Stress Less, Ache Less: Reclaiming Agency from the Grip of Chronic Headaches Through Mind-Body Synergy
The silent epidemic of chronic headaches is a pervasive and often debilitating force, a shadow cast over millions of lives. For those ensnared in its relentless grip, the world can shrink, defined by the ebb and flow of pulsating pain, the constant search for relief, and the gnawing frustration of traditional treatments that too often fall short. It’s a journey marked by canceled plans, missed opportunities, and the quiet despair of an invisible illness. Yet, within this landscape of suffering, a profound shift is underway – a revolution in understanding that acknowledges the intricate, inseparable dance between mind and body. This is the story of how that understanding is paving the way for a new paradigm of healing, empowering individuals to move from passive recipients of pain to active architects of their own well-being, leveraging the potent tools of mind-body medicine to "Stress Less, Ache Less."
For centuries, medical science largely approached chronic pain, including headaches, through a reductionist lens. The focus was on identifying a singular physiological anomaly – a structural issue, a chemical imbalance – and targeting it with medication or intervention. While undeniably crucial for acute conditions, this approach often overlooks the profound complexity of chronic pain, which is rarely a simple cause-and-effect equation. The patient suffering from daily migraines or tension headaches, whose scans reveal no overt pathology, is often left feeling unheard, dismissed, and increasingly hopeless. Their pain, though invisible to the diagnostic tools, is undeniably real, deeply personal, and profoundly impactful.
The narrative begins to change when we acknowledge the brain as the ultimate interpreter of pain, and the nervous system as a dynamic, adaptable entity constantly communicating with every cell in the body. Stress, in its myriad forms – emotional, psychological, physical – is not merely a trigger for headaches; it is a fundamental player in their chronification. It acts as an amplifier, turning the volume up on existing pain pathways and even creating new ones. The relentless cycle of stress leading to pain, and pain leading to more stress, is a cruel loop that traps individuals, diminishing their quality of life.
This is where the story of mind-body techniques truly takes flight. It’s a narrative of empowerment, of reconnecting with one’s innate capacity for self-regulation and healing. These techniques are not a panacea, nor are they a dismissal of physiological pain. Instead, they represent a sophisticated, evidence-based approach to modulate the nervous system, reframe the experience of pain, and cultivate resilience against the insidious effects of stress. For the knowledgeable audience, the mechanisms are not mystical; they are rooted in neurobiology, psychology, and physiology, demonstrating how conscious intervention can profoundly alter unconscious bodily processes.
Understanding the Battlefield: The Neurobiology of Chronic Headaches and Stress
Before delving into the techniques, it’s crucial to appreciate the intricate physiological landscape they aim to influence. Chronic headaches, whether migraine, tension-type, or cluster, involve complex interactions within the central and peripheral nervous systems.
At the heart of this interaction lies the Hypothalamic-Pituitary-Adrenal (HPA) axis, the body’s central stress response system. When perceived threats (be they physical or psychological) activate the HPA axis, it releases cortisol and other stress hormones. While essential for acute survival, chronic activation leads to systemic inflammation, dysregulation of neurotransmitters (like serotonin, which plays a critical role in migraine), and increased sensitivity of pain pathways.
The autonomic nervous system (ANS), comprising the sympathetic ("fight or flight") and parasympathetic ("rest and digest") branches, is another key player. Chronic stress keeps the sympathetic nervous system in overdrive, leading to muscle tension (a hallmark of tension headaches), vasoconstriction (contributing to altered blood flow in migraines), and heightened sensory perception. Conversely, the parasympathetic nervous system, particularly the vagus nerve, is crucial for calming the body and reducing inflammation. Mind-body techniques often aim to enhance vagal tone, shifting the ANS towards a state of balance.
Perhaps most critically, chronic pain often involves central sensitization. This phenomenon occurs when the nervous system becomes "wound up," leading to an exaggerated response to stimuli that would normally not be painful. The pain threshold lowers, and non-painful stimuli can be perceived as painful. This neuroplastic change means that even after an initial injury or trigger has resolved, the brain continues to generate pain signals. Stress significantly contributes to and perpetuates central sensitization.
The good news, and the core of the mind-body story, is that this neuroplasticity can work both ways. The brain and nervous system are not static; they can be rewired. Mind-body techniques leverage this inherent adaptability to dial down the stress response, desensitize pain pathways, and foster a sense of control over one’s internal experience.
