Is It Thirst or Tension? How to Tell if Your Headache is Caused by Dehydration
It’s a familiar scenario: a dull throb behind the eyes, a persistent ache that tightens around the temples, or a pervasive pressure that seems to cloud your thoughts. A headache. For many, it’s an unwelcome daily or weekly visitor, a disruption to concentration, productivity, and peace of mind. But what is its root cause? Is it the insidious creep of stress, knotting muscles and tightening nerves, or a more fundamental, yet often overlooked, physiological plea from your body: a desperate cry for water?
In a world that constantly bombards us with stimuli, deadlines, and digital screens, distinguishing between the myriad triggers of a headache can feel like deciphering an ancient riddle. Yet, for two of the most common culprits – dehydration and tension – the clues are often there, subtle yet significant, waiting for a discerning eye to connect them. Understanding these distinctions isn’t just an academic exercise; it’s an act of self-care, empowering us to respond effectively and reclaim our comfort.
This isn’t merely a guide; it’s an exploration, a journey into the intricate workings of our bodies, a story of how fluid balance and stress manifest as pain. We will delve deep into the physiological mechanisms, the tell-tale symptoms, and the often-blurred lines that make this diagnostic puzzle so compelling. Our audience, already knowledgeable and keen to understand the nuances of their own health, will appreciate a detailed look at the ‘why’ behind the ‘what,’ moving beyond superficial remedies to a profound understanding of their body’s signals.
The Dehydration Headache: A Silent Plea for Water
Imagine your brain, a magnificent organ comprising approximately 75% water, suspended delicately within your skull, cushioned by cerebrospinal fluid. Now, picture what happens when that vital fluid balance is disturbed. When you become dehydrated, your body begins to ration its water supply, drawing fluid from less critical areas to maintain essential functions. Unfortunately, the brain is not immune to this process.
The Physiological Mechanism: The Brain’s Shrinking Act
At a cellular level, dehydration leads to a reduction in the volume of water within the cells, including those of the brain. This phenomenon, known as cellular shrinkage, is driven by osmotic pressure. When the concentration of solutes (like sodium) in the blood increases due to insufficient water intake, water is drawn out of brain cells to try and equalize the concentration.
This reduction in brain volume causes the brain tissue to pull away slightly from the meninges – the sensitive membranes that line the skull and protect the brain. These meninges are rich in pain receptors. Even a slight tug or strain on these pain-sensitive structures can trigger a headache.
Furthermore, dehydration can lead to a decrease in overall blood volume, affecting cerebral blood flow. To compensate, the body may try to dilate blood vessels in the brain, which can also contribute to throbbing pain. The blood itself thickens slightly, making it harder for the heart to pump and reducing oxygen delivery to tissues, which can further exacerbate headache symptoms.
Another crucial player is the body’s electrolyte balance. Water is intrinsically linked with electrolytes like sodium, potassium, and magnesium. Dehydration often accompanies an imbalance in these vital minerals, which are essential for nerve function, muscle contraction, and maintaining fluid balance. Disruptions in these delicate balances can directly impact neurological function and contribute to headache pain.
The body’s natural response to dehydration also involves the release of certain hormones, such as vasopressin (also known as antidiuretic hormone, or ADH), which signals the kidneys to conserve water. While essential for survival, the systemic effects of these hormonal shifts can influence blood pressure and blood vessel tone, indirectly contributing to headache sensation.
