The Gout Attack Toolkit: What to Do When the Pain Strikes – A Narrative of Resilience and Strategy
The air hung still, heavy with an unspoken dread. For those initiated into its brutal mysteries, the subtle ache, the faint warmth in the joint, or the peculiar stiffness that precedes the storm is a familiar, terrifying harbinger. It’s the whisper before the shout, the distant rumble before the earth-shattering tremor. And then, it strikes. A gout attack – a fiery, relentless siege on a single joint, most often the big toe, transforming a mundane appendage into a throbbing, exquisitely painful sentinel of suffering.
This isn’t just pain; it’s an incapacitating, mind-altering agony that can bring the strongest among us to their knees, literally and figuratively. It’s the kind of pain that warps perception, makes sleep a distant dream, and turns the simplest act of walking into an Everest expedition. For the uninitiated, it’s a baffling, sudden descent into hell. For those who know, it’s a recurring nightmare they desperately seek to escape.
But what if we could arm ourselves? What if, instead of being passive victims, we became active combatants, equipped with a comprehensive "Gout Attack Toolkit"? This isn’t merely a collection of pills and ice packs; it’s a strategic arsenal encompassing knowledge, immediate action plans, long-term preventative measures, and crucial psychological resilience. For the knowledgeable audience, those who have felt its sting or seek to understand its depths, this narrative aims to illuminate the path from passive suffering to empowered management. We’ll delve into the science, share the strategies, and tell the stories that comprise the ultimate toolkit for navigating the treacherous waters of a gout attack.
Understanding the Enemy: The Microscopic Storm
Before we can effectively deploy our toolkit, we must first understand the adversary. Gout, often dismissed as an "old man’s disease" or a "rich man’s disease" due to its historical association with indulgent lifestyles, is, in fact, a complex metabolic disorder. It’s not a mere ache; it’s an inflammatory cascade triggered by the crystallization of monosodium urate (MSU) in the joints.