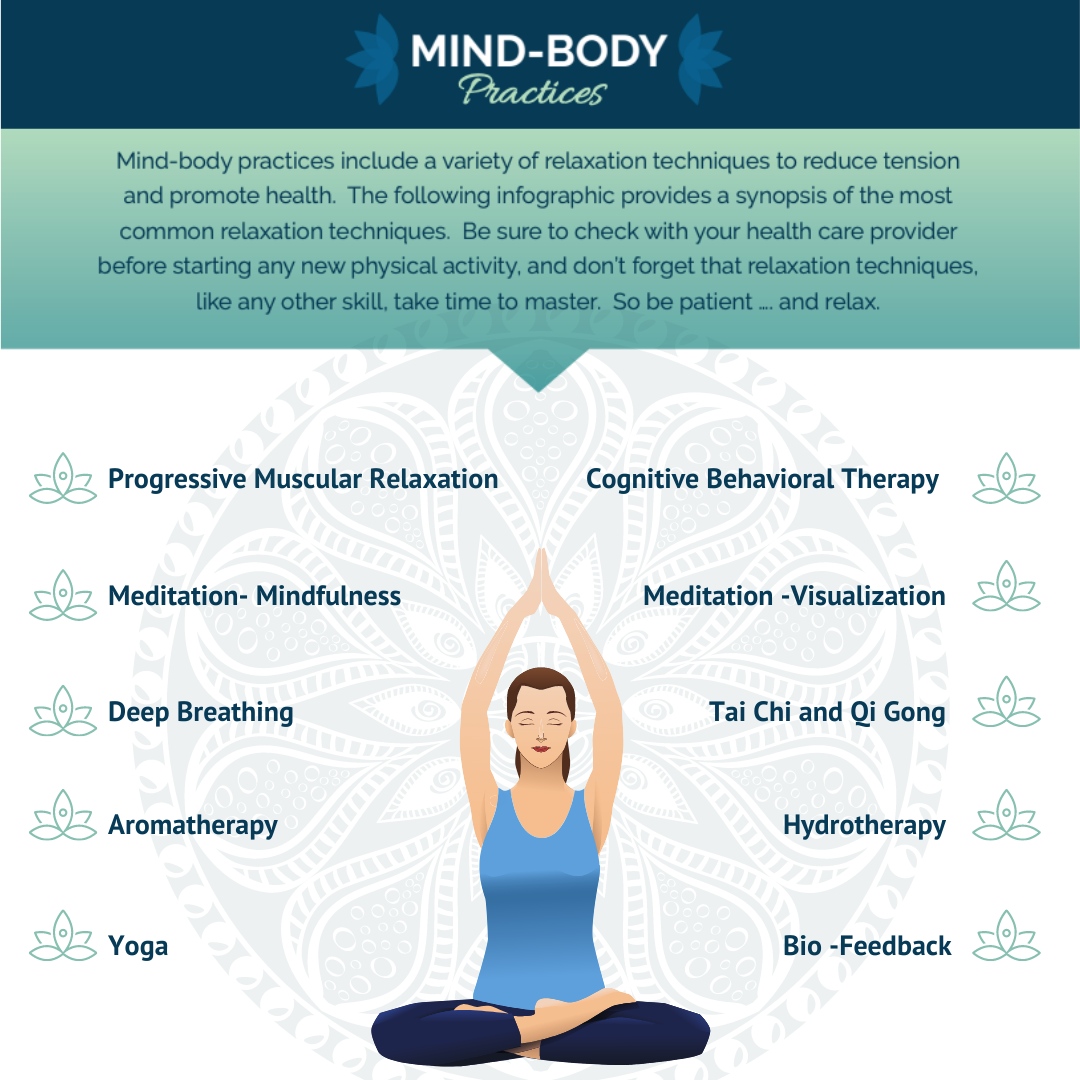
The Arsenal of Awareness: Core Mind-Body Techniques
The journey from chronic headache suffering to sustainable relief often involves building a personalized toolkit of mind-body practices. Each technique offers a unique pathway to influence the stress response, modulate pain, and cultivate resilience.
1. Mindfulness-Based Stress Reduction (MBSR)
The Practice: Originating from Jon Kabat-Zinn’s work, MBSR is a structured program that teaches participants to cultivate present-moment awareness, non-judgmentally observing thoughts, feelings, and bodily sensations. Key practices include the body scan, sitting meditation (focusing on breath), and mindful movement (e.g., gentle yoga).
The Mechanism: Mindfulness operates on multiple neurobiological fronts. It strengthens the prefrontal cortex (PFC), the brain’s executive control center, enhancing its ability to regulate the amygdala (the brain’s fear and stress center). This leads to a reduced fight-or-flight response and decreased production of stress hormones. Mindfulness also increases grey matter density in areas associated with attention and sensory processing, and improves interoception – the ability to sense internal bodily states. By fostering non-reactive awareness, individuals learn to observe headache pain without being consumed by it, breaking the cycle of fear and catastrophization that often amplifies suffering. The sustained focus on the breath also directly stimulates the vagus nerve, enhancing parasympathetic activity.