The Narrative of Symptoms: Reading the Body’s Language
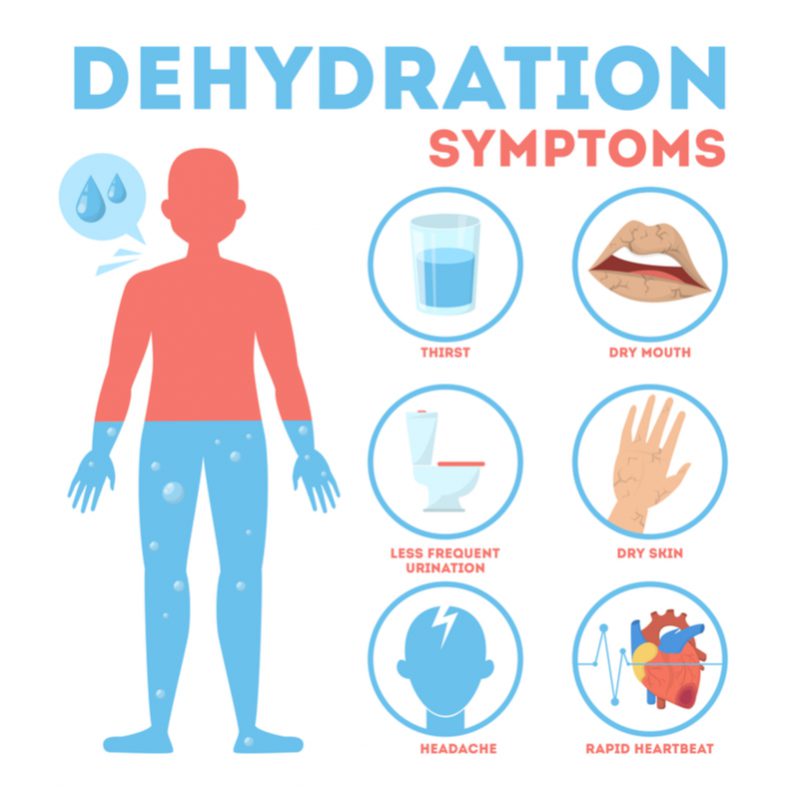
The dehydration headache often tells a distinct story through its symptoms:
- Type of Pain: Typically described as a dull ache or a throbbing sensation. It’s not usually sharp or stabbing.
- Location: Often felt across the forehead, temples, or even all over the head. It can sometimes be more pronounced on one side, but often feels diffuse.
- Accompanying Symptoms: This is where the story truly unfolds. Dehydration headaches are rarely isolated. They are usually accompanied by other signs that scream "I need water!"
- Thirst: The most obvious clue. A persistent, undeniable dryness in the mouth and throat.
- Fatigue and Lethargy: Feeling unusually tired, sluggish, and lacking energy. The brain is literally struggling to perform at optimal levels.
- Reduced Urination and Dark Urine: Your kidneys are working overtime to conserve water, leading to less frequent bathroom trips and urine that is concentrated and darker than usual.
- Dry Mouth and Sticky Saliva: A classic sign of insufficient fluid.
- Dizziness or Lightheadedness: Especially when standing up quickly, due to reduced blood volume and subsequent drop in blood pressure.
- Decreased Skin Turgor: Pinching the skin on the back of your hand and observing how quickly it returns to normal. Slow return indicates dehydration.
- Muscle Cramps: Electrolyte imbalances can lead to involuntary muscle contractions.
- Impaired Cognitive Function: Difficulty concentrating, irritability, and a general feeling of mental fogginess.
The Timeline and Triggers:
Dehydration headaches often develop gradually. They might start subtly after a period of inadequate fluid intake (e.g., a busy workday without water breaks, a long flight, intense exercise without rehydration). They can also be triggered by excessive fluid loss through sweating (exercise, hot weather), vomiting, diarrhea, or increased urination (due to certain medications or conditions). Alcohol consumption is a notorious dehydrator and a common precursor to dehydration headaches (the "hangover" headache is largely a dehydration headache).
The Tension Headache: The Body’s Knotted Response
In stark contrast to the fluid dynamics of dehydration, the tension headache tells a story of physical and emotional strain, a narrative woven from stress, posture, and muscle constriction. It is the most common type of headache, affecting millions globally, and its origins lie more in the musculoskeletal and nervous systems.
The Physiological Mechanism: Muscles, Nerves, and Stress
The primary theory behind tension headaches involves the contraction of muscles in the head, neck, and shoulders. When these muscles remain tensed for prolonged periods – often in response to stress, poor posture (e.g., hunching over a computer), or jaw clenching – they can become fatigued, leading to pain and discomfort. These chronically contracted muscles can also create trigger points, areas of localized tenderness that can refer pain to other parts of the head.
Beyond muscle contraction, the nervous system plays a critical role. Stress, anxiety, and even depression can alter the body’s pain perception pathways. Neurotransmitters, the chemical messengers in the brain, such as serotonin and norepinephrine, are often implicated in the modulation of pain. Imbalances or dysregulation of these neurotransmitters can lower the pain threshold, making individuals more susceptible to headaches.
The trigeminal nerve system, a complex network responsible for sensation in the face and motor functions like chewing, is also a key player. Chronic muscle tension and stress can sensitize the trigeminal nerve and its connections to the upper cervical spine (the neck), leading to a phenomenon known as central sensitization, where the brain becomes hypersensitive to pain signals. This means even minor stimuli can be perceived as significant pain.
