Beyond Water: The Electrolyte Balance Key to Preventing Dehydration Headaches
The Silent Thief: Unmasking the Dehydration Headache
Imagine this: the throbbing starts subtly, a dull ache behind your eyes, perhaps a slight pressure at your temples. You dismiss it, attributing it to a long day, screen time, or perhaps a lack of sleep. As the hours wear on, the ache intensifies, evolving into a relentless, pulsating torment that makes light unbearable and sound a piercing assault. You reach for the pain relievers, perhaps even a cup of coffee, and in a moment of common wisdom, you grab a glass of water. "I must be dehydrated," you think, downing the plain liquid with a sense of hopeful urgency.
Yet, for many, that glass of water, while momentarily soothing, doesn’t quite quell the storm. The headache persists, a stubborn reminder that something deeper is amiss. This familiar scenario plays out daily for millions, underscoring a fundamental misunderstanding of hydration. While water is undeniably the cornerstone of life, the simplistic mantra of "just drink more water" often falls short when it comes to truly preventing and resolving dehydration-induced headaches. The missing piece, the often-overlooked hero in this physiological drama, is the intricate dance of electrolytes.
For the knowledgeable audience, the distinction is critical. Dehydration isn’t merely a deficit of H₂O molecules; it’s a complex systemic imbalance that profoundly impacts cellular function, neuronal activity, and vascular regulation. And at the heart of this intricate web lies the precise concentration and distribution of electrolytes – the charged minerals that govern the very electrical impulses defining our existence. To truly understand and combat the dehydration headache, we must journey beyond the surface of a water glass and dive into the microscopic world of ionic equilibrium.
The Physiology of Pain: How Dehydration Triggers Headaches
Before we champion the cause of electrolytes, it’s essential to dissect the mechanisms by which dehydration, even in its mildest forms, can precipitate such debilitating head pain. This isn’t just about feeling thirsty; it’s about a cascade of physiological events that stress our most vital organ – the brain.
-
Cerebral Volume Changes and Meningeal Tension:
The human brain, remarkably, floats in cerebrospinal fluid (CSF) within the confines of the skull. This delicate environment maintains a precise osmotic balance with the blood. When the body becomes dehydrated, the blood plasma osmolarity (concentration of solutes) increases. Water, ever the equalizer, then shifts from areas of lower solute concentration (like the brain cells and CSF) to areas of higher concentration (the blood). This osmotic shift causes a slight, but significant, reduction in brain volume. Even a 1-2% decrease in brain water content can lead to a measurable shrinkage.
The brain itself lacks pain receptors, but its surrounding structures – the meninges (dura mater, arachnoid mater, pia mater) and the blood vessels embedded within them – are richly innervated with nociceptors (pain receptors). As the brain shrinks, it pulls on these pain-sensitive meninges and the bridging veins that traverse the subdural space. This traction and tension are primary culprits in generating the characteristic throbbing pain of a dehydration headache. -
Cerebral Blood Flow Alterations:
Dehydration also affects the cardiovascular system. As blood volume decreases, the body attempts to compensate by constricting blood vessels, especially in the periphery, to maintain blood pressure and prioritize flow to vital organs. While this compensatory mechanism is crucial, it can also lead to changes in cerebral blood flow. Reduced blood flow (ischemia) can deprive brain cells of oxygen and nutrients, leading to metabolic stress and the accumulation of waste products that irritate pain receptors.
Conversely, the brain’s autoregulatory mechanisms, sensing reduced blood volume, might initially cause vasoconstriction. However, as dehydration progresses or as rehydration efforts begin, there can be a reactive vasodilation. This rapid expansion of blood vessels, particularly the intracranial ones, can stretch their pain-sensitive walls, contributing to the pulsatile nature of the headache. -
Neurotransmitter Imbalance and Inflammation:
The brain is a complex electrochemical organ. Dehydration can disrupt the delicate balance of neurotransmitters – the chemical messengers that transmit signals between neurons. For instance, serotonin, a neurotransmitter heavily implicated in migraine pathogenesis, can be affected. Imbalances in electrolytes directly influence neuronal excitability and the efficiency of neurotransmission.
