Blood Volume Drop: The Vascular Reason Your Thirst Leads to Throbbing
The sun beats down, a relentless hammer on the earth. You’ve been active, perhaps hiking a challenging trail, pushing through a demanding workout, or simply caught up in a busy day, forgetting to reach for your water bottle. A subtle dryness starts in your mouth, a whisper of thirst. It grows, demanding attention, evolving into a nagging sensation that tugs at your consciousness. Then, it happens: a dull ache begins behind your eyes, a low thrum that gradually intensifies, becoming a rhythmic, insistent throbbing. Each beat of your heart seems to echo in your temples, a drumbeat of discomfort.
This isn’t just a random headache; it’s a profound, physiological dialogue between your body and its most fundamental fluid. It’s the vascular reason your thirst can lead to that unsettling throbbing, a testament to the intricate dance of homeostasis that governs your very existence. To understand this phenomenon, we must embark on a journey deep into the vascular landscape, exploring the delicate balance of fluid volume, the cunning mechanisms of the human body, and the often-overlooked signals it sends when that balance is disrupted.
The Foundation: Water, The Elixir of Life, and Its Compartments
At its core, life is a watery affair. Water constitutes a staggering 50-70% of an adult’s body weight, serving as the universal solvent, the medium for all biochemical reactions, and the transport system for nutrients, gases, and waste. This vital fluid isn’t a single, amorphous pool; it’s meticulously compartmentalized, each section maintaining a specific composition and volume, yet all interconnected.
We typically categorize body water into two major divisions:
- Intracellular Fluid (ICF): Approximately two-thirds of the total body water resides within the cells themselves. This is where the machinery of life operates, fueled by the precise ionic gradients maintained across cell membranes.
- Extracellular Fluid (ECF): The remaining one-third of total body water surrounds the cells. The ECF is further subdivided into:
- Interstitial Fluid: The fluid that bathes the cells directly, filling the spaces between them. It’s the immediate environment for nutrient exchange and waste removal.
- Intravascular Fluid (Plasma): This is the fluid component of blood, circulating within the vessels. It’s the dynamic medium that carries blood cells, proteins, hormones, and all the elements necessary for systemic transport.
For our story of thirst and throbbing, the intravascular fluid – the plasma volume – is our protagonist. It’s the direct determinant of your blood volume, and any significant drop here sends ripples throughout your entire physiological system.
The Genesis of Thirst: Osmolality vs. Volume
Thirst isn’t a singular sensation; it’s a sophisticated alarm system triggered by two primary stimuli, often working in concert:
-
Osmotic Thirst: This is the most common trigger. It arises when the concentration of solutes (like sodium) in your extracellular fluid increases. Imagine a crowded room: too many people (solutes) for the space (water). This increased osmolality pulls water out of cells, including the specialized osmoreceptor cells located in the circumventricular organs of the brain (specifically the organum vasculosum of the lamina terminalis, OVLT, and the subfornical organ, SFO). These neurons detect the cellular shrinkage caused by water loss and signal the hypothalamus, the brain’s master regulator, to initiate the sensation of thirst. Simultaneously, they stimulate the release of Antidiuretic Hormone (ADH), also known as vasopressin, from the posterior pituitary, which tells your kidneys to conserve water.
-
Hypovolemic Thirst: This occurs when there’s a significant reduction in overall blood volume, irrespective of changes in osmolality. This is a more urgent signal, often indicating substantial fluid loss (e.g., from hemorrhage, severe sweating, or prolonged dehydration). When blood volume drops, blood pressure falls. Baroreceptors, specialized pressure sensors located in the carotid arteries and aortic arch, detect this decrease. They relay this information to the brainstem, which, in turn, activates the sympathetic nervous system and the formidable Renin-Angiotensin-Aldosterone System (RAAS). Angiotensin II, a key hormone in the RAAS cascade, is a potent dipsogen (thirst stimulator) and a powerful vasoconstrictor, initiating a systemic response to restore both volume and pressure.
While osmotic thirst is often the first subtle cue, hypovolemic thirst, when severe, is a more visceral, demanding sensation, and it is this significant drop in blood volume that truly sets the stage for the vascular drama culminating in throbbing.
