The Antibiotic Conflict: Why Taking Zinc at the Wrong Time Makes Your Medicine Useless
In the grand theatre of human health, where microscopic battles are waged daily, few interventions have played as pivotal a role as antibiotics. These molecular marvels, born from the accidental discovery of penicillin, represent one of medicine’s greatest triumphs, transforming once-lethal infections into treatable ailments. They are the frontline defenders, the silent guardians against bacterial onslaughts that threaten to overwhelm our delicate biological systems. Yet, even these powerful agents are not invincible, and their efficacy can be undermined by a surprisingly common and seemingly innocuous habit: the mistimed intake of certain dietary supplements, particularly zinc.
This is the story of a silent conflict, a chemical tango occurring within the very confines of our digestive tracts, where a beneficial nutrient unwittingly sabotages the life-saving mission of an antibiotic. It’s a narrative of absorption, molecular interference, and the profound consequences that arise from a lack of understanding about the intricate pharmacology of our bodies. For the knowledgeable reader, this isn’t just a cautionary tale; it’s an exploration into the nuanced world of drug-nutrient interactions, pharmacokinetics, and the escalating crisis of antibiotic resistance – a crisis quietly fueled by seemingly minor oversights.
The Unseen Battlefield: Pharmacokinetics and the Gut
Before delving into the specifics of the zinc-antibiotic conflict, it’s essential to appreciate the complex journey a drug undertakes from the moment it enters our body until it exerts its therapeutic effect. This journey, known as pharmacokinetics, encompasses four key stages: Absorption, Distribution, Metabolism, and Excretion (ADME). For an antibiotic to work, it must first be adequately absorbed from the gastrointestinal (GI) tract into the bloodstream. This initial step is critical; if the drug cannot pass from the gut lumen into systemic circulation, it cannot reach its target site of infection.
The human GI tract is a marvel of biological engineering, designed to selectively absorb nutrients while simultaneously acting as a barrier against harmful substances. It’s a highly regulated environment, with specific transport proteins, pH gradients, and enzymatic activities all playing a role in determining a drug’s bioavailability – the fraction of an administered dose that reaches the systemic circulation in an unchanged form. A drug with poor oral bioavailability is essentially ineffective, regardless of its potency in a petri dish.
Many factors can influence drug absorption: the drug’s chemical properties (solubility, molecular size, charge), the presence of food, the pH of the stomach and intestines, and critically, the presence of other substances that can interact with the drug. It is within this dynamic and often turbulent environment that our story’s conflict unfolds.
The Protagonist: Our Antibiotic Arsenal
Our focus here is on two crucial classes of antibiotics particularly vulnerable to interference from metal ions: tetracyclines and fluoroquinolones.
-
Tetracyclines (e.g., doxycycline, minocycline, tetracycline) are broad-spectrum antibiotics, meaning they are effective against a wide range of bacteria. They work by inhibiting bacterial protein synthesis, specifically binding to the 30S ribosomal subunit, thereby preventing the assembly of essential proteins that bacteria need to grow and multiply. They are prescribed for a diverse array of infections, from acne and respiratory tract infections to Lyme disease and malaria prophylaxis. Their utility makes them indispensable tools in modern medicine.
-
Fluoroquinolones (e.g., ciprofloxacin, levofloxacin, moxifloxacin) are another class of broad-spectrum antibiotics that operate by interfering with bacterial DNA replication. They target bacterial topoisomerase II (DNA gyrase) and topoisomerase IV, enzymes crucial for DNA unwinding, replication, and repair. This effectively halts bacterial growth and leads to cell death. Fluoroquinolones are often reserved for more serious infections, including urinary tract infections, pneumonia, and certain skin and soft tissue infections, due to concerns about resistance and potential side effects.
Both tetracyclines and fluoroquinolones share a common structural feature: they contain chemical groups that can readily form complexes with metal ions. This characteristic, while not a flaw in itself, becomes their Achilles’ heel when confronted by specific antagonists in the GI tract.