Furthermore, cellular stress induced by dehydration can trigger an inflammatory response. Pro-inflammatory cytokines and other mediators can be released, sensitizing pain pathways and exacerbating the headache. The metabolic byproducts of stressed cells, such as lactate, can also contribute to a localized acidic environment, further irritating nociceptors. -
Electrolyte-Mediated Cellular Dysfunction:
This is where the direct link to our core topic emerges. Every single physiological process, from nerve impulse transmission to muscle contraction and glandular secretion, hinges on the precise movement of ions across cell membranes. When dehydration causes a shift in overall fluid balance, it inevitably impacts the concentration and distribution of these crucial electrolytes, leading to cellular dysfunction that manifests as pain.
The Unsung Heroes: What Are Electrolytes?
Electrolytes are minerals in your body that have an electric charge. They are found in your blood, urine, tissues, and other body fluids. But their role goes far beyond mere presence; they are the literal "spark plugs" of the body, facilitating electrical impulses that drive virtually every bodily function. They are vital for:
- Fluid Balance: Regulating the amount of water inside and outside cells.
- Nerve Impulses: Transmitting signals between cells, especially in the brain and nervous system.
- Muscle Function: Essential for muscle contraction and relaxation, including the heart.
- pH Balance: Maintaining the body’s acid-base balance.
The primary electrolytes of concern for human health, and specifically for preventing dehydration headaches, include:
- Sodium (Na⁺): The primary cation in the extracellular fluid (outside cells).
- Potassium (K⁺): The primary cation in the intracellular fluid (inside cells).
- Magnesium (Mg²⁺): A crucial intracellular cation, involved in hundreds of enzymatic reactions.
- Calcium (Ca²⁺): Essential for nerve and muscle function, bone health.
- Chloride (Cl⁻): The primary anion in the extracellular fluid, often paired with sodium.
- Bicarbonate (HCO₃⁻): A key buffer in the blood, helping to maintain pH.
A Symphony of Ions: How Specific Electrolytes Prevent Headaches
Understanding the individual roles of these electrolytes reveals why their balance, not just water intake, is paramount in preventing dehydration headaches.
-
Sodium (Na⁺): The Osmotic Maestro
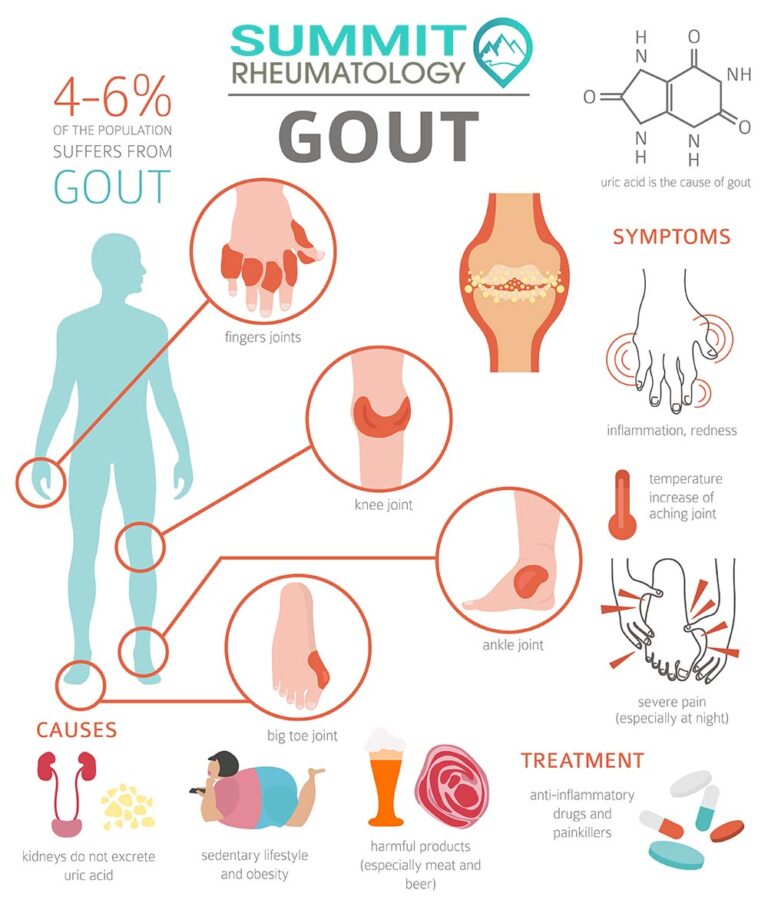
Sodium is the most abundant extracellular cation and the primary determinant of plasma osmolarity. It dictates where water goes. The famous sodium-potassium pump, present in virtually every cell membrane, actively transports sodium out of the cell and potassium into the cell, maintaining crucial electrochemical gradients.- Headache Connection: When sodium levels drop too low (hyponatremia), due to excessive plain water intake without adequate electrolyte replenishment (e.g., during intense exercise or illness), water floods into cells, causing them to swell. This cellular swelling, particularly in brain cells, can lead to cerebral edema, which is far more severe than brain shrinkage and can cause intense headaches, confusion, seizures, and even coma. Conversely, high sodium levels (hypernatremia), typically from severe dehydration without sufficient water or electrolyte intake, also disrupt osmotic balance, leading to brain cell shrinkage. Maintaining sodium within its narrow physiological range is critical for stable brain volume and preventing both forms of osmotic stress.