Imagine, if you will, millions of microscopic, needle-sharp crystals forming within the synovial fluid of your joint. These aren’t benign entities; they are foreign invaders. The body’s immune system, ever vigilant, detects these crystals and mounts a ferocious defense. Macrophages engulf the crystals, triggering the activation of the NLRP3 inflammasome, a molecular platform that initiates a potent inflammatory response. This leads to the production of interleukin-1 beta (IL-1β), a cytokine that acts as a clarion call, recruiting a veritable army of neutrophils and other immune cells to the site.
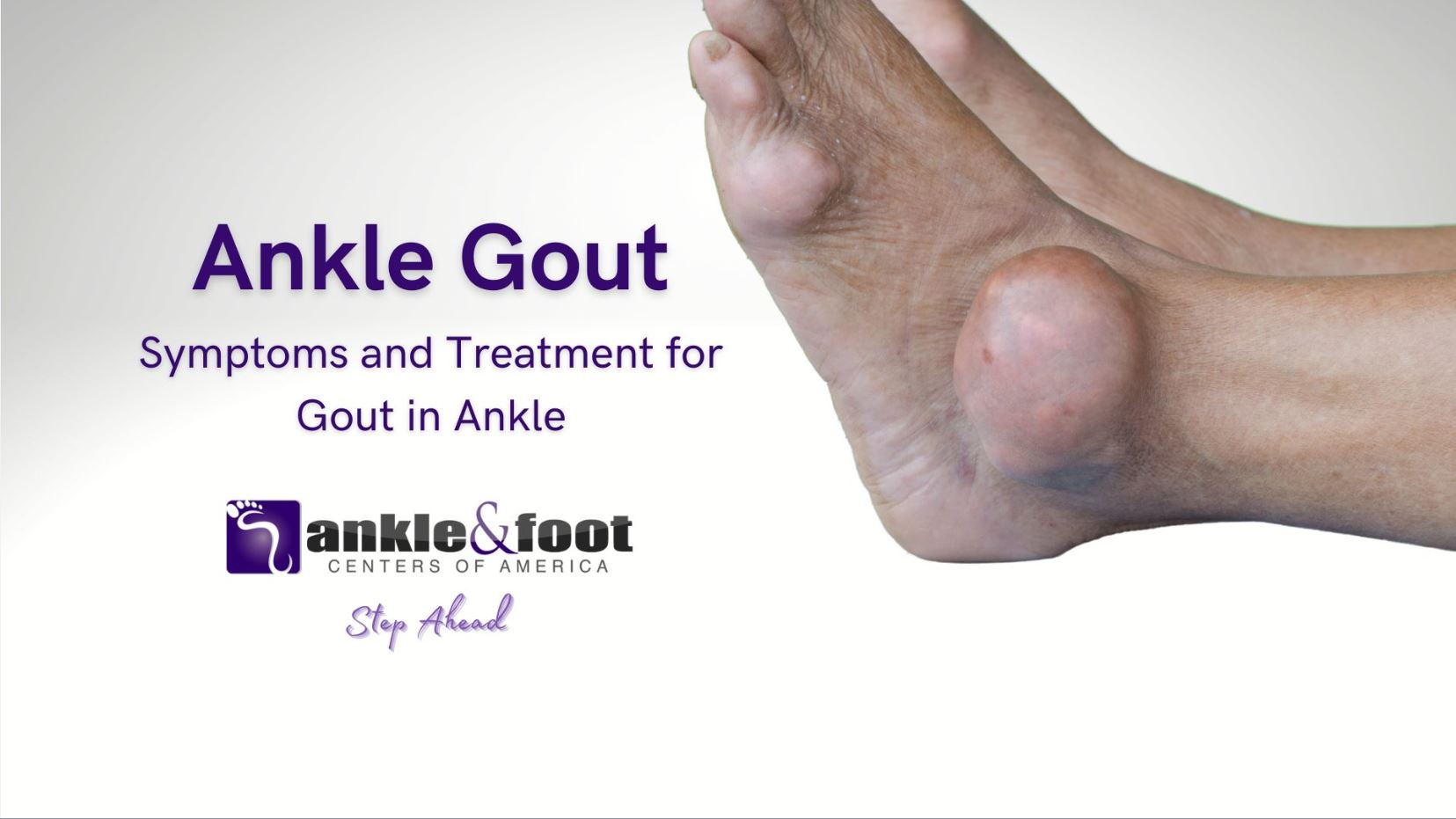
This influx of immune cells, while intended to clear the crystals, inadvertently causes immense collateral damage. The joint becomes inflamed, swollen, red, and excruciatingly tender. The very warmth we feel is the heat of this microscopic battle raging beneath our skin. Why the big toe, you might ask? Several factors contribute: gravity often makes it a cooler extremity, where uric acid is less soluble; it’s subject to microtrauma from daily activities; and its relatively poor vascularity can hinder the clearance of crystals.
Triggers, The Ticking Time Bombs: For a knowledgeable audience, recognizing triggers is paramount. They are the catalysts that push an already hyperuricemic state into an acute attack. These can include:
- Dietary excesses: High-purine foods (red meat, organ meats, shellfish), high-fructose corn syrup, sugary drinks.
- Alcohol: Especially beer and spirits, which both increase purine load and hinder uric acid excretion.
- Dehydration: Concentrates uric acid in the blood.
- Stress: Physiological stress can alter metabolic processes.
- Certain medications: Diuretics (thiazides, loop diuretics) are notorious for elevating uric acid.
- Trauma or surgery: Any physical stress on the body can precipitate an attack.
- Rapid fluctuations in uric acid levels: Ironically, initiating uric acid-lowering therapy (ULT) can sometimes trigger an attack as crystals are mobilized.
The psychological impact of these recurrent attacks cannot be overstated. The fear of the next attack, the anxiety of social situations where food and drink are present, the frustration of incapacitation, and the isolation of being unable to participate in daily life contribute to a profound mental burden. Our toolkit must address this too.
