The Trigger Tracker: How to Identify and Eliminate the Foods That Cause Your Headaches
The throbbing begins subtly, a faint pressure behind the eyes, a whisper of discomfort that quickly escalates into a roaring symphony of pain. For millions, this isn’t an occasional nuisance but a recurring nightmare – a headache that steals days, dims joy, and casts a shadow over the simplest pleasures of life. They reach for pills, retreat to dark rooms, and resign themselves to a fate they believe is beyond their control. But what if the key to unlocking freedom from this relentless torment lies not in a pharmacy, but in your pantry? What if the very sustenance designed to fuel your body is, in fact, silently sabotaging your well-being?
This is the story of the Trigger Tracker, a systematic, empowering journey designed to unmask the hidden culprits in your diet that are fueling your headaches. It’s a detective story where you are both the investigator and the subject, a journey from passive suffering to active discovery, from resignation to profound relief. For the knowledgeable individual, someone who understands the intricate dance of the human body and seeks not just symptomatic relief but root-cause resolution, the Trigger Tracker offers a rigorous, evidence-informed pathway to reclaim control over their health.
Part 1: The Invisible Enemy – Understanding Food-Related Headaches
To embark on this journey, we must first understand the nature of the enemy. Headaches are not monolithic; they manifest in various forms, each with its own physiological signature. While tension headaches, cluster headaches, and sinus headaches have distinct characteristics, our focus here will primarily be on those most commonly linked to dietary triggers: migraines and a significant subset of tension-type headaches, as well as some less common but equally debilitating types often exacerbated by systemic inflammation or specific chemical reactions.
The link between food and headaches, particularly migraines, has been recognized for centuries, yet it remains shrouded in misunderstanding. It’s not always as simple as "eat chocolate, get a headache." The connection is often delayed, dose-dependent, and highly individualized, making identification a complex puzzle.
Beyond "Just a Headache": The Physiological Pathways
For the discerning mind, understanding how food can trigger a headache is crucial. It’s not magic; it’s biochemistry. Several sophisticated physiological pathways are implicated:
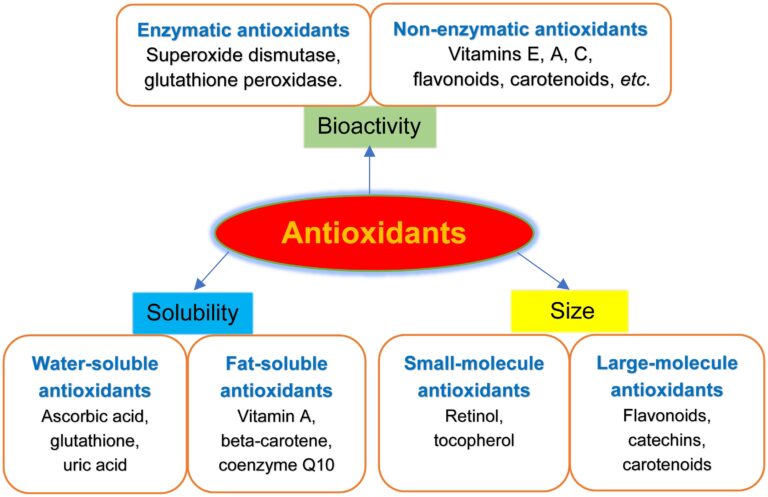
- Inflammation: Many foods, particularly processed ones, refined sugars, and certain fats (omega-6 heavy vegetable oils), can promote systemic inflammation. This low-grade, chronic inflammation can sensitize nerve endings, including those in the meninges (the membranes surrounding the brain), making them more prone to pain signals. Inflammatory mediators like prostaglandins can also directly impact blood vessel dilation and constriction, a key component of migraine pathophysiology.
- Histamine Release: Histamine, a compound involved in immune responses and neurotransmission, can be a potent headache trigger. Some foods are naturally high in histamine (fermented foods, aged cheeses, cured meats, red wine), while others can trigger the body to release its own histamine (citrus, chocolate, strawberries). Individuals with histamine intolerance lack sufficient diamine oxidase (DAO) enzyme to break down dietary histamine, leading to a buildup that can cause vasodilation, neuroinflammation, and subsequently, headaches.