For Headaches: Research consistently demonstrates that MBSR can reduce headache frequency, intensity, and duration, particularly for chronic tension-type headaches and migraines. It improves coping mechanisms, reduces pain-related disability, and enhances overall quality of life. The ability to "surf the wave" of pain rather than being overwhelmed by it is a profound shift for many sufferers.
The Story Element: Mindfulness is about reclaiming the present moment from the tyranny of anticipated pain or past suffering. It’s about learning to be an observer of one’s experience rather than a prisoner to it, fostering a deep sense of inner calm amidst external or internal storms.
2. Biofeedback
The Practice: Biofeedback is a non-invasive technique that uses electronic sensors to provide real-time information about physiological functions normally outside conscious awareness, such as heart rate, muscle tension, skin temperature, or brainwave activity. With this feedback, individuals learn to consciously control these functions.
The Mechanism: Biofeedback operates on principles of operant conditioning. By seeing or hearing their physiological responses (e.g., muscle tension readings, skin temperature graphs), individuals learn which mental or physical strategies (e.g., deep breathing, relaxation imagery) can alter these responses. For headaches, common types include:
- Electromyography (EMG) Biofeedback: Measures muscle tension, particularly in the forehead, neck, and shoulders, which are often implicated in tension headaches and can exacerbate migraines. Learning to relax these muscles directly reduces a key pain source.
- Thermal Biofeedback: Measures skin temperature, often in the fingers. Migraine sufferers frequently experience vasoconstriction (narrowing of blood vessels) in the extremities during an attack. Learning to increase peripheral blood flow (and thus hand temperature) through relaxation can help abort or reduce the severity of migraine attacks.
- Heart Rate Variability (HRV) Biofeedback: Focuses on regulating the beat-to-beat variation in heart rate, a proxy for vagal tone and autonomic balance. Improving HRV reflects a more resilient and balanced nervous system, less prone to stress-induced pain flares.
For Headaches: Biofeedback is particularly effective for both tension-type headaches and migraines. It’s often recommended as a first-line non-pharmacological treatment. Patients learn to abort developing headaches, reduce the intensity of existing ones, and decrease overall frequency by actively self-regulating their physiological responses to stress.
The Story Element: Biofeedback is about demystifying the body’s internal workings, providing a tangible pathway to self-mastery. It transforms abstract concepts like "stress" into measurable data, empowering individuals to take concrete steps toward control over their previously unconscious bodily reactions.
3. Progressive Muscle Relaxation (PMR) & Autogenic Training
The Practice:
- PMR: Developed by Edmund Jacobson, PMR involves systematically tensing and then relaxing different muscle groups throughout the body. The contrast between tension and release helps individuals become acutely aware of muscle tension and learn to release it.
- Autogenic Training: Developed by Johannes Schultz, this technique uses self-suggested phrases to induce a state of deep relaxation. Individuals mentally repeat phrases like "My arms are heavy, my legs are warm," focusing on specific bodily sensations.
The Mechanism: Both PMR and Autogenic Training directly activate the parasympathetic nervous system, inducing the "relaxation response." By consciously tensing and relaxing muscles, PMR helps individuals identify and reduce chronic muscle hypertonicity, a major contributor to tension headaches. Autogenic Training, through its focus on warmth and heaviness, influences blood flow and muscle relaxation via the ANS, promoting a systemic calm that counteracts the stress response. These practices also improve body awareness, making individuals more attuned to early signs of tension and stress.
For Headaches: These techniques are excellent for reducing the frequency and intensity of tension headaches by directly addressing muscle tension. They also contribute to overall stress reduction, improved sleep quality, and can serve as effective prophylactic measures for various headache types by lowering baseline stress levels.
The Story Element: These practices are about active participation in one’s own relaxation. They provide a tangible, step-by-step method to release the physical grip of stress, offering a profound sense of relief and control over bodily sensations.
4. Yoga and Tai Chi
The Practice: These ancient practices integrate physical postures (asanas in yoga), gentle movements (in Tai Chi), breath control (pranayama in yoga), and meditation. They are holistic systems designed to harmonize mind, body, and spirit.