The Immediate Response Toolkit: When the Fires Ignite (The First 24-48 Hours)
When the first spark ignites, time is of the essence. The efficacy of intervention often correlates directly with how swiftly it’s applied. This is where the immediate response toolkit shines, focusing on quelling the inflammatory storm and alleviating pain.
1. The Pharmacological Arsenal: The Heavy Hitters
These are the frontline medications, potent agents designed to halt the inflammatory cascade.
-
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): The Workhorses
- Mechanism: NSAIDs inhibit cyclooxygenase (COX) enzymes, reducing the production of prostaglandins, which are key mediators of pain and inflammation. For a gout attack, they are most effective when taken at the very first sign of symptoms.
- Examples: Indomethacin is historically a favorite for gout due to its potency, but naproxen, ibuprofen, and celecoxib (a COX-2 selective inhibitor) are also highly effective.
- Dosage & Timing: High doses are typically prescribed initially, followed by a tapering regimen as symptoms improve. The critical message here is early intervention. Delaying treatment even by a few hours can significantly prolong the attack.
- Warnings & Side Effects: Knowledgeable patients understand the risks. NSAIDs can cause gastrointestinal upset, ulcers, and bleeding. They can also impact kidney function and increase cardiovascular risk, especially with long-term use or in susceptible individuals. Always discuss with a physician, especially if you have pre-existing conditions like kidney disease, heart disease, or a history of GI bleeding.
- Narrative Element: The Indomethacin Story. "I remember my first severe attack. My doctor, a gruff but brilliant man, simply handed me a script for Indomethacin and said, ‘Take it the moment you feel anything, even a tingle.’ I was skeptical. But the next time, when that familiar warmth began in my big toe, I swallowed the pill. Within hours, the relentless march of pain slowed, then retreated. It wasn’t a magic wand, but it was a shield, buying me precious time and significantly blunting the attack’s full force."
-
Colchicine: The Ancient Warrior, Modernized
- Mechanism: Colchicine is unique. It interferes with microtubule formation, thereby inhibiting neutrophil migration and activity, and also reduces the activation of the NLRP3 inflammasome and IL-1β production. It doesn’t lower uric acid; it specifically targets the inflammatory process of gout.
- Dosage & Timing: Historically, high-dose colchicine was used, leading to severe gastrointestinal side effects. Modern guidelines advocate for a low-dose regimen: 1.2 mg at the first sign of an attack, followed by 0.6 mg an hour later, and then 0.6 mg once or twice daily until the attack subsides. This low-dose regimen is significantly better tolerated. Like NSAIDs, its efficacy is dramatically reduced if not initiated within the first 12-24 hours of an attack.
- Side Effects: While improved with low-dose, GI distress (nausea, vomiting, diarrhea) remains the most common side effect. It also has drug interactions and should be used with caution in patients with kidney or liver impairment.
- Narrative Element: The Colchicine Window. "My friend, a meticulous planner, had his colchicine prescription filled and waiting. One evening, after a particularly stressful week, he felt the tell-tale twinge. Without hesitation, he took the first dose. By morning, the attack was a mere shadow of what it could have been. He called it ‘hitting the window’ – catching the attack before it could fully blossom, a testament to preparedness and swift action."
-
Corticosteroids: The Fire Extinguishers
- Mechanism: Corticosteroids are potent anti-inflammatory agents that work by suppressing a wide range of inflammatory pathways, including the production of cytokines like IL-1β.
- Forms & When to Use: Oral corticosteroids (e.g., prednisone) are effective for widespread or severe attacks, or when NSAIDs and colchicine are contraindicated (e.g., kidney disease, GI bleeding history). Intra-articular injections (e.g., triamcinolone) can provide rapid, localized relief for single-joint attacks. Intramuscular injections are also an option.
- Side Effects: While effective, corticosteroids carry their own set of side effects, especially with long-term use (e.g., increased blood sugar, fluid retention, mood changes, bone density loss). For acute attacks, short courses are generally well-tolerated.
