The Silent Deficiency: Are You Missing Out on Magnesium’s Major Heart and Bone Benefits?
Prologue: The Unseen Architect
In the grand, intricate design of the human body, there exist unsung heroes – fundamental elements whose silent work underpins our very existence. Among these, magnesium stands as a true master architect, orchestrating a myriad of biological processes with quiet precision. Yet, despite its colossal importance, it often remains relegated to the background, a mineral frequently overlooked, misunderstood, and, most critically, deficient in a significant portion of the global population. This is the story of magnesium, the silent deficiency, and the profound, often unrecognized, impact it wields over the very foundations of our health: our cardiovascular system and our skeletal structure.
Imagine for a moment a colossal, bustling city. Its power grid hums with energy, its traffic flows smoothly, its buildings stand strong against the elements, and its communication networks link every district. Now, imagine a tiny, almost invisible component within this city – a specific type of bolt, a crucial electrical connector, a binding agent in the concrete. If this seemingly minor component were to degrade, become scarce, or simply fail to perform its duty, the entire city would begin to falter. Power flickers, traffic snarls, structures weaken, and communication breaks down. This city is your body, and that critical, often-missing component is magnesium.
For the knowledgeable audience, the narrative of magnesium is not just a list of enzymatic reactions; it’s a testament to the elegant complexity of human physiology and a cautionary tale about the subtle erosion of health in the modern era. We will delve deep into the cellular mechanics, the biochemical pathways, and the epidemiological insights that paint a vivid picture of magnesium’s indispensable role, focusing intently on its guardianship of the heart and the bedrock of our bones.
I. The Blueprint of Life: Magnesium’s Foundational Roles
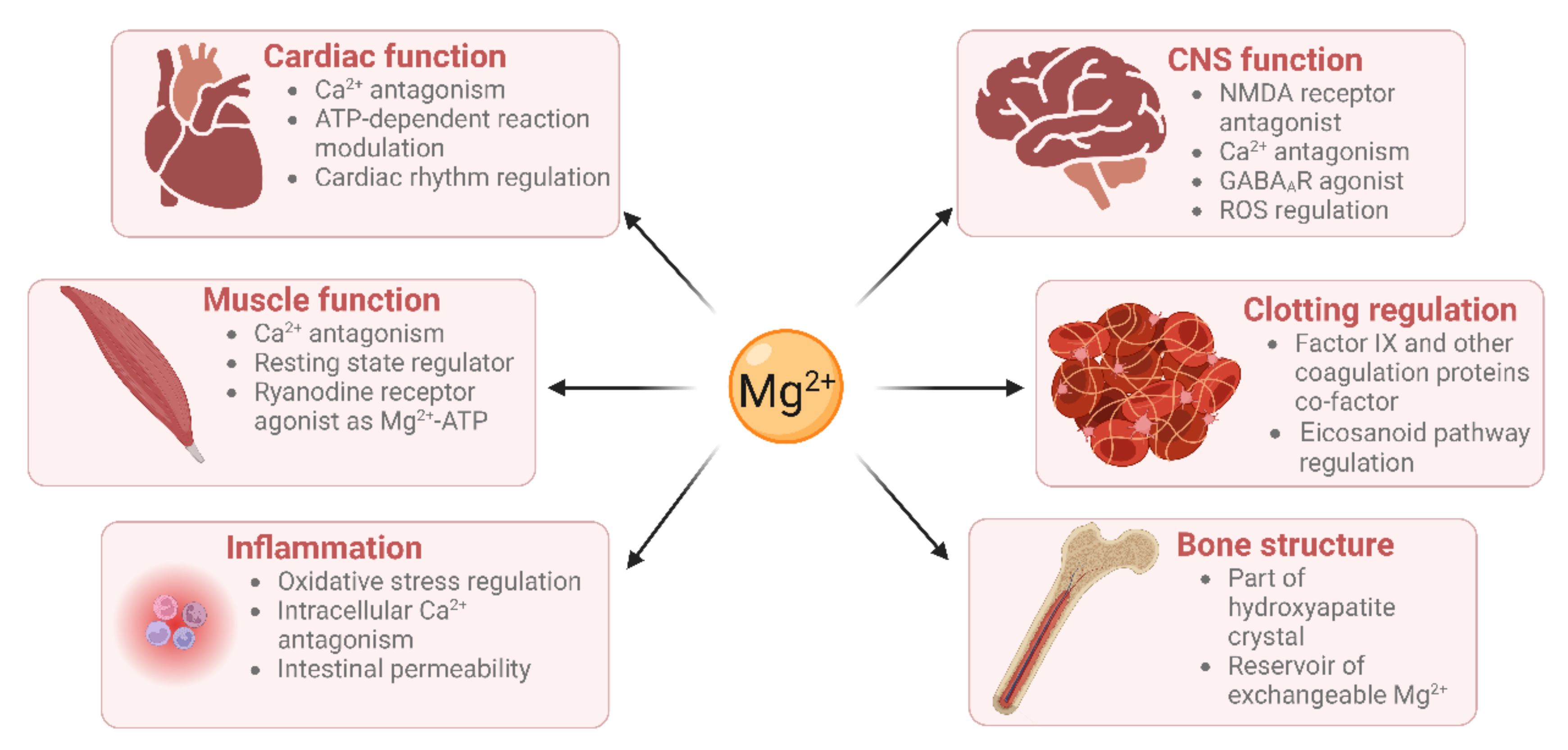
Before we zoom in on the heart and bones, it’s imperative to establish the sheer breadth of magnesium’s influence. It is not merely a supplementary player but a fundamental building block, a ubiquitous cofactor involved in over 300 enzymatic reactions within the body. To put this in perspective, think of magnesium as the universal key that unlocks countless biochemical doors.
