Myth vs. Medicine: Separating Fact from Fiction About Gout Causes
For centuries, gout has been a disease shrouded in misconception, often dismissed as a self-inflicted ailment of the gluttonous and the idle rich. Its historical moniker, "the disease of kings," conjures images of corpulent aristocrats feasting on platters of game and washing it down with copious amounts of port. This enduring caricature, while perhaps containing a kernel of truth about certain dietary triggers, has done a profound disservice to the millions who suffer from its excruciating pain, perpetuating stigma and obscuring the complex medical realities of its causation. In the modern era, as scientific understanding deepens, it’s high time to dismantle these myths and illuminate the intricate interplay of genetics, physiology, and lifestyle that truly underpins this ancient affliction.
This article aims to embark on a journey from folklore to molecular biology, dissecting the myriad factors that lead to gout, separating the sensationalized from the scientifically validated, and ultimately, empowering a knowledgeable audience with a comprehensive understanding of this often-misunderstood condition. We will delve into the core medical mechanisms, explore the predominant risk factors, and directly confront the persistent myths that continue to cloud public perception.
The Medical Heart of the Matter: Uric Acid and Hyperuricemia
At the very core of gout lies a metabolic imbalance involving uric acid. To truly grasp gout, one must first understand this fundamental player. Uric acid is a natural waste product generated by the body during the breakdown of purines, compounds found abundantly in our own cells (DNA, RNA) and in many foods. Normally, uric acid dissolves in the blood, passes through the kidneys, and is excreted in urine.
The problem arises when there’s an excess of uric acid in the blood, a condition known as hyperuricemia. It’s crucial to understand that hyperuricemia alone does not equate to gout. Many people can have elevated uric acid levels without ever experiencing a gout attack. However, hyperuricemia is the prerequisite for gout. When uric acid levels become sufficiently high, or when other factors create an opportune environment, the uric acid can crystallize into needle-like formations of monosodium urate (MSU).
These microscopic MSU crystals are the true culprits behind the agony of a gout attack. They tend to precipitate in cooler areas of the body, most notably the joints, especially the metatarsophalangeal joint at the base of the big toe (podagra). Once these crystals form, the body’s immune system recognizes them as foreign invaders, triggering a ferocious inflammatory response. This acute inflammation is what causes the characteristic symptoms of gout: sudden, excruciating pain, swelling, redness, and intense tenderness in the affected joint, often so severe that even the touch of a bedsheet is unbearable.
The journey of understanding gout, therefore, begins with a deep dive into why hyperuricemia occurs and why, in some individuals, it escalates into the painful manifestation of gout. This involves a delicate balance between uric acid production and excretion, a balance influenced by a complex web of genetic predispositions, physiological processes, and environmental factors.
The Unseen Architects: Genetic Predisposition
Perhaps the most significant and often overlooked factor in gout causation is genetics. While lifestyle choices certainly play a role, they often act as triggers or accelerators for an underlying genetic susceptibility. Gout, far from being solely a consequence of overindulgence, has a strong hereditary component. If a close family member has gout, your risk is significantly elevated, regardless of your diet or drinking habits.
Scientific research, particularly through genome-wide association studies (GWAS), has identified numerous genes that play a crucial role in regulating uric acid levels. These genes primarily influence two key processes: the production of uric acid and, more significantly, its excretion by the kidneys and intestines.
One of the most well-studied genes is SLC2A9 (Solute Carrier Family 2 Member 9), which encodes a urate transporter protein called GLUT9. This protein is critical for reabsorbing uric acid in the kidneys and, to a lesser extent, in the intestines. Variations (polymorphisms) in the SLC2A9 gene can lead to reduced uric acid excretion, causing levels to build up in the blood. Individuals with certain variants of this gene are at a substantially higher risk of developing hyperuricemia and gout.
Another important gene is ABCG2 (ATP Binding Cassette Subfamily G Member 2), which encodes a transporter protein that actively pumps uric acid out of the body, particularly in the intestines and kidneys. Certain variations in ABCG2 can impair its function, again leading to diminished uric acid excretion and increased serum uric acid levels.
Beyond these two prominent examples, many other genes are implicated, often working in concert, making gout a polygenic disease. This genetic blueprint dictates an individual’s inherent capacity to manage uric acid. For someone with a strong genetic predisposition to impaired uric acid excretion, even a moderately challenging diet or lifestyle can push their uric acid levels into the danger zone, whereas someone without such a predisposition might tolerate far greater dietary indiscretions without ever developing gout.