The Mechanism: Yoga and Tai Chi influence the body through multiple pathways. The physical postures and movements improve flexibility, strength, and circulation, reducing muscular tension and promoting healthier blood flow. Crucially, the emphasis on conscious breathing (deep, diaphragmatic breaths) directly stimulates the vagus nerve, enhancing parasympathetic activity and reducing sympathetic arousal. The meditative aspect fosters mindfulness, improving emotional regulation and reducing the impact of stress. Regular practice can also reduce systemic inflammation, modulate pain perception, and improve sleep patterns, all of which are critical for headache management.
For Headaches: Studies support the efficacy of regular yoga and Tai Chi practice in reducing the frequency, intensity, and impact of chronic migraines and tension-type headaches. They improve patients’ ability to cope with pain, reduce medication intake, and enhance overall physical and mental well-being.
The Story Element: These practices are a journey of embodied mindfulness, a moving meditation that reconnects individuals with their physical selves in a gentle, strengthening way. They offer a path to inner peace and physical grace, transforming the relationship with one’s body from one of conflict to one of compassionate cooperation.
5. Guided Imagery and Hypnosis
The Practice:
- Guided Imagery: Involves using descriptive language and mental visualization to create vivid sensory experiences in the mind. These images can be used to promote relaxation, reduce pain, or foster healing.
- Clinical Hypnosis: A state of highly focused attention and heightened suggestibility, typically induced by a trained therapist. During this state, individuals are more receptive to suggestions that can influence perception, sensation, emotion, and behavior.
The Mechanism: Both guided imagery and hypnosis tap into the power of the subconscious mind to alter physiological responses and pain perception. The brain doesn’t always distinguish between vivid imagination and reality. By imagining a calming scene, the body can respond with relaxation. In the context of pain, these techniques can activate descending pain inhibitory pathways in the brain (e.g., through the periaqueductal gray matter), effectively "closing the gate" on pain signals before they reach conscious awareness. They can also reframe the meaning of pain, reduce anxiety about future attacks, and foster a sense of control. Suggestions can include directly reducing headache intensity, increasing comfort, or visualizing the body healing.
For Headaches: Guided imagery and hypnosis have shown significant promise in reducing the frequency and severity of various headache types, including migraines and chronic tension headaches. They can be particularly useful for individuals who experience significant anticipatory anxiety about headaches or whose pain is highly influenced by psychological factors.
The Story Element: These practices invite individuals to rewrite their internal narrative around pain, transforming a perceived threat into an experience that can be managed, altered, or even dissolved through the power of their own mind. It’s a journey into the imaginative landscape of healing, where possibilities are boundless.
6. Cognitive Behavioral Therapy (CBT) for Pain
The Practice: CBT is a structured, evidence-based psychotherapy that helps individuals identify and change maladaptive thought patterns and behaviors that contribute to or exacerbate pain. For chronic headaches, CBT focuses on teaching coping skills, challenging negative thoughts, improving sleep hygiene, and promoting healthy behavioral responses to pain.
The Mechanism: CBT operates on the principle that thoughts, feelings, and behaviors are interconnected. In the context of chronic headaches, pain can lead to negative thoughts ("This pain will never end," "I can’t cope"), which then lead to negative emotions (anxiety, depression) and maladaptive behaviors (avoidance, catastrophizing). These, in turn, can amplify the pain experience and increase stress. CBT helps individuals:
- Cognitive Restructuring: Identify and challenge irrational or unhelpful thoughts (e.g., catastrophizing about headache onset).
- Behavioral Activation: Encourage engagement in meaningful activities despite pain, reducing isolation and improving mood.
- Relaxation Training: Incorporate techniques like PMR or diaphragmatic breathing to manage acute stress.
- Pacing: Teach strategies to balance activity and rest, preventing overexertion that can trigger headaches.
- Sleep Hygiene: Address sleep disturbances, a common headache trigger and amplifier.
For Headaches: CBT is a highly effective treatment for chronic headaches, reducing pain intensity, frequency, and disability. It empowers individuals to develop a robust set of coping strategies, significantly improving their functional ability and overall quality of life.
The Story Element: CBT is about changing the story one tells oneself about pain. It’s about recognizing that while pain may be a physical sensation, the suffering associated with it is often amplified by our thoughts and reactions. It offers a practical roadmap to rewire these patterns, transforming a narrative of victimhood into one of active coping and resilience.
Weaving the Tapestry: Integration and Personalization
The true power of mind-body techniques for chronic headaches lies not in any single practice, but in their synergistic integration. The journey to "Stress Less, Ache Less" is deeply personal, often requiring experimentation and patience to discover the optimal combination of strategies.
For a knowledgeable audience, the implication is clear: a multidisciplinary approach is often most effective. This might involve:
- Medical Management: Working with neurologists or pain specialists for pharmacological interventions, trigger point injections, or advanced therapies.