At the very core of our energy production, magnesium is indispensable. It forms a complex with ATP (adenosine triphosphate), the primary energy currency of the cell. Without this magnesium-ATP complex, the enzymes that utilize ATP cannot function effectively, meaning our cells cannot generate or utilize energy efficiently. From the contraction of a muscle cell to the firing of a neuron, every single energy-dependent process relies on this critical partnership.
Beyond energy, magnesium plays a pivotal role in the synthesis of DNA and RNA, the very blueprints of life, and in protein synthesis, the construction of all the functional components of our cells. It helps maintain the structural integrity of cell membranes and influences the transport of other vital ions, such as calcium and potassium, across these membranes. This membrane stability is crucial for nerve impulse conduction, muscle contraction, and maintaining the electrical potential of cells – especially pertinent to the rhythmic beat of the heart.
Furthermore, magnesium is involved in glucose metabolism and insulin signaling, acting as a key regulator in blood sugar control. It has anti-inflammatory properties and acts as a natural calcium channel blocker, influencing vascular tone and blood pressure. Its sedative effects on the nervous system underscore its role in stress response and sleep regulation.
In essence, magnesium is a foundational nutrient, a silent partner in virtually every significant physiological process. Its pervasive influence means that a deficiency, however subtle, can ripple through multiple systems, manifesting in a diverse and often perplexing array of symptoms.
II. The Silent Erosion: Why We’re Falling Short
If magnesium is so vital, why is its deficiency so widespread? The answer lies in a confluence of factors deeply embedded in modern lifestyles and agricultural practices, painting a narrative of slow, insidious erosion.
The story begins with the soil. Decades of intensive farming practices, reliant on synthetic fertilizers (which often deplete magnesium) and monoculture, have stripped our agricultural lands of their natural mineral content. The vibrant, nutrient-rich soil of yesteryear, teeming with microorganisms that made minerals bioavailable to plants, is increasingly a rarity. Consequently, the fruits, vegetables, and grains we consume today often contain significantly less magnesium than they did even a few decades ago.