-
Potassium (K⁺): The Intracellular Regulator
Potassium is the primary intracellular cation, crucial for nerve impulse transmission, muscle contraction (including cardiac muscle), and maintaining intracellular fluid volume. It works in concert with sodium to establish the resting membrane potential of cells.- Headache Connection: Imbalances in potassium, often lost alongside sodium during sweating, vomiting, or diarrhea, can disrupt nerve signal transmission and muscle function. Hypokalemia (low potassium) can lead to muscle weakness, fatigue, and can indirectly contribute to headache by affecting overall cellular energy status and vascular tone. Its role in maintaining the sodium-potassium pump’s efficiency is vital for preventing the cellular swelling or shrinkage that precipitates headaches.
-
Magnesium (Mg²⁺): The Mighty Modulator
Magnesium is an often-overlooked but profoundly important electrolyte, involved in over 300 enzymatic reactions. It’s a natural calcium channel blocker, a muscle relaxant, and a neurotransmitter modulator.- Headache Connection: Magnesium’s role in headache prevention is particularly strong, especially for migraine sufferers. It helps relax blood vessels, preventing the spasms and constriction that can initiate or worsen headaches. It modulates the release of neurotransmitters, including serotonin, which is implicated in pain pathways. Magnesium also blocks the activity of N-methyl-D-aspartate (NMDA) receptors, which are involved in pain transmission and neuronal excitability. Low magnesium levels (hypomagnesemia) can increase neuronal excitability, making the brain more susceptible to headache triggers, including those related to dehydration. Many individuals with chronic headaches or migraines are found to be magnesium deficient.
-
Calcium (Ca²⁺): The Signal Transducer
While largely associated with bone health, calcium plays a vital role in nerve impulse transmission, muscle contraction, and cellular signaling.- Headache Connection: Calcium homeostasis is tightly regulated. While not as directly implicated in dehydration headaches as sodium, potassium, or magnesium, severe imbalances can indirectly contribute. For instance, calcium influx into neurons is critical for neurotransmitter release. Disruptions to this delicate balance, which can occur during severe electrolyte derangements, could theoretically impact brain function and pain perception. Calcium also plays a role in vascular tone, and dysregulation could contribute to the cerebrovascular changes seen in headaches.
-
Chloride (Cl⁻) & Bicarbonate (HCO₃⁻): The pH and Volume Guardians
Chloride is the most abundant extracellular anion, working closely with sodium to maintain osmotic pressure and fluid balance. Bicarbonate is a crucial buffer that helps regulate the body’s pH.- Headache Connection: Chloride often follows sodium, so its balance is intrinsically linked to fluid volume and osmotic stability. Significant losses, such as from vomiting, can exacerbate electrolyte imbalances. Bicarbonate’s role in pH balance is vital because deviations from optimal pH can impact enzyme function, protein structure, and overall cellular metabolism, contributing to cellular stress and potential headache triggers.
When Water Alone Isn’t Enough: Scenarios Demanding Electrolyte Awareness
Understanding the "why" allows us to identify the "when." There are numerous situations where relying solely on plain water for hydration is insufficient and can even be detrimental, actively promoting electrolyte imbalances and increasing the risk of dehydration headaches.