- Physical Therapy: Addressing musculoskeletal imbalances, posture, and cervical issues that contribute to headaches.
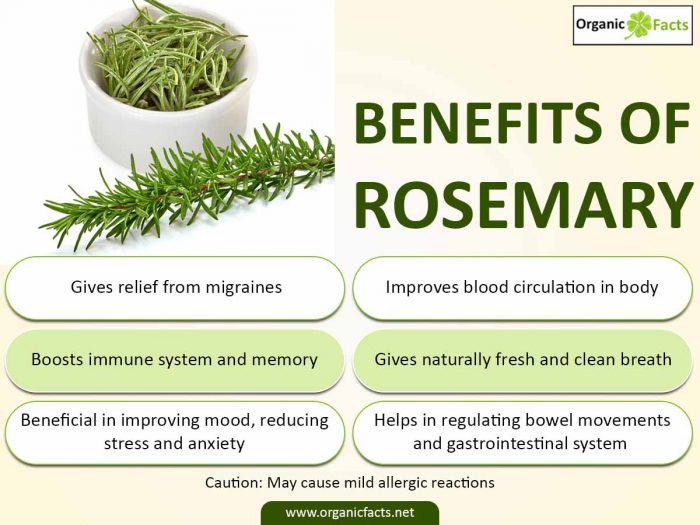
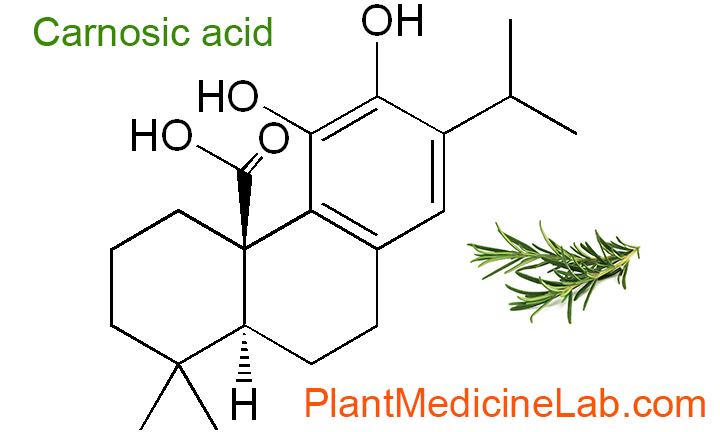
- Nutritional Support: Identifying dietary triggers and optimizing gut health.
- And crucially, Mind-Body Therapies: Integrating practices tailored to the individual’s specific headache type, stress profile, and preferences.
The "story" here is one of building a personalized healing sanctuary. One person might find profound relief through daily mindfulness meditation and thermal biofeedback, while another thrives on a combination of gentle yoga, CBT for pain, and guided imagery. Consistency is key; these are not quick fixes but rather skills that are honed over time, gradually rewiring the nervous system and fostering lasting change. Tracking headache patterns, stress levels, and the effectiveness of different techniques through a headache diary becomes an invaluable tool in this personalized journey, offering objective data to guide therapeutic choices.
The journey also underscores the importance of a strong therapeutic relationship with practitioners who understand and support an integrative approach. Healthcare professionals who can guide patients through the nuances of these techniques, interpret their progress, and offer encouragement are invaluable allies in this process.
Conclusion: Reclaiming the Narrative of Health
The narrative of chronic headache suffering has long been dominated by themes of helplessness and frustration. But with the growing understanding of the mind-body connection, and the increasing evidence supporting the efficacy of mind-body techniques, this narrative is shifting. It is transforming into a story of empowerment, resilience, and profound healing.
"Stress Less, Ache Less" is more than a catchy phrase; it’s a testament to the inherent capacity of the human system to self-regulate, to adapt, and to heal. By consciously engaging with practices like mindfulness, biofeedback, yoga, and CBT, individuals suffering from chronic headaches are not simply managing symptoms; they are actively reshaping their neural pathways, recalibrating their stress response, and fundamentally altering their relationship with pain.
This journey demands patience, commitment, and an open mind. It requires a willingness to explore the intricate landscape of one’s own internal experience and to trust in the body’s innate wisdom. But for those who embark on this path, the rewards are immeasurable: reduced pain, restored function, improved mood, and a renewed sense of agency over their health. The story concludes not with a miraculous cure, but with a sustainable, empowering approach to living a fuller, more vibrant life, free from the constant shadow of chronic pain. It is a testament to the power of the mind, in concert with the body, to rewrite the narrative of suffering into one of hope, healing, and enduring well-being.