The Descent: From Hydrated to Hypovolemic
Let’s trace the path. You’ve been active, perhaps under a hot sun. Your body sweats to cool itself, a highly efficient thermoregulatory mechanism. But sweat isn’t just water; it also contains electrolytes, primarily sodium. Initially, the water loss might exceed solute loss, leading to a rise in plasma osmolality and the onset of osmotic thirst. You might feel a dry mouth, a general sense of fatigue.
However, if fluid intake doesn’t match output, the situation escalates. Continued sweating, inadequate drinking, or even conditions like vomiting or diarrhea can lead to a more substantial reduction in total body water, affecting all fluid compartments. Critically, the intravascular fluid volume begins to shrink. This is hypovolemia: a reduction in the circulating plasma volume.
The immediate consequences of hypovolemia are profound:
- Reduced Venous Return: Less blood flows back to the heart.
- Decreased Cardiac Preload: The heart has less blood to fill its chambers before contraction.
- Reduced Cardiac Output: The amount of blood pumped by the heart per minute decreases.
- Falling Blood Pressure: The systemic pressure exerted by blood against the arterial walls drops.
This falling blood pressure is the critical signal that triggers the body’s emergency response, a symphony of compensatory mechanisms designed to protect vital organs, especially the brain and heart, from inadequate perfusion.
The Body’s Emergency Response: A Symphony of Compensation
When blood volume drops and blood pressure falls, your body doesn’t just give up. It activates a highly sophisticated, multi-pronged defense system:
-
Neural Response: The Baroreflex:
- The baroreceptors, sensing the drop in pressure, immediately fire fewer impulses to the brainstem.
- This reduced signaling disinhibits the sympathetic nervous system, unleashing a torrent of activity.
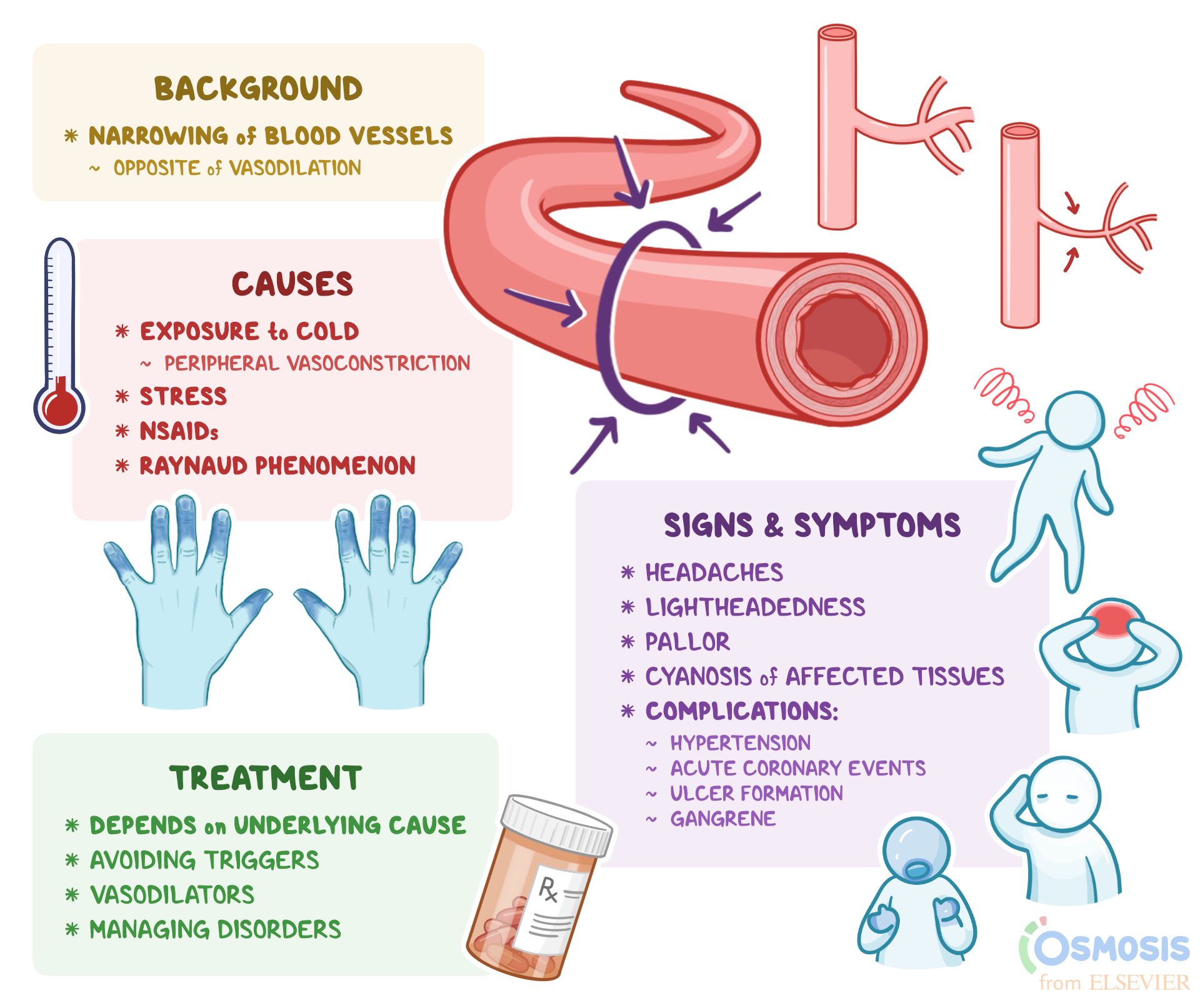
- Widespread Vasoconstriction: Sympathetic nerve fibers release norepinephrine, causing blood vessels in non-essential organs (skin, gut, kidneys, skeletal muscles) to constrict powerfully. This effectively "shunts" blood away from these areas and redirects it towards the critical organs: the brain and heart. This constriction helps to increase total peripheral resistance, thereby trying to maintain systemic blood pressure.
- Increased Heart Rate and Contractility: Sympathetic stimulation also directly acts on the heart, increasing its rate and the force of its contractions, attempting to pump more blood with each beat and increase cardiac output despite reduced preload.