Next, consider the journey from farm to fork. The processing of foods, a hallmark of modern diets, further exacerbates the problem. Refining grains, for instance, removes the germ and bran – precisely where the majority of magnesium resides. White flour, white rice, and processed sugars are magnesium-poor compared to their whole-grain counterparts. Fast food, convenience meals, and sugary beverages, which dominate many diets, are nutritional deserts when it comes to this crucial mineral.
Beyond diet, several other factors conspire to deplete our magnesium stores:
- Stress: Chronic psychological and physiological stress increases the excretion of magnesium from the body. The "fight or flight" response, while essential for survival, consumes magnesium at an accelerated rate.
- Medications: Many commonly prescribed drugs can lead to magnesium depletion. Diuretics, often used for hypertension or heart failure, increase magnesium excretion. Proton pump inhibitors (PPIs), used for acid reflux, can impair magnesium absorption. Certain antibiotics and chemotherapy drugs also fall into this category.
- Alcohol: Excessive alcohol consumption not only impairs magnesium absorption but also increases its excretion through the kidneys.
- Medical Conditions: Conditions such as Crohn’s disease, celiac disease, and other malabsorption syndromes can hinder the body’s ability to absorb magnesium from food. Diabetes can lead to increased urinary excretion of magnesium.
- Excessive Calcium Intake: While calcium is crucial, an imbalance with magnesium can be detrimental. High calcium intake without adequate magnesium can actually increase magnesium requirements, as these two minerals compete for absorption and have opposing actions in many physiological processes (e.g., muscle contraction vs. relaxation).
- Aging: As we age, our digestive efficiency can decrease, leading to reduced absorption of nutrients, including magnesium. Kidney function may also decline, affecting magnesium retention.
This complex interplay of factors means that even individuals who believe they maintain a healthy diet might inadvertently be living with a chronic, low-grade magnesium deficiency, quietly undermining their long-term health.
III. The Heart’s Unsung Guardian: Magnesium and Cardiovascular Health
The heart, a tireless pump that beats approximately 100,000 times a day, is profoundly dependent on magnesium. Its role here is multifaceted, touching upon electrical stability, vascular tone, blood pressure regulation, and metabolic health. To understand this, let’s consider the heart as a finely tuned orchestra, and magnesium as its crucial conductor, ensuring harmony and preventing discordant notes.
A. The Electrical Symphony: Preventing Arrhythmias
The heart’s rhythm is governed by a precise electrical impulse generation and conduction system. This electrical activity relies on the controlled movement of ions – sodium, potassium, and calcium – across myocardial cell membranes. Magnesium is a critical regulator of these ion channels.
- Potassium Channels: Magnesium influences the activity of potassium channels, which are vital for repolarization (the recovery phase) of cardiac cells after each beat. A magnesium deficiency can lead to potassium depletion within cells, making the heart muscle more excitable and prone to irregular rhythms.
- Calcium Channels: Magnesium acts as a natural calcium channel blocker. While calcium is essential for muscle contraction, excessive intracellular calcium can lead to over-excitation and contribute to arrhythmias. Magnesium helps to modulate calcium influx, ensuring a balanced contraction and relaxation cycle.
Clinically, magnesium deficiency is strongly associated with various arrhythmias, including atrial fibrillation, ventricular premature beats, and even life-threatening ventricular tachycardias. In acute settings, intravenous magnesium is a standard treatment for certain types of arrhythmias, particularly Torsades de Pointes, demonstrating its immediate and profound impact on cardiac electrical stability.
B. The Pressure Regulator: Blood Pressure Control
Hypertension, or high blood pressure, is a leading risk factor for heart disease and stroke. Magnesium contributes to blood pressure regulation through several mechanisms:
- Vasodilation: Magnesium promotes the relaxation of smooth muscle cells in the walls of blood vessels, leading to vasodilation (widening of the vessels). This reduces peripheral vascular resistance, thereby lowering blood pressure.
- Nitric Oxide Production: Magnesium is involved in the synthesis of nitric oxide (NO), a powerful vasodilator produced by endothelial cells lining blood vessels.