- Gut-Brain Axis Disruption: The intricate bidirectional communication between the gut microbiome and the brain is a burgeoning field of research. Dysbiosis (an imbalance in gut bacteria) can lead to increased gut permeability ("leaky gut"), allowing undigested food particles and bacterial toxins to enter the bloodstream. This can trigger systemic inflammation and immune responses that directly or indirectly affect brain function and pain perception. Certain food sensitivities can also exacerbate this disruption, leading to a cascade of negative effects that manifest as neurological symptoms, including headaches.
- Vascular Changes: Migraines, in particular, are often associated with changes in cerebral blood flow. Certain food components can act as vasodilators (widening blood vessels) or vasoconstrictors (narrowing blood vessels). For instance, tyramine (found in aged cheeses, cured meats, fermented foods) can cause blood vessel constriction followed by dilation. Nitrates and nitrites (in processed meats) are potent vasodilators. Both rapid constriction and dilation can trigger headache pain.
- Neurotransmitter Imbalance: Food components can directly or indirectly influence neurotransmitter levels. For example, aspartame and MSG are excitatory neurotransmitters that can overstimulate neurons. Caffeine withdrawal can lead to adenosine receptor upregulation and subsequent vasodilation, triggering a headache. The balance of serotonin, dopamine, and other neurotransmitters, all influenced by diet, plays a critical role in pain modulation.
Why It’s So Hard to Pinpoint: The Veil of Complexity
If the links are so clear, why do so many suffer in ignorance? The answer lies in the multifaceted nature of these triggers:
- Delayed Reactions: Unlike an immediate allergic reaction, food-induced headaches often manifest hours, or even a full day, after consumption. This temporal disconnect makes it incredibly difficult to link cause and effect without meticulous tracking.
- Dose-Dependency: A small amount of a trigger food might be tolerated, while a larger portion elicits a severe reaction. This threshold effect further complicates identification.
- Cumulative Effect: Sometimes, it’s not a single food but the combination of several trigger foods, or even a trigger food consumed amidst other stressors (poor sleep, dehydration, hormonal fluctuations), that tips the scales.
- Multi-Trigger Events: Many individuals have multiple food triggers, and identifying one does not guarantee freedom from others. The elimination of one trigger might reduce headache frequency but not eliminate them entirely, leading to frustration.
- The Myth of "One Size Fits All": What triggers a headache in one person might be perfectly benign for another. Generic lists of "headache foods" are a starting point but must always be personalized.
Understanding these complexities is the first step in cultivating the patience and precision required for the Trigger Tracker.
Part 2: Embarking on the Journey – Preparing for the Trigger Tracker
The Trigger Tracker isn’t a quick fix; it’s a profound self-study. It demands commitment, self-awareness, and a methodical approach. This preparatory phase is critical for setting the stage for success.
The Mindset Shift: From Passive Suffering to Active Investigation
For years, you may have felt like a victim of your headaches. The Trigger Tracker flips this narrative. You are no longer a passive recipient of pain but an active investigator, a scientist in your own laboratory. This shift in perspective is empowering. It cultivates patience, as results won’t appear overnight. It fosters discipline, as meticulous tracking is non-negotiable. And crucially, it requires self-compassion, recognizing that this is a challenging journey with potential setbacks, but one ultimately leading to greater understanding and relief.
Consulting Your Navigator (Healthcare Professional): A Prudent First Step
Before embarking on any significant dietary change, particularly one aimed at addressing a chronic condition like headaches, consulting a qualified healthcare professional is paramount. This could be your primary care physician, a neurologist, or a registered dietitian specializing in food sensitivities. Their role is to:
- Rule out serious underlying conditions: Ensure your headaches aren’t symptoms of more urgent neurological issues.