- Narrative Element: The Prednisone Paradox. "After an attack that simply wouldn’t yield to NSAIDs, my doctor prescribed a short course of prednisone. The relief was almost instantaneous, a blessed reprieve from the agony. It felt like a miracle drug. But I learned to respect its power; it’s a potent tool for emergencies, not a casual solution, and careful tapering is essential to avoid rebound flares."
2. Non-Pharmacological Comfort Measures: The Soothers and Stabilizers
While medications fight the biochemical battle, these measures provide crucial physical and psychological support.
- Rest and Elevation: Immobilizing the affected joint is critical. Movement exacerbates pain. Elevating the limb above heart level helps reduce swelling by promoting fluid drainage. Imagine the joint as a battlefield; you wouldn’t send more troops into a mosh pit.
- Cold Therapy: Applying ice packs (wrapped in a cloth to prevent frostbite) for 15-20 minutes at a time, several times a day, can significantly reduce pain and swelling. The cold constricts blood vessels, reducing blood flow to the inflamed area and numbing nerve endings. Narrative: The Frozen Pea Bag Saga. "My grandmother swore by a bag of frozen peas. It was the perfect size, molded to her foot, and always ready in the freezer. It became a symbol of comfort, a small ritual of defiance against the pain."
- Hydration: While not an immediate pain reliever, staying well-hydrated with water is always beneficial. It helps flush the kidneys and maintain overall metabolic balance. Avoid sugary drinks or alcohol.
- Loose Clothing/Footwear: Any pressure on the inflamed joint is excruciating. Loose socks, open-toed slippers, or even going barefoot (if safe and practical) are essential.
- Distraction Techniques: When pain is overwhelming, engaging the mind can provide a temporary escape. Gentle music, reading, mindfulness exercises, or deep breathing techniques can shift focus away from the throbbing.
- Pain Management Positioning: Experiment with pillows and blankets to find the absolute least painful position for the affected limb. Sometimes, a slight elevation or a specific angle can make a world of difference.
The Strategic Long-Term Toolkit: Beyond the Acute Attack – Preventing Recurrence
The acute attack is a crisis, but it’s also a wake-up call. The period between attacks, known as the "intercritical" phase, is not a time for complacency but for strategic planning. This toolkit focuses on preventing future attacks and managing the underlying hyperuricemia.
1. Uric Acid Lowering Therapy (ULT): The Architects of Prevention
The cornerstone of long-term gout management is lowering and maintaining serum uric acid levels below a target threshold, typically <6 mg/dL, and for those with tophi, often <5 mg/dL. This dissolves existing crystals and prevents new ones from forming.
-
Allopurinol: The Gold Standard
- Mechanism: Allopurinol is a xanthine oxidase inhibitor (XOI). It blocks the enzyme responsible for converting purines into uric acid, thereby reducing uric acid production.
- Dosage & Titration: Allopurinol is started at a low dose (e.g., 50 mg or 100 mg daily) and slowly titrated upwards, typically by 50-100 mg every 2-4 weeks, until the target uric acid level is achieved. This gradual approach minimizes the risk of precipitating an attack.
- Starting During an Attack: While historically controversial, current guidelines suggest that ULT can be initiated during an acute attack, provided appropriate anti-inflammatory prophylaxis (colchicine or NSAIDs) is also given. The rationale is that rapid shifts in uric acid can trigger attacks, so starting ULT while treating the inflammation is a pragmatic approach for many.
- Hypersensitivity Syndrome: A rare but severe side effect, Allopurinol Hypersensitivity Syndrome (AHS), is more common in patients with certain HLA-B*5801 genotypes (prevalent in some Asian populations and African Americans) and those with kidney impairment. Genetic testing may be considered for at-risk groups.