-
Hormonal Response:
- Antidiuretic Hormone (ADH/Vasopressin): Already stimulated by increased osmolality, ADH release intensifies with hypovolemia. At higher concentrations, ADH is a potent vasoconstrictor, contributing to the systemic squeeze on blood vessels. Its primary role, however, remains to increase water reabsorption in the kidneys, conserving every precious drop.
- Renin-Angiotensin-Aldosterone System (RAAS): The kidneys, sensing reduced blood flow (due to sympathetic constriction of renal arteries and reduced systemic pressure), release renin. Renin initiates a cascade that ultimately produces Angiotensin II. As mentioned, Angiotensin II is a powerful vasoconstrictor, raising systemic vascular resistance. It also stimulates the adrenal glands to release aldosterone, which promotes sodium (and thus water) reabsorption in the kidneys, further boosting blood volume.
- Adrenaline (Epinephrine) and Noradrenaline (Norepinephrine): The adrenal medulla, stimulated by the sympathetic nervous system, releases these catecholamines into the bloodstream, amplifying and prolonging the sympathetic effects – vasoconstriction, increased heart rate, and contractility.
These compensatory mechanisms are a marvel of physiological engineering, working tirelessly to maintain a semblance of normal blood pressure and ensure adequate blood flow to the brain and heart. But this fierce battle for equilibrium comes at a cost, particularly for the areas being deprived of blood, and it sets the stage for our throbbing sensation.
The Throbbing Connection: Where Vascular Stress Becomes Pain
Now we arrive at the heart of the mystery: why does a drop in blood volume, coupled with the body’s compensatory mechanisms, lead to that distinctive, often pulsatile, throbbing headache? The answer is multifaceted, involving a complex interplay of vascular changes, neural signaling, and inflammatory mediators.
-
Cerebral Autoregulation and Its Limits:
- The brain is incredibly protective of its blood supply. It has a remarkable system called cerebral autoregulation, which allows cerebral blood vessels to constrict or dilate to maintain a relatively constant blood flow across a wide range of systemic blood pressures.
- When systemic blood pressure drops due to hypovolemia, cerebral vessels should dilate to maintain flow. However, severe dehydration and hypovolemia push this system to its limits.