- Provide guidance and oversight: Offer professional advice tailored to your health history, especially if you have existing medical conditions (e.g., diabetes, autoimmune diseases) or are taking medications.
- Support nutrient adequacy: Ensure your elimination diet remains nutritionally complete and safe.
- Interpret complex results: Help differentiate between food triggers and other factors.
This professional collaboration transforms the Trigger Tracker from a self-experiment into a medically informed exploration.
Essential Tools for the Expedition: The Food & Symptom Diary
This is the cornerstone of the Trigger Tracker – your most powerful investigative tool. Without meticulous record-keeping, the subtle patterns and delayed reactions will remain hidden. Think of it as your captain’s log for the journey.
What to Track, and How to Track It Effectively:
Your diary should capture as much detail as possible, transforming subjective experience into objective data points.
- Food & Drink Intake:
- Every single item: Be scrupulously honest. That single breath mint, the splash of milk in your coffee, the tiny snack – it all counts.
- Time of consumption: Crucial for identifying delayed reactions.
- Quantity: A small amount might be tolerated, a large amount might not.
- Preparation method: Fried, baked, raw? This can alter chemical compounds.
- Ingredients: Especially for processed foods. Read labels diligently.
- Headache Symptoms:
- Onset time: When did the headache begin?
- Severity (1-10 scale): Helps track improvement or worsening.
- Type of pain: Throbbing, dull, sharp, pressure.
- Location: Temples, forehead, back of head, one-sided, bilateral.
- Associated symptoms: Nausea, vomiting, light sensitivity (photophobia), sound sensitivity (phonophobia), aura, dizziness, fatigue, brain fog, mood changes, digestive issues (bloating, gas, diarrhea, constipation), skin rashes, nasal congestion, muscle aches. These "non-headache" symptoms can be vital clues to food sensitivities.
- Relief measures: What did you do? Did it help?
- Other Contributing Factors:
- Sleep: Hours slept, quality of sleep.
- Stress levels: On a scale of 1-10.
- Hydration: Water intake (crucially important!).
- Physical activity: Type and duration.
- Medications/Supplements: Any changes or regular intake.
- Hormonal cycle (for women): Menstrual phase can significantly influence headache susceptibility.
- Weather changes: Barometric pressure shifts are known triggers for some.
- Environmental exposures: Strong smells, bright lights, loud noises.
Tips for Effective Diary Keeping:
- Consistency is Key: Make it a non-negotiable daily habit.
- Digital vs. Analog: Choose what works best for you (notebook, spreadsheet, dedicated app). The most effective one is the one you will use.
- Be Specific: Instead of "sandwich," write "sourdough bread, turkey, lettuce, tomato, mustard." Instead of "coffee," specify "black coffee, 1 cup."
- Review Regularly: Look for patterns weekly. Are headaches more frequent after certain types of meals? Is there a consistent time lag?
The Baseline Period: A Crucial Pre-Elimination Phase
Before you remove any foods, spend at least 1-2 weeks meticulously tracking your typical diet and symptoms. This "baseline" period provides invaluable data, allowing you to establish your normal headache frequency, severity, and associated symptoms. It gives you a benchmark against which to measure the effectiveness of the elimination phase. Without a solid baseline, you won’t truly know if your interventions are making a difference.
Part 3: The Deep Dive – Implementing the Elimination Phase
With your preparation complete and your diary in hand, you’re ready for the core of the Trigger Tracker: the elimination phase. This is where you intentionally remove potential culprits to allow your body to reset and symptoms to subside.
The Core Principle: Elimination & Reintroduction
The scientific method dictates that to identify a cause, you must isolate variables. In the context of food triggers, this means:
- Eliminate: Remove suspected foods from your diet entirely.
- Observe: Monitor your symptoms for improvement.
- Reintroduce: Systematically add foods back, one at a time, to identify which ones provoke a reaction.
Choosing Your Path: Selective vs. Comprehensive Elimination
The intensity of your elimination phase will depend on your starting point and the severity of your headaches.