The Unwitting Antagonist: Zinc and the Chelation Conundrum
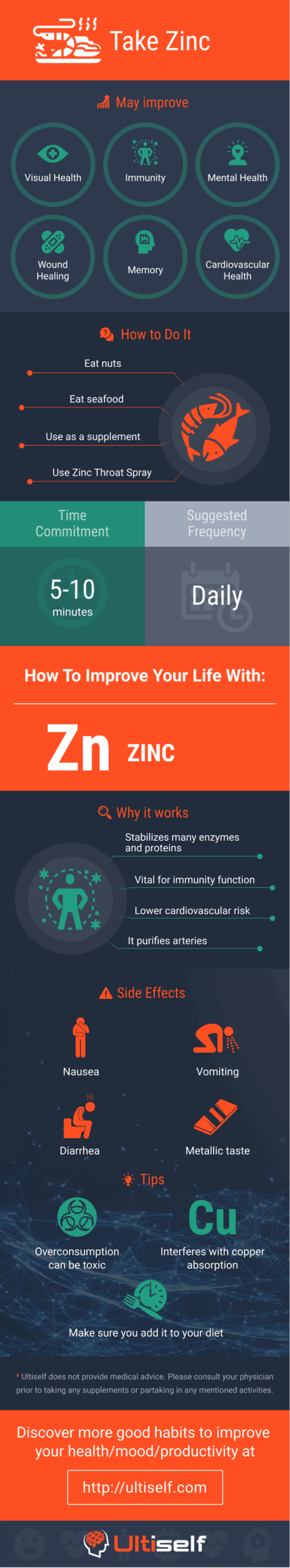
Enter zinc, a vital trace element essential for countless physiological processes in the human body. Zinc is a cofactor for over 300 enzymes, playing critical roles in immune function, wound healing, DNA synthesis, protein synthesis, and sensory functions like taste and smell. Given its widespread importance, zinc supplements are popular, especially for boosting immunity during cold and flu season or for addressing deficiencies.
The problem arises not from zinc’s inherent nature, but from its chemical behavior. Zinc, like other divalent cations (ions with a +2 charge, such as calcium, magnesium, and iron) and trivalent cations (ions with a +3 charge, such as aluminum), possesses the ability to form chelates.
Chelation is a chemical process where a metal ion forms multiple bonds with a single organic molecule, typically forming a ring-like structure. The organic molecule is called a chelating agent or ligand. Many drugs, including tetracyclines and fluoroquinolones, act as chelating agents due to their specific molecular architecture. When these antibiotics encounter metal ions like zinc in the GI tract, they don’t simply coexist; they bind together, forming a new, larger, and often poorly soluble complex.
Imagine the antibiotic molecule as a highly specific key, designed to fit into the lock of a bacterial enzyme. When it chelates with a zinc ion, it’s like attaching a bulky, unusable keychain to the key. This newly formed antibiotic-zinc chelate is fundamentally different from the unbound antibiotic molecule.
- Reduced Solubility: The chelated complex is often less soluble in the aqueous environment of the GI tract. This means it struggles to dissolve and present itself for absorption.
- Increased Molecular Size: The combined molecule is larger, making it more difficult for it to pass through the tight junctions between intestinal cells or to be recognized by specific transport proteins.
- Altered Charge and Polarity: The chelation alters the overall charge and polarity of the antibiotic, changing its ability to partition across the lipid-rich cell membranes of the intestinal lining.
The net result of this chelation is a drastic reduction in the antibiotic’s bioavailability. Instead of being absorbed into the bloodstream to fight the infection, the antibiotic-zinc complex simply passes through the digestive system and is excreted, essentially making the medicine useless.
Studies have shown that concomitant administration of zinc can reduce the absorption of tetracyclines and fluoroquinolones by as much as 50% to 90%. For example, taking ciprofloxacin with a zinc supplement can reduce its absorption by over 60%. This isn’t a minor dip in efficacy; it’s a profound undermining of the entire therapeutic strategy.