-
Intense Physical Activity & Heavy Sweating:
During strenuous exercise, especially in hot or humid conditions, the body can lose significant amounts of sweat. Sweat is not just water; it contains electrolytes, primarily sodium and chloride, but also potassium and magnesium. A marathon runner, for example, can lose liters of sweat per hour. Replenishing this fluid with only plain water dilutes the remaining electrolytes in the body, leading to hyponatremia (low sodium) and other deficiencies, which can manifest as headaches, muscle cramps, and fatigue. This is why sports drinks (ideally, those without excessive sugar) were initially formulated. -
Illness with Vomiting or Diarrhea:
Gastrointestinal illnesses that cause persistent vomiting or diarrhea lead to rapid and substantial losses of both fluid and electrolytes. Vomiting results in the loss of stomach acid (rich in chloride) and other digestive fluids, while diarrhea flushes out large quantities of sodium, potassium, and water. Attempting to rehydrate with plain water in these scenarios can worsen electrolyte depletion, making recovery slower and increasing the risk of headaches and more severe complications. Oral Rehydration Solutions (ORS) are specifically designed for these situations. -
Excessive Heat Exposure:
Working or spending prolonged time in hot environments without adequate protection or hydration leads to continuous sweating, even without strenuous exercise. The cumulative loss of electrolytes can quickly lead to an imbalance, manifesting as heat exhaustion symptoms, including headaches, dizziness, and muscle cramps. -
Alcohol Consumption (Hangovers):
Alcohol is a diuretic, meaning it increases urine production and causes the body to excrete more fluid than it takes in. This diuretic effect leads to dehydration and significant electrolyte losses, particularly potassium and magnesium. The characteristic headache of a hangover is not solely due to alcohol’s direct effects on the brain but is heavily influenced by this profound dehydration and electrolyte depletion. The brain shrinkage and vascular changes associated with dehydration are key players here. -
Certain Dietary Regimens (e.g., Ketogenic Diet):
Diets that significantly restrict carbohydrates, such as the ketogenic diet, lead to increased water and electrolyte excretion. When carbohydrate stores (glycogen) are depleted, the body releases the water bound to them. Furthermore, the kidneys excrete more sodium and potassium in the absence of insulin, which typically promotes their reabsorption. Individuals on these diets often experience the "keto flu," a constellation of symptoms including headaches, fatigue, and muscle cramps, which are largely attributable to electrolyte imbalances. -
Chronic Medical Conditions:
Certain medical conditions or medications can predispose individuals to electrolyte imbalances. Kidney disease, heart failure, uncontrolled diabetes, and diuretic medications can all impact the body’s ability to regulate fluid and electrolyte levels, making these individuals more susceptible to dehydration headaches. -
Elderly and Young Children:
These age groups are particularly vulnerable. The elderly often have a blunted thirst response, reduced kidney function, and may be on medications that affect fluid balance. Young children have a higher surface area-to-volume ratio, making them more prone to rapid fluid loss, and their ability to communicate thirst or symptoms may be limited.
Strategic Hydration: Practical Approaches to Electrolyte Balance
Given the critical role of electrolytes, a strategic approach to hydration moves beyond simply consuming water to consciously ensuring adequate electrolyte intake.
-
Dietary Sources: The Foundation of Balance
The most natural and sustainable way to maintain electrolyte balance is through a varied, nutrient-rich diet.- Sodium: While often demonized, adequate sodium is essential. Healthy sources include real sea salt, fermented foods (sauerkraut, pickles), and broths. Avoid excessive processed foods that contain hidden, unhealthy forms of sodium.
- Potassium: Abundant in fruits and vegetables. Think bananas, avocados, spinach, sweet potatoes, coconut water, oranges, and beans.
- Magnesium: Found in leafy green vegetables (spinach, kale), nuts (almonds, cashews), seeds (pumpkin, chia), legumes, whole grains, dark chocolate, and avocados.
- Calcium: Dairy products, fortified plant milks, leafy greens (collard greens, turnip greens), and fortified cereals.
- Chloride: Often found with sodium in salt, also in sea vegetables.