- The overall systemic vasoconstriction driven by the sympathetic nervous system and Angiotensin II is designed to raise central blood pressure. But this can create a delicate balance: while peripheral vessels are squeezed, the brain’s vessels are trying to maintain flow.
-
The Brain Shrinks, Meninges Stretch:
- One direct consequence of severe dehydration is a loss of fluid not just from the bloodstream, but also from the interstitial fluid surrounding brain cells and even from the brain cells themselves.
- This can lead to a slight shrinkage of the brain parenchyma. The brain floats within the cerebrospinal fluid (CSF) inside the rigid skull, anchored by pain-sensitive structures called meninges (the dura mater, arachnoid mater, and pia mater).
- When the brain shrinks, it can pull on these meningeal membranes and the blood vessels embedded within them. These structures are richly innervated by pain receptors, and their stretching or traction is a well-known cause of headaches, often described as dull or aching.
-
Vascular Dilation and Rebound Phenomenon:
- This is arguably the most critical component of the throbbing sensation. While the body initiates widespread vasoconstriction to raise overall blood pressure, the brain’s attempt to maintain its own blood flow, or even a localized response to metabolic stress, can lead to cerebral vasodilation.
- Metabolic Byproducts: Reduced blood flow, even transiently, can lead to the accumulation of metabolic byproducts (like adenosine, CO2, lactate) in the brain tissue. These are potent local vasodilators, signaling to the local vessels to open up and increase blood flow.
- Rebound Effect: Imagine a tightly squeezed hose that is suddenly released. The intense systemic vasoconstriction in response to hypovolemia can be followed by a relative rebound vasodilation once the initial compensatory efforts wane, or as the body struggles to maintain perfusion. This is particularly true if the dehydration is prolonged or if there’s an uneven restoration of fluid.
- Pulsatile Flow: When blood vessels, particularly arteries, are dilated, the pulsatile nature of blood flow becomes much more pronounced. Each beat of the heart sends a wave of pressure through these widened vessels. If these vessels are stretched, inflamed, or if their surrounding pain receptors are sensitized, this pulsatile pressure wave is perceived as a throbbing pain. It’s like hearing a bass drum reverberate more intensely in a large, empty hall than in a small, cluttered room.
-
Inflammation and Neurovascular Activation:
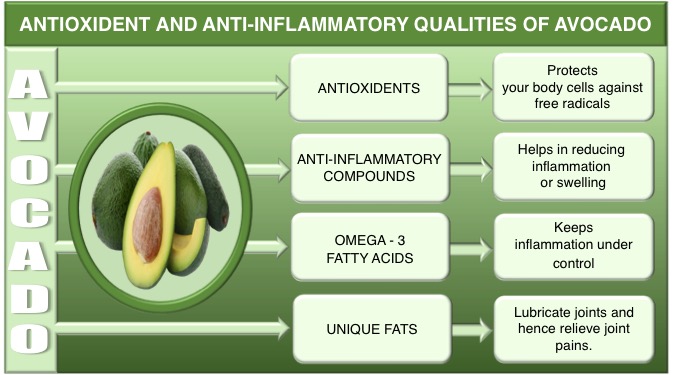
- Dehydration is a stressor. Stress, especially physiological stress, can trigger the release of inflammatory mediators and neuropeptides.
- Prostaglandins, Bradykinin: These substances are known to sensitize pain receptors and promote vasodilation.
- Calcitonin Gene-Related Peptide (CGRP): This neuropeptide is heavily implicated in migraine headaches. It’s released from trigeminal nerve endings and is a potent vasodilator and neurogenic inflammatory agent. While not a full-blown migraine, dehydration-induced headaches share some common pathways, and CGRP release could contribute to the throbbing and pain sensitization.
- The combination of stretched meninges, dilated blood vessels, and inflammatory soup creates a perfect storm for pain generation. The pain receptors in the vessel walls and surrounding tissues become hypersensitive, making the normal pulsatile flow of blood feel like a painful throb.
-
Autonomic Nervous System Imbalance:
- The intense sympathetic activation in response to hypovolemia, followed by potential shifts as the body tries to re-establish balance, can create a state of autonomic dysregulation. This imbalance can affect vascular tone and pain perception throughout the body, not just in the head. Some individuals report a general sense of "throbbing" or heightened awareness of their pulse in various parts of their body during severe dehydration.