The Echoes of Failure: The Ripple Effect of Sub-therapeutic Dosing
The consequences of this drug-nutrient interaction extend far beyond a single patient’s failed treatment. When an antibiotic dose is effectively halved or more, it results in sub-therapeutic concentrations of the drug at the site of infection. This is where the true danger lies:
-
Treatment Failure: The primary and most immediate outcome is that the infection persists or worsens. The patient remains ill, suffers prolonged symptoms, and may require additional courses of antibiotics, often stronger or broader-spectrum ones, to finally eradicate the pathogen. This prolongs suffering, increases healthcare costs, and can lead to more severe complications.
-
Increased Risk of Relapse and Re-infection: Even if symptoms temporarily improve, the underlying bacterial population may not be fully eliminated. This creates a breeding ground for relapse once the antibiotic course is finished, or leaves the patient vulnerable to re-infection by the same or a different pathogen.
-
Accelerated Antibiotic Resistance: This is perhaps the most insidious and far-reaching consequence. Sub-therapeutic drug levels are a major driver of antibiotic resistance. When bacteria are exposed to concentrations of an antibiotic that are too low to kill them outright, but just enough to cause stress, they have a powerful selective pressure to evolve resistance mechanisms. The weaker, more susceptible bacteria may be eliminated, but any bacteria with even a slight genetic advantage in resisting the drug will survive and proliferate. Over time, this leads to the emergence of highly resistant strains, rendering our existing antibiotics ineffective. This is not just a theoretical concern; it’s a real-world phenomenon contributing significantly to the global antibiotic resistance crisis, a crisis that the World Health Organization has declared one of the top ten global health threats.
-
Economic Burden: Failed treatments lead to extended hospital stays, additional doctor visits, more diagnostic tests, and the need for more expensive second-line antibiotics. This imposes a significant financial burden on individuals, healthcare systems, and national economies.
Beyond Zinc: A Broader Look at Drug-Nutrient Interactions
It’s crucial to emphasize that zinc is not alone in its ability to interfere with antibiotic absorption. The same chelation phenomenon occurs with other common multivalent cations:
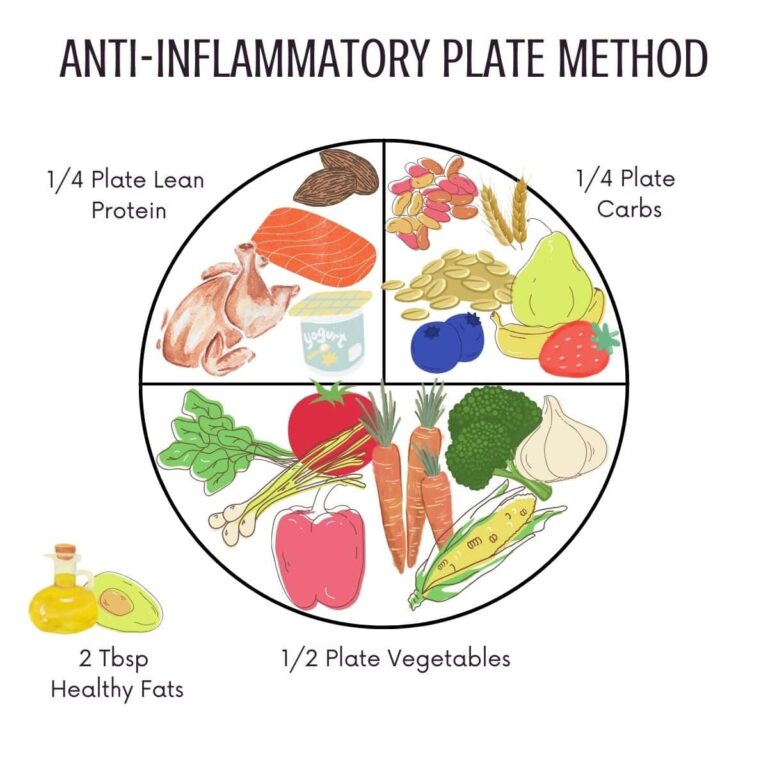
- Calcium: Found abundantly in dairy products (milk, cheese, yogurt), fortified foods, and calcium supplements. Taking tetracyclines or fluoroquinones with a glass of milk or a calcium supplement is equally detrimental.