Understanding the genetic component is vital because it shifts the narrative from one of personal blame to one of biological vulnerability. It underscores that while lifestyle modifications are important for managing gout, they often work within the confines of an individual’s genetic predisposition. It also explains why some people who appear to lead healthy lives still develop gout, while others who seemingly defy all health recommendations remain gout-free.
The Kidney’s Crucial Role: Excretion and Impairment
While genetics lays the foundation, the kidneys are the primary workhorses in the body’s uric acid management system. Approximately two-thirds of the uric acid produced daily is excreted by the kidneys, with the remaining one-third handled by the intestines. Any impairment in kidney function or in the specific mechanisms by which kidneys handle uric acid can lead directly to hyperuricemia and, subsequently, gout.
The kidneys don’t just filter uric acid; they actively reabsorb some of it back into the bloodstream to maintain a healthy balance. It’s a complex process involving various transporters (like those encoded by SLC2A9 and ABCG2, as mentioned above). Problems can arise from:
- Reduced Glomerular Filtration Rate (GFR): This is the overall measure of kidney function. Conditions like chronic kidney disease (CKD), regardless of its underlying cause (diabetes, hypertension, autoimmune diseases), will inevitably lead to decreased uric acid excretion. As CKD progresses, the kidneys become less efficient at filtering waste products, including uric acid, causing it to accumulate in the blood.
- Impaired Tubular Secretion: Even with a normal GFR, specific transporters in the kidney tubules can malfunction. Some genetic variations primarily affect these transporters, leading to what’s called "underexcretion" of uric acid.
- Medications: A number of commonly prescribed medications can interfere with uric acid excretion, making them significant risk factors for gout.
- Diuretics (water pills): Thiazide diuretics (e.g., hydrochlorothiazide) and loop diuretics (e.g., furosemide) are frequently used to treat high blood pressure and heart failure. They increase water and salt excretion, but they also reduce the kidney’s ability to excrete uric acid, often leading to dose-dependent hyperuricemia.
- Low-dose Aspirin: While high doses of aspirin promote uric acid excretion, low doses (often used for cardiovascular protection) paradoxically inhibit it, increasing uric acid levels.
- Immunosuppressants: Drugs like cyclosporine, used in organ transplant recipients or for autoimmune diseases, can impair kidney function and directly interfere with uric acid handling.
- Certain cancer chemotherapy drugs: These can cause rapid cell turnover, leading to a surge in purine breakdown and, consequently, uric acid production (tumor lysis syndrome), which can overwhelm the kidneys.
The intimate link between kidney health and gout underscores the systemic nature of the disease. Gout is not merely a joint problem; it’s a metabolic disorder deeply intertwined with renal physiology. Furthermore, gout itself, particularly chronic or poorly managed gout, can contribute to kidney stone formation (urate nephrolithiasis) and potentially worsen kidney function over time, creating a vicious cycle.
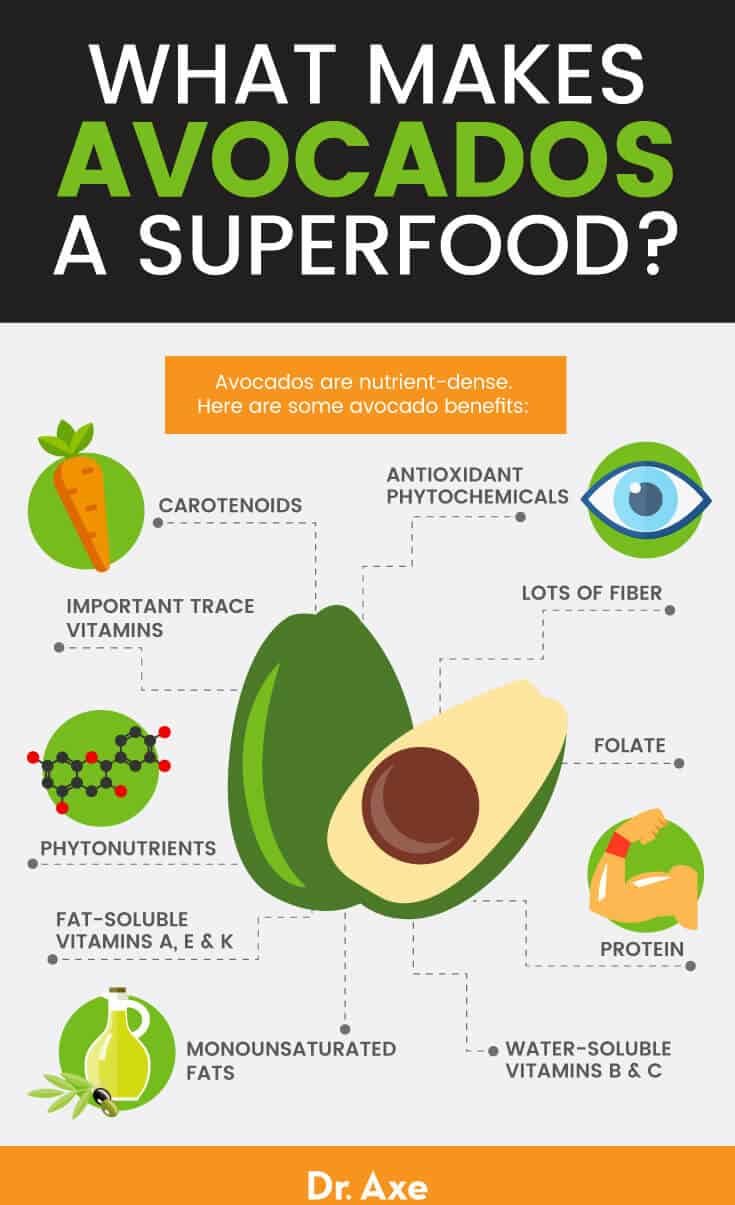
Dietary Influences: Nuance Over Blame