Inflammation, albeit often low-grade, can also contribute. Sustained muscle contraction can reduce blood flow to the affected tissues, leading to a buildup of metabolic byproducts and localized inflammation, which irritates nerve endings and contributes to pain.
The Narrative of Symptoms: A Vise Around the Skull
The tension headache’s narrative is characterized by specific patterns:
- Type of Pain: Often described as a constant, dull pressure or tightness, like a band tightening around the head or a vise squeezing the skull. It’s typically non-throbbing, unlike the pulsatile nature of a dehydration headache or migraine.
- Location: Commonly felt on both sides of the head (bilateral), often starting in the back of the head or neck and spreading forward to the temples and forehead. It can also manifest as pressure behind the eyes.
- Accompanying Symptoms: Unlike dehydration headaches, tension headaches usually lack systemic symptoms like thirst or dizziness. However, they are often accompanied by:
- Tenderness: Scalp, neck, and shoulder muscles often feel tender to the touch.
- Stiffness: A feeling of stiffness or limited range of motion in the neck.
- Irritability: Due to the persistent discomfort.
- Sensitivity to light or sound (mild): While not as severe as with migraines, some people with tension headaches may experience a slight aversion to bright lights or loud noises.
- No Nausea or Vomiting: This is a key differentiator from migraines.
The Timeline and Triggers:
Tension headaches can be episodic (occurring occasionally) or chronic (occurring 15 or more days a month for at least three months). They are strongly linked to:
- Stress and Anxiety: Emotional strain is a primary trigger.
- Poor Posture: Hunching over computers, phones, or prolonged awkward positions.
- Lack of Sleep: Insufficient rest can exacerbate muscle tension and lower pain thresholds.
- Eyestrain: Prolonged focus on screens or reading in poor light.
- Jaw Clenching (Bruxism): Often stress-related, leading to tension in the temporomandibular joint (TMJ) and surrounding muscles.
- Hunger: While hunger can also lead to dehydration, the mechanism for a hunger-related tension headache is often related to blood sugar drops and general systemic stress.
The Crucial Distinction: Unraveling the Clues
While both types of headaches bring discomfort, their distinct narratives offer crucial clues for differentiation. Let’s compare their stories side-by-side:
| Feature | Dehydration Headache | Tension Headache |
|---|---|---|
| Type of Pain | Dull ache, throbbing, pulsating | Constant pressure, tightness, band-like |
| Location | Often diffuse, frontal, temples, or all over | Bilateral, band around the head, neck/shoulder origin |
| Severity | Mild to moderate | Mild to moderate (can be severe in chronic cases) |
| Accompanying | Thirst, dry mouth, fatigue, dark urine, dizziness, | Neck/shoulder stiffness, muscle tenderness, irritability |
| Symptoms | reduced urination, lightheadedness, decreased focus | |
| Nausea/Vomiting | Rare | Absent |
| Light/Sound | Mild sensitivity possible | Mild sensitivity possible |
| Triggers | Inadequate fluid intake, exercise, heat, alcohol, | Stress, anxiety, poor posture, lack of sleep, eyestrain |
| vomiting, diarrhea | ||
| Relief | Drinking water/electrolytes, rest | OTC pain relievers, stress reduction, massage, heat/cold |
| Onset | Gradual | Gradual, often builds over time |
The presence of thirst, dry mouth, and changes in urine color are powerful indicators pointing towards dehydration. Conversely, a headache accompanied by palpable muscle tension in the neck and shoulders, without significant thirst, strongly suggests a tension headache.
The Body’s Intricate Symphony: The Deeper Science of Hydration
To truly appreciate the impact of dehydration, one must understand the body not just as a collection of organs, but as a meticulously orchestrated symphony of physiological processes, where water is the conductor.
Fluid Compartments and Osmosis:
Our bodies are approximately 60% water, distributed across various compartments:
- Intracellular Fluid (ICF): Water within the cells (about two-thirds of total body water).
- Extracellular Fluid (ECF): Water outside the cells (about one-third), further divided into:
- Interstitial Fluid: Surrounding cells.
- Plasma: The fluid component of blood.
- Transcellular Fluid: Cerebrospinal fluid, synovial fluid, etc.