In essence, the throbbing headache of dehydration is a complex interplay: the brain physically shrinks, tugging on pain-sensitive structures; its blood vessels attempt to dilate to maintain flow, sometimes in a compensatory or rebound manner against systemic constriction; and inflammatory signals amplify the perception of pain, making the normal pulsatile flow of blood feel like a relentless hammering.
The Restoration: Quenching the Thirst, Calming the Throb
The immediate antidote to this vascular turmoil is, unsurprisingly, rehydration. When you drink water, a series of events begins to reverse the dehydration cascade:
- Oral-Pharyngeal Receptors: The act of drinking itself provides immediate, though temporary, relief from thirst signals, even before the fluid has been absorbed.
- Gastric Distention: As water fills the stomach, stretch receptors send signals to the brain, further reducing thirst.
- Fluid Absorption: Water is rapidly absorbed from the gastrointestinal tract into the bloodstream.
- Normalization of Osmolality and Volume: As plasma volume increases and osmolality decreases, the osmoreceptors and baroreceptors return to their baseline activity.
- Suppression of Compensatory Mechanisms: ADH release diminishes, the RAAS is deactivated, and sympathetic nervous system activity subsides. The widespread vasoconstriction lessens.
- Vascular Normalization: As blood volume stabilizes and systemic blood pressure normalizes, the exaggerated vasodilation in the brain or the rebound effects diminish. The inflammatory mediators are cleared, and pain receptor sensitization reduces.
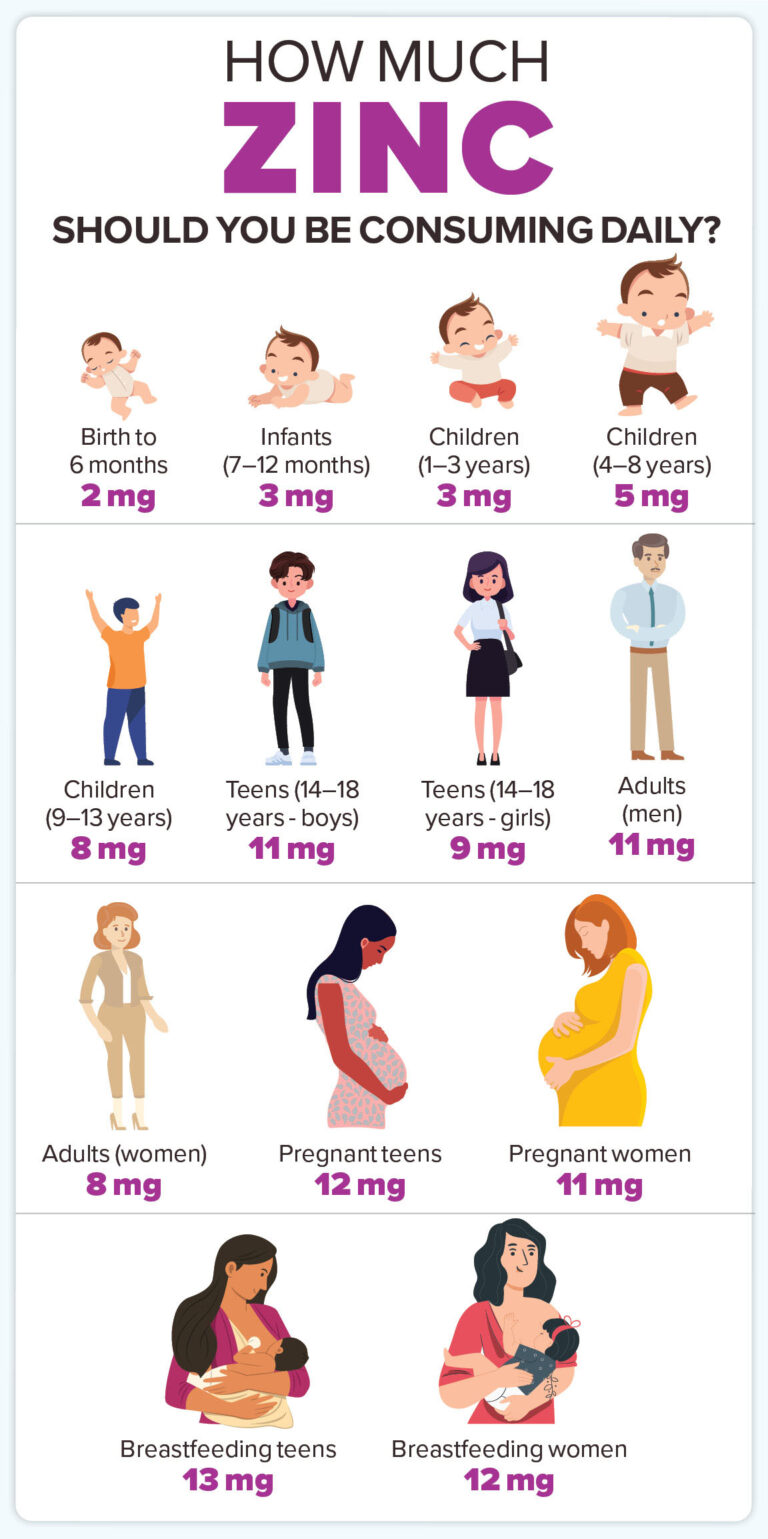
Slowly, the throbbing recedes, replaced by a sense of relief and renewed vitality. However, for severe dehydration, simply drinking plain water might not be enough. Electrolytes, especially sodium, are crucial for retaining water in the appropriate compartments. Without them, rapid ingestion of large amounts of plain water can dilute existing electrolytes, potentially leading to hyponatremia, a dangerous condition. This is why electrolyte-rich fluids or oral rehydration solutions are often recommended for more significant fluid deficits.
Broader Implications: Beyond the Headache
Understanding the vascular reasons behind dehydration’s throbbing extends beyond a simple headache. It illuminates the fundamental principles of fluid balance that underpin numerous physiological and pathological states:
- Orthostatic Hypotension: This common condition, where blood pressure drops upon standing, is often exacerbated by hypovolemia or impaired baroreflex function. The body struggles to shunt blood upwards against gravity when volume is low.