- Narrative Element: The Allopurinol Journey. "My Uncle Arthur hated taking pills. But after years of debilitating attacks, he finally committed to Allopurinol. It wasn’t an overnight fix; it took months to find the right dose and for his body to adjust. He also had a few mild flares initially, which his doctor explained were part of the process as old crystals dissolved. But slowly, steadily, the attacks became less frequent, then less severe, until they were a distant memory. It was a journey of patience and adherence, but it gave him his life back."
-
Febuxostat: The Alternative XOI
- Mechanism: Febuxostat is another selective xanthine oxidase inhibitor, offering an alternative for patients who cannot tolerate or do not respond adequately to allopurinol.
- When to Use: Often prescribed for patients with moderate to severe kidney impairment where allopurinol dosing can be challenging, or for those who experienced adverse reactions to allopurinol.
- Cardiovascular Concerns: The FDA issued a warning regarding an increased risk of cardiovascular death with febuxostat compared to allopurinol in a large safety study. This makes shared decision-making with a physician crucial, weighing risks and benefits.
-
Probenecid: The Uricosuric Agent
- Mechanism: Probenecid works differently; it enhances the kidneys’ ability to excrete uric acid, making it a "uricosuric" agent.
- When to Use: Primarily used in "under-excretors" (patients whose kidneys don’t efficiently remove uric acid) with good kidney function.
- Contraindications: Not suitable for patients with a history of kidney stones or impaired kidney function, as it can increase the risk of stone formation.
-
Pegloticase: The Last Resort, The New Beginning
- Mechanism: Pegloticase is an intravenous enzyme that converts uric acid into allantoin, a harmless, water-soluble compound readily excreted by the kidneys.
- When to Use: Reserved for severe, refractory chronic tophaceous gout that has not responded to other ULTs. It can rapidly dissolve large tophi and bring uric acid levels down dramatically.
- Challenges: Administered by IV infusion every two weeks, it carries a risk of infusion reactions and the development of anti-drug antibodies, which can lead to loss of efficacy.
- Narrative Element: The Patient Who Regained Mobility. "Mr. Henderson, a man in his 60s, had gout so severe his joints were deformed with tophi, and he could barely walk. He’d tried everything. Pegloticase was his last hope. The journey was challenging, with careful monitoring, but within months, his tophi began to shrink, his pain receded, and he started to regain mobility he thought was lost forever. It was a testament to the power of targeted therapy for the most severe cases."
2. Lifestyle Modifications: The Foundation of Health
Medications are powerful, but they work best when supported by a healthy lifestyle. These are not merely suggestions; they are integral components of the long-term toolkit.
-
Dietary Awareness:
- High-Purine Foods to Limit: Red meat, organ meats (liver, kidneys), shellfish (shrimp, scallops, mussels), and foods/drinks high in high-fructose corn syrup (soda, fruit juices).
- Moderate Purine Foods: Poultry, fish (not shellfish), lentils, beans. These can be consumed in moderation.
- Beneficial Foods: Cherries (and cherry juice) have demonstrated uric acid-lowering and anti-inflammatory properties. Coffee, vitamin C, and low-fat dairy products have also been associated with a lower risk of gout.
- Narrative Element: The Diet Detective. "I once worked with a patient who meticulously tracked his diet and flares. He discovered that even small amounts of beer or certain types of seafood were immediate triggers for him, while others could tolerate them. He became his own ‘diet detective,’ learning his body’s unique sensitivities, proving that personalized dietary management is key."
-
Alcohol Moderation: Especially beer and spirits, which contribute significantly to uric acid levels. Wine, in moderation, appears to have less impact, but complete abstinence or significant reduction is often recommended.
-
Weight Management: Obesity is a major risk factor for gout and metabolic syndrome. Losing weight, even modestly, can significantly lower uric acid levels and reduce the strain on joints. However, rapid weight loss (e.g., crash diets) can sometimes trigger attacks due to increased ketone body production, which competes with uric acid excretion. A slow, sustainable approach is best.
-
Hydration (Again): Consistent, adequate water intake is crucial for kidney function and helping to excrete uric acid.