The movement of water between these compartments is governed by osmosis, the movement of water across a semipermeable membrane from an area of lower solute concentration to an area of higher solute concentration. When we are dehydrated, the ECF becomes hypertonic (higher solute concentration). This draws water out of the ICF, leading to cellular dehydration and shrinkage, particularly noticeable in brain cells.
Electrolytes: The Unsung Heroes:
Electrolytes (sodium, potassium, chloride, magnesium, calcium) are minerals that carry an electric charge when dissolved in water. They are absolutely critical for:
- Nerve Impulse Transmission: Essential for brain function, muscle contraction, and heart rhythm.
- Fluid Balance: Sodium, in particular, is the primary determinant of ECF volume and osmolality.
- Muscle Function: Calcium and potassium are vital for muscle contraction and relaxation.
- pH Balance: Maintaining the body’s acid-base equilibrium.
Dehydration often leads to electrolyte imbalances, especially hyponatremia (low sodium) if excessive plain water is consumed rapidly after severe dehydration, or hypernatremia (high sodium) if water loss exceeds sodium loss. Both can cause severe neurological symptoms, including headaches, confusion, and seizures.
Hormonal Regulation: A Masterpiece of Feedback Loops:
The body has sophisticated mechanisms to regulate fluid balance:
- Antidiuretic Hormone (ADH) / Vasopressin: Released by the posterior pituitary gland in response to increased plasma osmolality (dehydration) or decreased blood volume. ADH increases water reabsorption in the kidneys, conserving fluid.
- Renin-Angiotensin-Aldosterone System (RAAS): Activated by decreased blood pressure or blood volume. Renin leads to the production of angiotensin II, which constricts blood vessels and stimulates aldosterone release. Aldosterone promotes sodium and water reabsorption in the kidneys.
- Thirst Mechanism: The hypothalamus in the brain senses changes in osmolality and blood volume, triggering the sensation of thirst, a direct command to rehydrate.
When these systems are constantly stressed by inadequate fluid intake, their efficiency can be compromised, leading to a cascade of physiological disturbances that contribute to headache pain and overall malaise.
The Overlap and the Shadow Zones: When the Lines Blur
Life, however, is rarely a neat dichotomy. The human body is a complex system, and sometimes the narratives of thirst and tension intertwine, creating a blurred landscape where discerning the primary cause becomes more challenging.
Consider a scenario: a demanding project at work leads to prolonged screen time (eyestrain), poor posture (neck tension), skipped meals (blood sugar dip), and forgetting to drink water (dehydration). In this instance, the headache experienced might be a multifactorial beast, exhibiting characteristics of both dehydration and tension. The underlying tension might be exacerbated by the body’s generalized stress response to dehydration, or vice-versa.
- Stress-Induced Dehydration: Chronic stress can lead to shallow breathing, increased perspiration, and simply forgetting to drink water. The physiological effects of stress (cortisol release, sympathetic nervous system activation) can also independently trigger headaches.
- Dehydration Exacerbating Tension: A body operating in a dehydrated state is less resilient. Muscles are more prone to cramping and stiffness, making them more susceptible to tension and less able to recover from sustained contraction. The brain’s reduced fluid volume might also make it more sensitive to pain signals, amplifying a pre-existing tension headache.
- Caffeine Withdrawal: Many individuals consume caffeine, a diuretic. Sudden cessation can lead to both dehydration (due to previous diuretic effect) and withdrawal symptoms, including headaches, which often mimic tension headaches but can also have throbbing qualities.
In these "shadow zones," a holistic assessment of recent activities, diet, sleep patterns, and emotional state becomes paramount. It’s not always about finding the single cause, but understanding the contributing factors and addressing them systematically.
Beyond Plain Water: A Holistic Approach to Hydration
While water is the cornerstone of hydration, a truly knowledgeable approach recognizes that sometimes, especially after significant fluid loss, more is needed.
- Electrolyte-Rich Fluids: For intense exercise, prolonged heat exposure, or illness involving vomiting/diarrhea, plain water alone might not be sufficient. Electrolyte-rich beverages (sports drinks, coconut water, oral rehydration solutions) can help replenish lost sodium, potassium, and other vital minerals, preventing further imbalance. However, for everyday hydration, these are often unnecessary and can contain excessive sugar.