This is perhaps the most myth-laden aspect of gout. For too long, diet has been cast as the sole villain, unfairly blaming individuals for a condition rooted in deeper biological predispositions. While diet certainly plays a role, it’s rarely the only cause and often acts as a trigger rather than the fundamental underlying problem. The key is nuance – understanding which dietary components matter most, and how they interact with an individual’s genetic and physiological makeup.
-
High-Purine Foods:
- Organ Meats: Liver, kidney, sweetbreads are exceptionally high in purines and should be consumed sparingly, if at all, by individuals prone to gout.
- Red Meat: Beef, pork, lamb contain moderate to high levels of purines. While not as potent as organ meats, excessive consumption can contribute to hyperuricemia, especially in genetically susceptible individuals.
- Certain Seafood: Shellfish (shrimp, crab, lobster, scallops) and some fish (anchovies, sardines, herring, mackerel) are notoriously high in purines.
- The Nuance: It’s important to differentiate between dietary purines and the body’s total uric acid load. Only a fraction of the body’s daily uric acid comes directly from dietary purines. Most is produced internally. Therefore, while restricting high-purine foods can help lower uric acid levels by a small to moderate amount (typically 1-2 mg/dL), it’s often insufficient to manage severe hyperuricemia on its own, especially if genetics or kidney function are significant factors. Furthermore, not all purine-rich foods are equally problematic. Plant-based purine sources (like lentils, beans, mushrooms, spinach, asparagus) have not been consistently linked to an increased risk of gout and are generally considered healthy. The demonization of all purine-rich foods is an oversimplification.
-
Fructose-Sweetened Beverages:
- This is a relatively more recent, yet increasingly recognized, dietary culprit. High-fructose corn syrup (HFCS) and sucrose (table sugar, which is half fructose) are abundant in soft drinks, fruit juices, and many processed foods. Fructose metabolism uniquely stimulates the production of uric acid and simultaneously inhibits its excretion by the kidneys.
- Studies have shown a strong correlation between regular consumption of sugar-sweetened beverages and an increased risk of gout, even independent of other dietary factors. This effect is often more pronounced than that of purine-rich foods. This highlights that "diet" isn’t just about purines; the type of sugar matters significantly.
-
Alcohol Consumption:
- Alcohol is a well-established trigger for gout attacks and a contributor to chronic hyperuricemia, but not all types of alcohol are equally problematic.
- Beer: Is particularly potent because it contains both alcohol (which increases uric acid production and decreases excretion) and a significant amount of purines from yeast.
- Spirits (Hard Liquor): Also increase uric acid levels, primarily through the effects of ethanol on uric acid metabolism.
- Wine: Appears to have a less pronounced effect than beer or spirits, with some studies even suggesting moderate wine consumption may not increase gout risk significantly. However, excessive consumption of any alcohol is detrimental for gout sufferers.
- The Mechanism: Alcohol metabolism produces lactate, which competes with uric acid for excretion by the kidneys. Alcohol also dehydrates the body and increases purine breakdown, contributing to higher uric acid levels.
-
Dehydration:
- While not a direct "cause" of chronic hyperuricemia, acute dehydration can trigger a gout attack. When the body is dehydrated, uric acid in the blood becomes more concentrated, increasing the likelihood of crystal formation. Maintaining adequate hydration is crucial for preventing attacks and supporting kidney function.