- Magnesium: Present in green leafy vegetables, nuts, seeds, and frequently found in antacids (magnesium hydroxide) and supplements.
- Iron: Common in red meat, legumes, fortified cereals, and widely taken as an iron supplement for anemia.
- Aluminum: Often found in antacids (aluminum hydroxide) and some over-the-counter medications.
This means that a patient taking an antibiotic like doxycycline for Lyme disease, who also takes a daily multivitamin containing zinc, calcium, and iron, or who washes down their pill with milk, is effectively negating a significant portion of their treatment. The conflict isn’t just about zinc; it’s about a broader class of interactions often overlooked in the daily rush of medication administration.
The Path Forward: Navigating the Nutritional Minefield
The solution to this conflict is deceptively simple: timing. The key is to separate the intake of the antibiotic from the intake of zinc and other interacting multivalent cations.
-
The Golden Rule of Separation: Healthcare professionals typically recommend taking tetracyclines and fluoroquinolones at least 2 hours before or 4-6 hours after any products containing zinc, calcium, magnesium, iron, or aluminum. This time window allows the antibiotic to be absorbed into the bloodstream before the interfering ions arrive in significant concentrations, or ensures that the bulk of the ions have passed through the GI tract before the antibiotic is introduced.
-
Read Labels Diligently: Patients should be educated to read the labels of all their supplements, multivitamins, antacids, and even food products. Many seemingly harmless items contain these interacting minerals. For instance, some protein shakes or fortified cereals can be rich in calcium and iron.
-
Consult Your Pharmacist: Pharmacists are frontline experts in drug interactions. They can provide personalized advice on timing, potential interactions with over-the-counter medications, supplements, and even specific foods. This consultation is invaluable and often underutilized.
-
Doctor-Patient Communication: Patients must inform their prescribing doctor about all medications, supplements, and herbal remedies they are currently taking. This holistic view allows the doctor to anticipate potential conflicts and provide clear instructions.
-
Educate, Educate, Educate: The core problem is a lack of awareness. Educational campaigns targeting both the public and healthcare providers are essential. Simple visual aids, clear instructions on prescription bottles, and routine counseling can significantly reduce the incidence of these avoidable interactions.
-
Question the "Immunity Boost": While zinc is vital, the widespread practice of "mega-dosing" zinc for immunity, often without medical necessity, increases the likelihood of such interactions. A balanced diet usually provides sufficient zinc for most healthy individuals. Supplementation should be considered under medical guidance, especially when other medications are involved.
The Broader Implications: A Call to Vigilance
The story of zinc and antibiotics is a microcosm of a larger truth in pharmacology: the human body is an incredibly complex system, and introducing external substances, even beneficial ones, can have unforeseen consequences. In an age of increasing polypharmacy (the use of multiple medications) and a booming supplement industry, the potential for drug-nutrient and drug-drug interactions has never been greater.
The antibiotic resistance crisis is not a distant threat; it is here, and it is accelerating. Every instance of sub-therapeutic dosing, whether due to a mistimed supplement, poor adherence, or inadequate absorption, contributes to this global challenge. It undermines the efficacy of our most precious medical resources and pushes us closer to a post-antibiotic era where common infections could once again become deadly.
The "Antibiotic Conflict" isn’t a battle between good and evil; it’s a conflict born of ignorance. Zinc is not the enemy, nor are antibiotics inherently flawed. The true antagonist is the lack of understanding, the oversight in recognizing the intricate chemical dance that occurs within us. By fostering greater awareness, promoting diligent communication between patients and healthcare providers, and emphasizing responsible medication and supplement use, we can resolve this conflict and ensure that our powerful antibiotic arsenal remains effective for generations to come. The stakes are nothing less than the future of global health.