. Instead, take small, frequent sips (e.g., 100-200ml every 15-20 minutes). This allows for steady absorption and minimizes discomfort.
- Listen to Your Body: Drink until your thirst is quenched, but continue to sip fluids for the next hour or two to ensure sustained rehydration.
- Temperature Matters: Cool (but not ice-cold) fluids are generally more palatable and absorbed more quickly than very hot or very cold beverages.
- Monitor Urine Color: A simple, yet effective indicator. Pale yellow urine indicates good hydration; dark yellow or amber suggests continued dehydration. Aim for consistently pale yellow.
Beyond Fluids: Complementary Measures
- Rest: Lie down in a cool, quiet, dark room. Physical exertion will only increase fluid loss through sweat and delay recovery. Sensory input can exacerbate the headache.
- Cool Compress: A cool, damp cloth on the forehead or neck can provide symptomatic relief by constricting blood vessels and soothing irritated nerves.
- Light Snack: If you can tolerate it, a small, bland snack (e.g., crackers, banana) can help stabilize blood sugar and provide some additional electrolytes.
- Over-the-Counter Pain Relievers (Use with Caution): While not addressing the root cause, NSAIDs like ibuprofen or acetaminophen can provide temporary symptomatic relief if tolerated and after rehydration has begun. They should not be seen as a substitute for fluids.
By combining the right fluids with the right drinking strategy and supportive measures, you create an optimal environment for your body to execute the "3-Hour Fix."
Part 5: The Journey to Equilibrium – A Hypothetical Case Study
To truly illustrate the "3-Hour Fix," let’s follow Alex, a 32-year-old software engineer, through a typical scenario. Alex spent a particularly grueling day coding, fueled by coffee, skipping lunch, and forgetting his water bottle. The evening found him with a dull, persistent ache behind his eyes, a feeling of cotton in his mouth, and a profound weariness. His urine was dark, and the thought of another line of code made him wince. This was a classic moderate dehydration headache.
Hour 0: The Onset and Intervention
Alex recognizes the signs. He resists the urge to grab a sugary soda or an immediate painkiller. Instead, he reaches for a pre-mixed oral rehydration solution (ORS) he keeps in his pantry. He pours a glass, notes its cool temperature, and takes his first slow, deliberate sips. He also dims the lights, puts on some quiet music, and settles onto the couch.
- Physiological Response: The ORS hits his stomach. The brain’s thirst receptors, firing frantically just moments ago, register the first intake of fluid. The body’s internal alarm bells begin to quiet, albeit subtly. The immediate dry mouth sensation starts to recede.
Hour 1: Initial Relief and Systemic Engagement
Over the first hour, Alex sips approximately 500ml of ORS, taking a small sip every 10-15 minutes. He avoids gulping. He notices the headache’s intensity hasn’t vanished, but it’s softened. The sharp, pulsating edge has dulled into a more generalized pressure. He feels less parched, and a sliver of his energy begins to return.
- Physiological Response: The ORS has efficiently moved from his stomach to his small intestine, where the glucose-sodium co-transport system is working overtime. Water and electrolytes are rapidly absorbed into his bloodstream. Blood volume is beginning to normalize, and blood osmolality is slowly decreasing. This osmotic shift allows water to begin re-entering his brain cells, slightly reducing the meningeal tension. His kidneys are starting to respond, reducing ADH output.
Hour 2: Significant Improvement and Cellular Repair
Alex continues his methodical sipping, consuming another 300-400ml of ORS. By now, the headache is noticeably diminished. He can open his eyes without wincing, and the nausea has completely subsided. He even feels comfortable enough to get up for a light, bland snack – a banana for potassium, and some plain crackers.
- Physiological Response: A substantial volume of fluid has now been distributed throughout his body. His brain cells are significantly rehydrated, easing the mechanical stress. Electrolyte concentrations are nearing optimal levels, allowing his neurons to function more smoothly. The cerebral blood vessels are less irritated, contributing to the reduction in pulsatile pain. The systemic feeling of fatigue is lifting as his body’s core functions stabilize. His urine, while still a bit dark, is showing signs of lightening.
Hour 3: Near Resolution and Restoration of Equilibrium
As the three-hour mark approaches, Alex finishes his final glass of ORS, bringing his total intake to roughly 1 liter. The headache is all but gone, replaced by a lingering sense of mild pressure, if anything. He feels alert, refreshed, and capable of resuming normal, light activities. His urine is a healthy pale yellow.
- Physiological Response: His body has largely restored its fluid and electrolyte balance. The brain has re-expanded to its normal volume, relieving the meningeal tension. Neuronal function is optimized, and vascular irritation is minimal. While complete, deep cellular rehydration will continue over the next several hours, the primary symptomatic drivers of the headache have been effectively neutralized. Alex has successfully executed the "3-Hour Fix."
This hypothetical journey demonstrates that for moderate dehydration, prompt and strategic rehydration isn’t just a palliative measure; it’s a direct intervention that allows the body’s intrinsic homeostatic mechanisms to swiftly correct the underlying physiological imbalances.
Part 6: Beyond the Fix – Prevention and Long-Term Wellness
While the "3-Hour Fix" offers powerful relief, the ultimate goal is prevention. A knowledgeable audience understands that consistent, proactive hydration is not merely about avoiding headaches; it’s fundamental to overall health, cognitive function, energy levels, and metabolic efficiency.
Proactive Hydration Strategies:
- Consistent Intake: Don’t wait for thirst. Thirst is often a sign that you’re already mildly dehydrated. Aim to sip water consistently throughout the day.