- Sodium-Potassium Pump: By optimizing the function of the sodium-potassium pump, magnesium helps regulate the balance of electrolytes within cells, which impacts cellular volume and vascular tone.
- Calcium Modulation: Its role in moderating intracellular calcium levels also prevents excessive vasoconstriction, contributing to lower blood pressure.
Numerous studies have shown an inverse relationship between magnesium intake and blood pressure, with magnesium supplementation often leading to modest but clinically significant reductions in both systolic and diastolic blood pressure, particularly in individuals with existing hypertension.
C. Vascular Integrity: Preventing Calcification and Endothelial Dysfunction
Beyond blood pressure, magnesium plays a crucial role in maintaining the structural integrity and health of blood vessels themselves:
- Anti-Calcification: One of magnesium’s most vital, yet underappreciated, roles is its ability to inhibit vascular calcification. Inadequate magnesium allows calcium to accumulate in the soft tissues, including the arterial walls, contributing to atherosclerosis and arterial stiffness. Magnesium helps keep calcium soluble and directs it towards bones and teeth, where it belongs. This is particularly relevant when considering the interplay with Vitamin K2 and Vitamin D, forming a triumvirate that guides calcium metabolism effectively.
- Endothelial Function: The endothelium, the inner lining of blood vessels, plays a critical role in vascular health. Magnesium supports healthy endothelial function, ensuring proper vasodilation and preventing the initiation of atherosclerotic plaques.
- Anti-Inflammatory Effects: Chronic low-grade inflammation is a key driver of cardiovascular disease. Magnesium has anti-inflammatory properties, reducing markers of inflammation like C-reactive protein (CRP), thereby protecting the cardiovascular system from damage.
D. Metabolic Synergy: Insulin Sensitivity and Glucose Control
Magnesium’s influence extends to metabolic health, which is intricately linked to cardiovascular well-being. It is a critical cofactor for enzymes involved in glucose metabolism. Deficiency impairs insulin signaling, leading to insulin resistance, a precursor to Type 2 diabetes and a significant risk factor for heart disease. By improving insulin sensitivity, magnesium indirectly contributes to better blood lipid profiles and reduced cardiovascular risk.
In summary, magnesium is a comprehensive cardiovascular protector, acting on multiple fronts to ensure the heart’s electrical stability, maintain healthy blood pressure, preserve vascular elasticity, and foster metabolic harmony. Its deficiency, therefore, creates a cascade of vulnerabilities that can lead to a spectrum of cardiac ailments.
IV. The Bone’s Bedrock: Magnesium’s Role in Skeletal Strength
While calcium typically steals the spotlight when it comes to bone health, magnesium is the silent architect that provides the true bedrock of skeletal strength. Without adequate magnesium, calcium cannot be properly utilized, leading to weakened bones despite sufficient calcium intake. Imagine bones as ancient fortresses, and magnesium as the master builder and repairman, ensuring their resilience and structural integrity.