In summary, diet plays a supporting role, often acting as a catalyst for individuals already genetically predisposed or those with compromised kidney function. It’s less about the occasional indulgence and more about chronic patterns of consumption, particularly of high-fructose beverages, excessive alcohol, and certain purine-rich foods. The "rich man’s diet" myth, therefore, needs to be updated to the "modern processed food and sugary drink diet" myth, which affects people across all socioeconomic strata.
The Modern Scourge: Obesity and Metabolic Syndrome
The rise in global obesity rates and the prevalence of metabolic syndrome (a cluster of conditions including abdominal obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels) have coincided with an increasing incidence of gout. This is no mere coincidence; the links are robust and multifaceted.
-
Obesity: Individuals who are overweight or obese tend to have higher serum uric acid levels. Adipose tissue (fat cells), particularly visceral fat around the organs, is metabolically active. It produces inflammatory cytokines and hormones that can directly increase uric acid production and impair its renal excretion. Furthermore, obesity is often associated with insulin resistance.
-
Insulin Resistance: A hallmark of metabolic syndrome and type 2 diabetes, insulin resistance means the body’s cells don’t respond effectively to insulin. To compensate, the pancreas produces more insulin (hyperinsulinemia). High insulin levels have been shown to reduce the kidney’s ability to excrete uric acid, leading to its accumulation in the blood. This creates a direct link between the metabolic derangements of insulin resistance and hyperuricemia.
-
Inflammation: Obesity and metabolic syndrome are characterized by a state of chronic low-grade inflammation throughout the body. While the MSU crystals directly trigger the acute inflammatory response in gout, this underlying systemic inflammation may prime the body for more severe or frequent attacks, or contribute to the overall disease burden.
-
Comorbidities: Obesity and metabolic syndrome are strongly linked to other conditions that independently increase gout risk, such as hypertension (high blood pressure) and chronic kidney disease. Many medications for these conditions (e.g., diuretics for hypertension) further exacerbate hyperuricemia.
Therefore, gout is increasingly recognized as a component of the broader metabolic syndrome spectrum. It’s a manifestation of a systemic metabolic dysfunction, not just an isolated joint problem. Addressing obesity and metabolic syndrome through lifestyle interventions (dietary changes, exercise) can be highly effective in reducing uric acid levels and managing gout, reinforcing the idea that overall health is intrinsically linked to gout risk.
Other Contributing Factors and Comorbidities
Beyond the primary drivers, several other factors can influence gout risk and severity:
-
Lead Exposure: Chronic lead exposure, even at levels not typically associated with overt lead poisoning, can impair kidney function and reduce uric acid excretion, increasing the risk of "saturnine gout." This was historically observed in populations with occupational exposure to lead or those who consumed "moonshine" distilled in lead-containing stills.
-
Psoriasis and Other Proliferative Disorders: Conditions characterized by rapid cell turnover, such as psoriasis or certain cancers (e.g., lymphomas, leukemias), lead to an increased breakdown of cellular purines, resulting in higher uric acid production.
-
Hypothyroidism: An underactive thyroid gland has been associated with elevated uric acid levels and an increased risk of gout, though the exact mechanism is still being researched.
-
Trauma or Surgery: Physical stress, trauma, or surgery can sometimes trigger an acute gout attack. The mechanisms are complex but may involve localized inflammation, changes in blood flow, or mild dehydration during recovery.
-
Gender and Age: Gout is significantly more common in men than in premenopausal women. Estrogen appears to have a protective effect, enhancing uric acid excretion. After menopause, women’s risk of gout rises and approaches that of men. The incidence of gout also increases with age in both genders.
These myriad factors underscore the complexity of gout causation. It’s rarely a single, isolated issue but rather a convergence of genetic predispositions, physiological vulnerabilities, and environmental influences.
Beyond the Toe: Common Myths Debunked
Now that we’ve delved into the medical realities, let’s directly confront some of the most pervasive myths about gout:
Myth 1: Gout is only caused by diet and overindulgence.
Fact: While diet and lifestyle choices (alcohol, sugary drinks, high-purine foods) can certainly trigger attacks and contribute to hyperuricemia, they are rarely the sole cause. The vast majority of gout cases have a strong genetic component that impairs the body’s ability to excrete uric acid. Many individuals with a pristine diet can still develop gout due to their genetic predisposition or underlying kidney issues, while others with less-than-ideal diets may never experience it. Blaming diet alone is an oversimplification that ignores the complex interplay of factors.
Myth 2: It’s a disease of the past or only affects the wealthy.