- Fruits and Vegetables: Many fruits and vegetables are excellent sources of water and electrolytes. Watermelon, cucumber, oranges, strawberries, and leafy greens contribute significantly to daily fluid intake and provide essential vitamins and minerals.
- Mindful Consumption: Be aware of diuretics like excessive caffeine and alcohol, which increase urine output and can lead to dehydration. Moderate their intake, especially when already feeling unwell.
For the knowledgeable audience, consider the concept of osmolality in beverages.
- Hypotonic solutions (lower solute concentration than body fluids, like plain water) are absorbed quickly but might dilute existing electrolytes if consumed in large quantities without repletion.
- Isotonic solutions (similar solute concentration, like many sports drinks) are generally well-absorbed and replace both water and electrolytes effectively.
- Hypertonic solutions (higher solute concentration, like sugary sodas) can actually draw water into the gut from the bloodstream, potentially worsening dehydration in the short term.
Proactive Strategies: Preventing the Ache
The best defense against both dehydration and tension headaches is a proactive, mindful approach to daily living.
-
Consistent Hydration:
- Carry a water bottle and sip throughout the day.
- Set reminders on your phone or computer to drink water.
- Start and end your day with a glass of water.
- Adjust intake based on activity level, climate, and health status. Aim for clear or pale yellow urine.
-
Mindful Stress Management:
- Incorporate relaxation techniques: deep breathing, meditation, yoga, mindfulness.
- Prioritize sleep: Aim for 7-9 hours of quality sleep per night.
- Engage in regular physical activity: Exercise is a potent stress reliever.
- Learn to say no: Manage your commitments to avoid overwhelm.
-
Ergonomics and Posture:
- Ensure your workstation is set up ergonomically to minimize neck and shoulder strain.
- Take frequent breaks to stretch and move, especially if you have a sedentary job.
- Be mindful of your posture throughout the day, whether sitting, standing, or using electronic devices.
-
Balanced Nutrition:
- Eat regular, balanced meals to maintain stable blood sugar levels.
- Include plenty of fruits and vegetables for hydration and essential nutrients.
-
Listen to Your Body: Pay attention to early warning signs of thirst, fatigue, or muscle tension. Addressing these proactively can often prevent a full-blown headache.
When to Seek Professional Guidance: Red Flags and the Unseen
While most headaches are benign, some can signal more serious underlying conditions. A knowledgeable individual understands the importance of recognizing red flags and seeking timely medical attention.
Consult a healthcare professional if you experience:
- Sudden, severe headache (thunderclap headache): This can be a sign of a stroke, aneurysm, or hemorrhage.
- Headache accompanied by neurological symptoms: Weakness, numbness, vision changes, difficulty speaking, confusion, loss of balance.
- Headache with fever, stiff neck, rash: Could indicate meningitis or encephalitis.
- Headache after a head injury: Especially if it worsens or is accompanied by other symptoms.
- Headache that is new or different from your usual headaches, especially if you are over 50.
- Chronic headaches that are worsening or unresponsive to typical remedies.
- Headaches that interfere significantly with daily life.
- Headaches with pain around the eye or ear.
These symptoms require immediate medical evaluation. Even in less dramatic cases, if your headaches are frequent, severe, or significantly impacting your quality of life, a doctor can help diagnose the specific type of headache and recommend appropriate management strategies, which might include lifestyle changes, medication, or specialist referrals.
Conclusion: The Power of Deciphering Your Body’s Story
The journey to understanding our headaches is ultimately a journey of self-awareness. It’s about tuning into the subtle whispers of our bodies before they escalate into urgent shouts. The narrative of a dehydration headache is one of fluid imbalance, a simple yet profound plea for replenishment. The story of a tension headache is one of accumulated stress, physical strain, and nervous system overload.
For the knowledgeable individual, this distinction isn’t just about symptom matching; it’s about appreciating the intricate physiological dance occurring within. It’s about recognizing that every ache, every throb, is a piece of a larger story your body is trying to tell you. By learning to differentiate between the parched cry for water and the knotted plea for release, we empower ourselves with the ability to respond not with guesswork, but with informed intention.
In a world that often encourages us to push through discomfort, to ignore the signals, let us choose instead to listen. Let us choose to understand. For in understanding, we find the path not just to temporary relief, but to sustained well-being, where the clarity of thought and the comfort of the body can once again harmonize, free from the shadow of the mysterious ache. The power to decipher this story lies within each of us, waiting to be activated by knowledge and mindful attention.