A. Direct Structural Component: The Bone Matrix
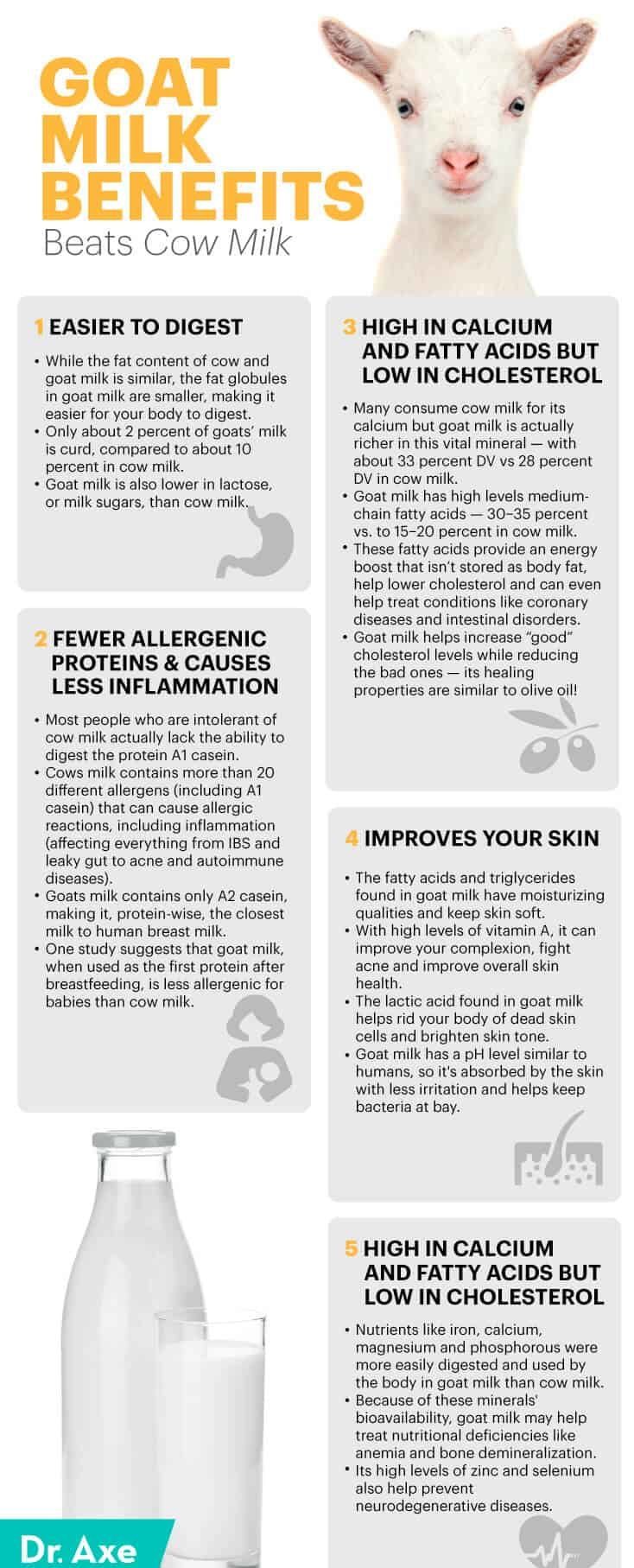
Approximately 50-60% of the body’s total magnesium is stored in the bones, making it a fundamental structural component of the bone matrix itself. Magnesium ions are incorporated into the crystal lattice of hydroxyapatite, the primary mineral of bone, contributing to its density and strength. It’s not just a bystander; it’s an integral part of the bone’s physical structure.
B. The Calcium-Vitamin D-Magnesium Triumvirate
This is perhaps where magnesium’s role in bone health becomes most profound and complex. Magnesium is the crucial, often-missing link in the metabolism of both calcium and vitamin D, forming a vital triumvirate that dictates bone mineral density and remodeling.
- Vitamin D Activation: Vitamin D is not active in its dietary or sunlight-derived form. It requires two hydroxylation steps to become calcitriol, its active hormonal form. Both of these steps are magnesium-dependent. Without sufficient magnesium, vitamin D remains largely inactive, rendering calcium absorption inefficient and impairing its ability to regulate bone metabolism, even if vitamin D levels appear adequate on blood tests.
- Calcium Regulation: Magnesium directly influences calcium homeostasis in several ways. It regulates the parathyroid hormone (PTH), which is a key player in maintaining calcium levels in the blood. PTH signals the body to release calcium from bones if blood levels are too low. Magnesium deficiency can impair PTH secretion and function, leading to dysregulated calcium levels. Furthermore, as discussed, magnesium helps prevent ectopic calcification, ensuring calcium is directed to bones and teeth rather than soft tissues.
- Osteoblast and Osteoclast Activity: Magnesium impacts the balance between osteoblasts (bone-building cells) and osteoclasts (bone-resorbing cells). It helps to stimulate osteoblast activity and regulate osteoclast differentiation and function, thereby promoting bone formation and preventing excessive bone breakdown.