Fact: Gout is far from a historical relic. In fact, its prevalence has been steadily increasing globally, particularly in developed nations. This rise is attributed to factors like the aging population, increasing rates of obesity and metabolic syndrome, and the widespread consumption of high-fructose corn syrup. While historical records link it to affluence, modern gout affects people across all socioeconomic strata. The "disease of kings" is now a disease of modernity, impacting a diverse demographic.
Myth 3: Gout only affects the big toe.
Fact: While the big toe (podagra) is the most common site for the first gout attack (affecting about 50-70% of initial attacks), gout can affect any joint in the body. Other frequently affected joints include the ankles, knees, wrists, fingers, and elbows. In chronic, untreated gout, these uric acid crystals can also accumulate under the skin to form visible, chalky lumps called tophi, which can be disfiguring and cause joint damage, even appearing in ears or other soft tissues.
Myth 4: "Just drink water" or "eat cherries" is a cure.
Fact: Adequate hydration is crucial for helping the kidneys excrete uric acid and can help prevent attacks, but it is not a standalone "cure" for chronic hyperuricemia or established gout. Similarly, cherries and cherry extract contain anthocyanins, which have anti-inflammatory and antioxidant properties and may slightly lower uric acid levels. Some studies suggest they can reduce the risk of gout attacks. However, they are a complementary therapy, not a substitute for prescribed medication (like allopurinol or febuxostat for long-term management, or NSAIDs/colchicine for acute attacks) when needed, especially in severe or recurrent cases. Relying solely on these natural remedies can lead to uncontrolled disease progression and long-term joint damage.
Myth 5: Gout is "just arthritis" and nothing serious.
Fact: Gout is far more than "just" a painful joint condition. It is a systemic inflammatory disease and a marker of underlying metabolic dysfunction. Chronic, uncontrolled gout can lead to irreversible joint damage, severe pain, functional disability, and the formation of tophi. Moreover, gout is strongly associated with a range of serious comorbidities, including chronic kidney disease, hypertension, cardiovascular disease (heart attacks and strokes), diabetes, and metabolic syndrome. Ignoring gout or failing to manage it effectively can have significant long-term health consequences beyond the joints, increasing morbidity and mortality.
The Human Cost: Understanding for Empathy and Management
The persistent myths surrounding gout have a real human cost. They fuel stigma, leading many sufferers to feel shame or guilt, and sometimes even discouraging them from seeking timely and consistent medical care. This can result in delayed diagnosis, undertreatment, and ultimately, preventable suffering and long-term complications.
Understanding the true causes of gout – the intricate dance between genetics, kidney function, and modifiable lifestyle factors – shifts the narrative from one of blame to one of biological reality and empowers both patients and healthcare providers. For patients, it fosters a sense of agency, allowing them to focus on effective management strategies without the burden of unwarranted guilt. For clinicians, it facilitates a more holistic approach, addressing not only the acute pain but also the underlying metabolic derangements and associated comorbidities.
The journey from myth to medicine reveals gout to be a sophisticated, multifaceted disease, deeply intertwined with our genetic heritage and modern lifestyle. It is a condition that demands respect, comprehensive understanding, and a commitment to evidence-based management.
Conclusion
The story of gout, from ancient lore to modern molecular science, is a compelling narrative of evolving understanding. What was once attributed solely to the excesses of royalty is now recognized as a complex metabolic disorder driven by an intricate interplay of genetic predisposition, renal physiology, and a spectrum of environmental and lifestyle factors. The idea that gout is merely a punishment for gluttony is not only inaccurate but also harmful, perpetuating stigma and hindering effective management.
We have seen that hyperuricemia, the precursor to gout, arises predominantly from the body’s impaired ability to excrete uric acid, largely dictated by our genetic makeup. The kidneys play a central role, and their function can be compromised by genetic variants, underlying diseases like chronic kidney disease, and even commonly prescribed medications. While dietary choices – particularly the consumption of high-fructose beverages, excessive alcohol, and certain purine-rich foods – can certainly act as triggers and contribute to the uric acid load, they rarely operate in isolation. The growing epidemic of obesity and metabolic syndrome further intertwines gout with broader systemic health issues.
Separating fact from fiction about gout causes is not merely an academic exercise; it is a critical step towards compassionate care, informed decision-making, and improved public health outcomes. By shedding the outdated stereotypes and embracing the scientific realities, we can ensure that individuals living with gout receive the understanding, support, and effective medical interventions they deserve. The future of gout management lies in this nuanced, evidence-based approach, fostering a world where the agony of gout is no longer exacerbated by the sting of misconception.