- Hydration Schedule: For those who struggle, setting reminders or using a water tracking app can be incredibly effective.
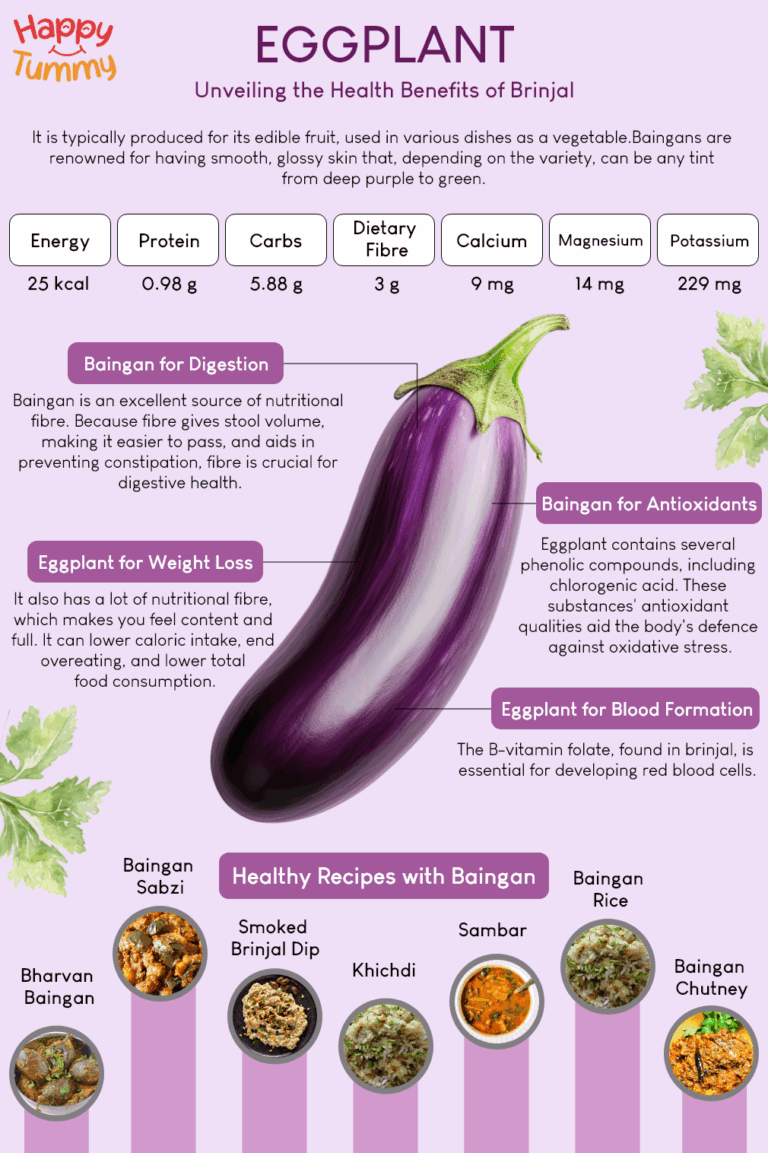
- Water-Rich Foods: Incorporate fruits and vegetables with high water content (cucumbers, watermelon, oranges, leafy greens) into your diet. These also provide essential vitamins and minerals.
- Before, During, and After Exercise: Pre-hydrate, sip fluids frequently during activity, and replenish electrolytes afterward, especially during intense or prolonged workouts.
- Awareness of Environment: Increase fluid intake when in hot climates, at high altitudes, or in dry environments.
- Limit Diuretics: Moderate alcohol and caffeine intake, and be mindful of their dehydrating effects. If consuming them, compensate with extra water.
- Monitor Urine Color: Make it a habit to check your urine color regularly. It’s a simple, non-invasive indicator of your hydration status.
When to Seek Medical Attention:
While most dehydration headaches are manageable at home, certain symptoms warrant professional medical advice:
- Severe Symptoms: Unrelenting headache, confusion, dizziness that prevents standing, extreme lethargy, or rapid heart rate.
- Inability to Keep Fluids Down: Persistent vomiting that prevents rehydration.
- Symptoms Worsen or Don’t Improve: If the headache or other symptoms persist or worsen despite consistent rehydration efforts over several hours.
- Pre-existing Conditions: Individuals with heart conditions, kidney disease, or diabetes need to be particularly cautious and consult their doctor regarding hydration strategies.
- Signs of Severe Dehydration: Sunken eyes, lack of tears, very dry mouth, decreased urination, or fever accompanied by stiff neck.
Conclusion: Empowering the Hydrated Life
The dehydration headache, while common, doesn’t have to be a prolonged ordeal. By understanding its physiological underpinnings and embracing a strategic approach to rehydration, we unlock the body’s remarkable capacity for rapid self-correction. The "3-Hour Fix" is not a myth; it’s a testament to the efficient mechanisms our bodies employ when given the right tools at the right time.
This journey from discomfort to equilibrium is a powerful narrative of self-care and informed action. It transforms the experience from passive suffering to an active partnership with our own physiology. Beyond the immediate relief, adopting a proactive approach to hydration is a profound investment in overall well-being, enhancing everything from cognitive function and physical performance to mood and metabolic health.
So, the next time that tell-tale throb begins, remember the "3-Hour Fix." Reach for that electrolyte solution, sip deliberately, rest strategically, and witness your body’s impressive ability to restore its delicate balance. Embrace the power of knowledge, and step confidently towards a consistently hydrated, headache-free existence. Your brain, and indeed your entire body, will thank you for it.