Studies have shown that low magnesium intake is associated with reduced bone mineral density, an increased risk of osteoporosis, and higher rates of bone fractures, independent of calcium intake. This underscores the point that simply consuming more calcium without addressing magnesium deficiency is akin to trying to build a strong house with plenty of bricks but no mortar.
C. Preventing Bone Loss and Fractures
Magnesium’s direct and indirect roles culminate in its ability to protect against bone loss. By ensuring optimal vitamin D activation, regulating PTH, promoting calcium absorption and utilization, and contributing directly to bone structure, magnesium stands as a formidable guardian against conditions like osteopenia and osteoporosis. For older adults, particularly postmenopausal women, who are at higher risk for these conditions, ensuring adequate magnesium intake becomes paramount for maintaining skeletal integrity and reducing the devastating impact of fragility fractures.
V. The Elusive Diagnosis: Detecting the Undetectable
Given magnesium’s profound importance, one might assume its deficiency would be easily identified. However, this is where the "silent" in "silent deficiency" truly comes into play, making diagnosis notoriously challenging. The story of diagnosing magnesium deficiency is often one of frustration and missed opportunities.
The primary reason for this difficulty lies in magnesium’s distribution within the body. Only about 1% of the body’s total magnesium is found in the blood serum. The vast majority resides within cells (intracellularly) and in bone. When serum magnesium levels drop, the body has sophisticated mechanisms to pull magnesium from bone and other cellular stores to maintain this critical extracellular balance. This means that a standard serum magnesium test can often appear "normal" even when the body’s overall magnesium reserves are significantly depleted. It’s like checking the water level in a small pond and assuming the entire underground aquifer is full.
Consequently, symptoms of magnesium deficiency are often vague, non-specific, and can mimic other conditions, further complicating diagnosis. These symptoms can include:
- Neuromuscular: Muscle cramps, spasms, tremors, restless legs syndrome, general weakness.
- Neurological/Psychological: Fatigue, anxiety, depression, irritability, insomnia, headaches, migraines.
- Cardiovascular: Palpitations, arrhythmias, high blood pressure.
- Metabolic: Insulin resistance, sugar cravings.
- Other: Nausea, loss of appetite, premenstrual syndrome (PMS) symptoms, constipation.
For a knowledgeable audience, it’s crucial to understand that relying solely on serum magnesium levels for assessment is inadequate. More comprehensive diagnostic approaches, though not always routinely available, might include:
- Red Blood Cell (RBC) Magnesium: This test measures magnesium inside red blood cells, which can be a better indicator of intracellular magnesium status than serum levels.
- Magnesium Loading Test (Magnesium Retention Test): This involves administering a specific dose of magnesium intravenously and then measuring the amount excreted in the urine over 24 hours. If a significant amount is retained, it suggests a deficiency.
- Clinical Symptom Assessment: A thorough medical history and evaluation of symptoms, especially when multiple risk factors for deficiency are present, can be a valuable diagnostic tool, guiding a trial of supplementation.
The elusive nature of magnesium deficiency means that clinicians must maintain a high index of suspicion, especially in patients presenting with a constellation of non-specific symptoms or those with known risk factors.
VI. Reclaiming the Balance: Dietary Strategies and Supplementation
The story of magnesium deficiency doesn’t end in resignation; it’s a call to action, a narrative of reclaiming balance through informed dietary choices and, when necessary, targeted supplementation.