-
Exercise (Gentle, Regular): Not during an acute attack, but regular, low-impact exercise (walking, swimming, cycling) promotes overall health, aids in weight management, and improves joint health.
-
Stress Management: Chronic stress can contribute to inflammation and overall metabolic imbalance. Techniques like yoga, meditation, deep breathing, or engaging in hobbies can be invaluable.
-
Regular Monitoring: Regular blood tests to monitor uric acid levels are essential to ensure ULT is working and to adjust dosages as needed. Monitoring kidney function, blood pressure, lipids, and glucose is also important, as gout often co-exists with other metabolic conditions.
-
Communication with Healthcare Provider: This is perhaps the most critical component. Gout management is highly individualized. A strong, open relationship with a rheumatologist or general practitioner who understands gout is paramount for personalized treatment plans, medication adjustments, and managing comorbidities.
The Psychological Toolkit: Mindset and Resilience
Living with a chronic condition like gout extends beyond physical symptoms; it deeply impacts mental and emotional well-being. The psychological toolkit empowers individuals to navigate this often-overlooked aspect of the disease.
-
Acceptance, Not Resignation: Gout is a chronic condition, but it is manageable. Accepting this reality allows one to move from a place of helplessness to proactive management. It’s not about giving up; it’s about acknowledging the challenge and committing to a sustainable path forward.
-
Empowerment Through Knowledge: Understanding the pathophysiology, triggers, and treatment options reduces fear and anxiety. Knowledge transforms the unknown into the manageable. It allows patients to ask informed questions, participate in shared decision-making, and feel more in control.
-
Building a Support System: You are not alone. Connecting with family, friends, or online communities of people living with gout can provide invaluable emotional support, practical advice, and a sense of shared experience. Sharing stories and strategies can be incredibly therapeutic.
-
Tracking and Journaling: Keeping a record of attacks (date, duration, severity, potential triggers, medications used, and their effectiveness) can reveal patterns and help refine management strategies. It’s a personal data repository for better self-management and discussions with your doctor.
-
Patience and Persistence: Gout management is a marathon, not a sprint. Finding the right medication and dosage, adapting lifestyle, and seeing results takes time. There will be setbacks, but persistence in adherence to treatment and lifestyle changes is key.
- Narrative Element: The Mental Marathon. "After my initial diagnosis, I felt defeated. Every meal was a minefield, every twinge a harbinger of doom. But slowly, with the support of my doctor and my family, I started to shift my mindset. I learned to see each day as an opportunity to make choices that supported my health, rather than fearing the next attack. It was a mental marathon, teaching myself patience and celebrating small victories – a week without pain, a successful social gathering, a sustained period of low uric acid. This mental shift, as much as any pill, was what truly freed me."
Conclusion: Don’t Suffer in Silence, Build Your Toolkit
The narrative of gout doesn’t have to be one of relentless suffering. While its attacks are undeniably brutal, the modern understanding of the disease, coupled with an array of effective treatments and strategic lifestyle choices, offers a powerful path to management and prevention. The Gout Attack Toolkit is not a static list; it’s a dynamic, personalized strategy for resilience.
It begins with the immediate, decisive action during an attack, leveraging the pharmacological heavy hitters – NSAIDs, colchicine, and corticosteroids – alongside comforting non-pharmacological measures. It extends into the long-term, strategic deployment of Uric Acid Lowering Therapy, meticulously tailored to individual needs, supported by fundamental lifestyle modifications that reinforce overall health. And crucially, it embraces the psychological dimension, fostering acceptance, empowering through knowledge, and building resilience to navigate the emotional landscape of a chronic condition.
To the knowledgeable audience, those who understand the nuances of this complex disease, this toolkit is a call to action. Don’t suffer in silence. Engage with your healthcare providers, educate yourselves, build your personal arsenal, and empower yourselves to reclaim control from the clutches of gout. The path to a pain-free, active life is within reach – one informed decision, one strategic action, one resilient step at a time.