- Bicarbonate: The body primarily produces this, but some mineral waters contain it.
-
Electrolyte Supplements: When and Why
While diet is paramount, there are scenarios where supplementation becomes beneficial or even necessary:- Intense Exercise/Sweating: For workouts lasting longer than 60-90 minutes, especially in heat, a well-formulated electrolyte drink (low in sugar, balanced ratios of Na, K, Mg) can prevent hyponatremia and improve performance and recovery.
- Illness: Oral Rehydration Solutions (ORS) are medically recommended for vomiting and diarrhea. These contain precise ratios of sodium, potassium, chloride, glucose, and citrate to facilitate rapid absorption and rebalance.
- Ketogenic/Low-Carb Diets: Many individuals on these diets proactively supplement with sodium, potassium, and magnesium to prevent "keto flu" symptoms.
- Chronic Conditions/Medications: Under medical guidance, individuals with certain health conditions or those taking diuretics may require targeted electrolyte supplementation.
- Hangover Prevention/Remedy: Electrolyte-rich fluids before bed and upon waking can significantly mitigate hangover symptoms, including headaches.
When choosing a supplement, look for:
- Balanced Ratios: Not just high sodium, but also sufficient potassium and magnesium.
- Minimal Sugar: Excess sugar can negate benefits or cause digestive upset.
- Bioavailable Forms: For magnesium, forms like magnesium citrate, glycinate, or malate are often preferred over magnesium oxide.
-
DIY & Natural Electrolyte Boosters:
- Coconut Water: A natural source of potassium, with some sodium and magnesium.
- Homemade Oral Rehydration Solution: A simple recipe typically involves water, salt, sugar, and sometimes baking soda or fruit juice (for potassium). Many recipes are available from reputable health organizations.
- Infused Waters: Adding slices of cucumber, lemon, lime, or berries to water can impart small amounts of minerals and enhance flavor, encouraging more consistent hydration. A pinch of sea salt can also be added.
- Bone Broth: Rich in sodium, potassium, calcium, magnesium, and other minerals, making it an excellent hydrating and nourishing option, particularly during illness or recovery.
-
Listen to Your Body and Seek Professional Advice:
The body provides subtle cues. Beyond thirst, watch for fatigue, muscle cramps, dizziness, or changes in urine color (darker urine often indicates dehydration). However, self-diagnosis and indiscriminate supplementation can be risky.- Hyponatremia (Water Intoxication): Over-consuming plain water without replacing lost electrolytes, particularly during intense physical activity, can dilute sodium levels to dangerously low levels. This is a medical emergency.
- Hyperkalemia (High Potassium): While rare from diet alone, excessive potassium supplementation can be dangerous, especially for individuals with kidney issues, leading to cardiac arrhythmias.
- Hypermagnesemia (High Magnesium): Though less common, extremely high doses of magnesium can lead to diarrhea, nausea, and in severe cases, cardiac issues.
Always consult a healthcare professional or a registered dietitian if you have underlying health conditions, are on medications, or are considering significant changes to your hydration or supplementation strategy. They can assess your individual needs and guide you safely.
Conclusion: The Intelligent Approach to Hydration
The persistent, debilitating dehydration headache serves as a potent reminder that our understanding of hydration needs an upgrade. Moving "beyond water" is not about abandoning the most fundamental fluid of life, but rather about appreciating the intricate physiological ballet that water orchestrates, a dance choreographed by electrolytes.
The story of the dehydration headache is a narrative of imbalance: brain cells stressed by osmotic shifts, blood vessels struggling to maintain flow, and neurons misfiring due to ionic disruption. By recognizing the critical roles of sodium, potassium, magnesium, and other charged minerals, we empower ourselves to move from reactive pain management to proactive prevention.
For the knowledgeable individual, this isn’t just about avoiding discomfort; it’s about optimizing cellular function, enhancing cognitive clarity, and supporting overall well-being. Whether through strategic dietary choices, judicious use of supplements, or simply a more mindful approach to fluid intake in specific circumstances, embracing the full spectrum of electrolyte balance is the intelligent approach to truly preventing dehydration headaches. Listen to your body, respect its complex chemistry, and provide it with the full array of elements it needs to thrive – far beyond just a glass of plain water.