A. Food First: Nature’s Bounty
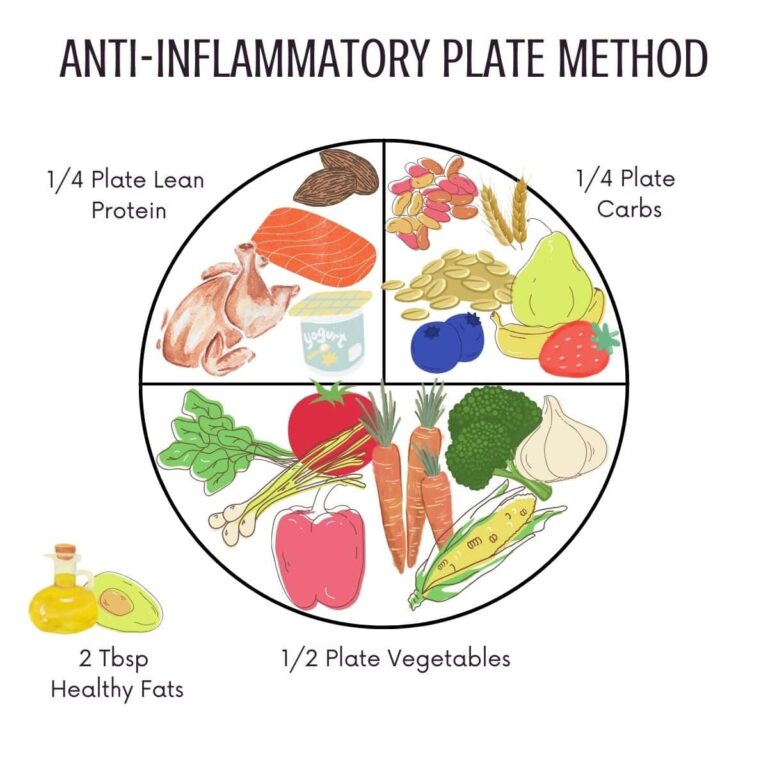
The most fundamental and safest approach to ensure adequate magnesium intake is through diet. Nature has provided an abundance of magnesium-rich foods, particularly those that are minimally processed:
- Leafy Green Vegetables: Spinach, kale, Swiss chard are magnesium powerhouses. Chlorophyll, the green pigment in plants, has magnesium at its core.
- Nuts and Seeds: Almonds, cashews, peanuts, pumpkin seeds, chia seeds, flaxseeds are excellent sources.
- Legumes: Black beans, lentils, chickpeas, and soybeans are rich in magnesium.
- Whole Grains: Brown rice, oats, quinoa, and whole wheat are superior to their refined counterparts.
- Avocados: A delicious and healthy source.
- Bananas: A good source of both magnesium and potassium.
- Dark Chocolate: The higher the cocoa content, the more magnesium. A delicious way to boost intake in moderation!
- Fatty Fish: Salmon, mackerel, and halibut contain magnesium.
- Mineral Water: Some mineral waters can provide significant amounts of bioavailable magnesium.
Emphasizing a diet rich in whole, unprocessed foods, with a strong focus on plant-based sources, is the cornerstone of preventing and addressing magnesium deficiency. Cooking methods that minimize nutrient loss (e.g., steaming over boiling) are also beneficial.
B. When Food Isn’t Enough: Supplementation Considerations
Despite best efforts, given the depleted soil, food processing, and various lifestyle factors, dietary intake alone may not always be sufficient to replete magnesium stores, especially in cases of established deficiency or increased need. This is where supplementation becomes a valuable tool, but it requires a nuanced approach for the knowledgeable audience.
There are various forms of magnesium supplements, each with different bioavailability and potential side effects:
- Magnesium Citrate: A common and well-absorbed form, often used for its mild laxative effect.
- Magnesium Glycinate/Bisglycinate: Highly bioavailable and generally well-tolerated, less likely to cause digestive upset. Often preferred for its calming properties and for individuals with sensitive digestive systems.
- Magnesium Threonate: Unique for its ability to cross the blood-brain barrier, making it potentially beneficial for cognitive function and neurological health.
- Magnesium Malate: Often recommended for individuals with fatigue or muscle pain, as malate is involved in energy production.
- Magnesium Chloride: Found in magnesium oil sprays (for transdermal absorption) and some oral supplements. Can be well-absorbed.
- Magnesium Oxide: While it contains a high percentage of elemental magnesium, its bioavailability is poor. It’s often used as a laxative rather than for systemic magnesium repletion.