- Hypertension: Chronic fluid retention and dysregulation of the RAAS are central to many forms of hypertension. The constant struggle to manage blood volume directly impacts arterial pressure.
- Heart Failure: In heart failure, the heart’s ability to pump blood is compromised. Managing fluid volume – ensuring adequate preload without causing volume overload – is a critical therapeutic challenge.
- Kidney Disease: The kidneys are the ultimate arbiters of fluid and electrolyte balance. Impaired kidney function directly leads to profound disturbances in blood volume, with consequences ranging from edema to severe dehydration.
- Migraine Triggers: Dehydration is a well-established trigger for migraines, a primary headache disorder characterized by severe, throbbing pain, often associated with vascular changes and neurogenic inflammation. The mechanisms discussed here – cerebral vasodilation, neurogenic inflammation, and pain sensitization – directly overlap with proposed migraine pathophysiology. This connection suggests that even mild dehydration can push susceptible individuals towards a full-blown migraine attack.
- Medication Effects: Diuretics (which increase urine output), ACE inhibitors, and ARBs (which interfere with the RAAS) are commonly prescribed medications that directly impact fluid volume and blood pressure. Their side effects and therapeutic actions are deeply intertwined with the body’s homeostatic mechanisms for blood volume.
Conclusion: A Silent Dialogue
The throbbing headache that accompanies intense thirst is far more than a nuisance; it is a profound and eloquent communication from your body. It is a testament to the relentless, intricate work of your vascular system, struggling to maintain equilibrium in the face of dwindling resources. It’s the sound of your blood vessels, normally silent partners in your existence, screaming for attention, their rhythmic contractions and dilations amplified into a painful drumbeat.
It reminds us that the simple act of drinking water is not merely quenching a fleeting desire, but a vital intervention that supports a complex ballet of physiological processes. The next time you feel that dry mouth, that nagging thirst, and especially that rhythmic throb behind your eyes, take a moment to appreciate the incredible, invisible struggle unfolding within you. Listen to your body’s silent dialogue, and respond to its most fundamental plea. Hydrate, and restore the harmonious flow of life.