- Magnesium Taurate: Combines magnesium with taurine, an amino acid known for its cardiovascular benefits, making it potentially synergistic for heart health.
Dosage and Administration:
The Recommended Dietary Allowance (RDA) for magnesium for adults generally ranges from 310-420 mg per day, depending on age and gender. However, therapeutic doses for deficiency can be higher, often ranging from 200-600 mg elemental magnesium per day, split into multiple doses to improve absorption and minimize digestive side effects.
Potential Side Effects:
The most common side effect of oral magnesium supplementation is gastrointestinal upset, primarily diarrhea, especially with higher doses or less bioavailable forms like magnesium oxide or citrate. This can often be mitigated by reducing the dose, switching to a more bioavailable form (like glycinate), or taking it with food.
Interactions and Precautions:
- Medications: Magnesium can interact with certain medications, including antibiotics (tetracyclines and quinolones), diuretics, and proton pump inhibitors. It’s crucial to consult a healthcare professional before starting supplementation, especially if on prescription drugs.
- Kidney Disease: Individuals with impaired kidney function should exercise extreme caution with magnesium supplementation, as their kidneys may not be able to excrete excess magnesium, leading to hypermagnesemia (magnesium toxicity), which can be dangerous.
- Other Supplements: While magnesium works synergistically with vitamin D and K2, it’s important to consider the balance. Excessive calcium supplementation without adequate magnesium can be problematic.
For the knowledgeable individual, understanding these nuances allows for a more informed discussion with healthcare providers, moving beyond a simple recommendation to a personalized and effective strategy for magnesium repletion.
VII. A Holistic Perspective: Magnesium in the Symphony of Health
While our focus has been primarily on the heart and bones, it’s important to reiterate that magnesium’s influence extends across the entire physiological landscape. It contributes to:
- Neurological Health: Reducing anxiety, improving mood, alleviating migraines, and supporting sleep quality.
- Muscle Function: Preventing cramps, improving exercise performance, and aiding recovery.
- Blood Sugar Regulation: As discussed, enhancing insulin sensitivity.
- Anti-Inflammatory Response: Contributing to overall immune health.
Magnesium doesn’t operate in isolation; it’s a vital player in the body’s interconnected symphony. Addressing a magnesium deficiency often yields improvements across multiple systems, creating a ripple effect of enhanced well-being. This holistic perspective underscores that correcting a silent deficiency isn’t just about patching a specific problem but about restoring overall physiological harmony.
VIII. Epilogue: The Awakening
The story of magnesium is a profound narrative of a hidden hero, a ubiquitous yet underappreciated mineral whose silent deficiency can slowly, insidiously undermine the very pillars of our health: the rhythmic beat of our heart and the foundational strength of our bones. We have journeyed through its myriad roles, explored the reasons behind its widespread scarcity, and detailed its indispensable guardianship over cardiovascular and skeletal health.
For the knowledgeable individual, this story is an awakening – a call to re-evaluate what truly constitutes a healthy diet and lifestyle in the modern world. It’s an invitation to consider that persistent fatigue, muscle twitches, anxiety, or even seemingly unrelated conditions like arrhythmias or declining bone density, might trace their roots back to this silent, pervasive deficiency.
The good news is that this is a story with a hopeful ending. Armed with knowledge, we have the power to reclaim this vital balance. By prioritizing whole, unprocessed foods rich in magnesium, by understanding the factors that deplete it, and by considering judicious, informed supplementation when necessary, we can restore this master architect to its rightful place.
Let the silence of magnesium deficiency be broken by the resounding awareness of its profound importance. Let us recognize its role not as a mere supplement, but as a fundamental nutrient, a cornerstone of vibrant health, ensuring that our hearts beat strong and our bones stand firm for a lifetime. Consult with your healthcare professional, explore your dietary choices, and empower yourself with the knowledge to bring this silent hero back into the spotlight of your well-being. The story of magnesium is, ultimately, the story of our own potential for optimal health, waiting to be fully realized.