-
Selective Elimination (Targeted Approach): This is often a good starting point for those with mild to moderate headaches or those who suspect a few specific culprits. You remove the most common headache triggers first.
- Common Culprits to Consider Eliminating:
- Dairy: Lactose (sugar) and casein (protein) can be inflammatory or difficult to digest.
- Gluten: The protein found in wheat, barley, rye. Can cause inflammation, gut permeability issues, and neurological symptoms even in non-celiac individuals.
- Refined Sugar & Artificial Sweeteners: Can cause blood sugar fluctuations, inflammation, and direct neurological excitation (e.g., aspartame, sucralose).
- Caffeine: While it can temporarily relieve headaches, chronic consumption can lead to rebound headaches or withdrawal symptoms.
- Processed Foods & Additives: MSG, nitrates/nitrites (cured meats), sulfites (wine, dried fruits), artificial colors/preservatives. These can be direct neurotoxins or inflammatory agents.
- Histamine-Rich Foods: Aged cheeses, fermented foods (sauerkraut, kimchi, kombucha), red wine, cured meats, spinach, tomatoes, citrus, chocolate. Relevant for those with histamine intolerance.
- Tyramine-Rich Foods: Aged cheeses, cured meats, fermented products, some nuts, fava beans. Can trigger vascular changes.
- Chocolate: Contains caffeine, tyramine, and phenylethylamine, all potential triggers.
- Citrus Fruits: Can trigger histamine release for some.
- Nightshades: Tomatoes, potatoes, eggplants, peppers (less common for headaches, but can be inflammatory for some individuals with autoimmune conditions).
- Common Culprits to Consider Eliminating:
-
Comprehensive Elimination (The "Clean Slate"): For those with severe, chronic headaches that haven’t responded to selective elimination, a more restrictive approach might be necessary. This involves removing a wider array of potentially problematic foods, often focusing on whole, unprocessed, low-allergen options. Examples include the Autoimmune Protocol (AIP) diet or a very simple "paleo-like" elimination. This approach is highly restrictive and should ideally be undertaken with the guidance of a healthcare professional or registered dietitian to ensure nutritional adequacy and safety.
The Elimination Phase (Typically 2-4 Weeks): What to Expect and Strategies for Success
Once you’ve chosen your elimination strategy, you commit to it fully for a defined period, usually 2-4 weeks. This duration allows enough time for inflammatory processes to calm down and for your body to clear potential triggers.
-
What to Expect:
- Withdrawal Symptoms: If you’re eliminating caffeine, sugar, or highly processed foods, you might experience initial headaches, fatigue, irritability, or cravings. This is often a sign your body is detoxing and should subside within a few days to a week. Don’t give up during this phase!
- Initial Improvement: Many individuals report a significant reduction in headache frequency and intensity within the first week or two.
- Plateaus: Some may experience initial improvement followed by a plateau. This could indicate remaining triggers, other non-food factors at play, or that your body needs more time to heal.
- Frustration: It’s normal to feel limited and frustrated. Remind yourself of your ultimate goal: freedom from pain.
-
Strategies for Success During Elimination:
- Meal Planning & Preparation: This is your secret weapon. Plan your meals and snacks in advance. Cook in batches. This prevents impulsive, off-plan eating when hunger strikes.
- Read Labels Like a Detective: Assume nothing. Hidden dairy, gluten, sugar, or additives are everywhere. Look for ingredient lists on everything.
- Cook at Home: The easiest way to control ingredients is to prepare your own food. Eating out becomes challenging but not impossible if you communicate clearly with restaurant staff about your restrictions.
- Inform Your Social Circle: Explain your dietary changes to family and friends. Their understanding and support can make a huge difference.
- Manage Cravings: Have compliant alternatives readily available. Distract yourself with other activities. Remind yourself of your goals.
- Prioritize Hydration: Drink plenty of filtered water. Dehydration is a common headache trigger that can confound results.
- Focus on Nutrient Density: Emphasize whole, unprocessed foods: lean proteins, a wide variety of vegetables, healthy fats (avocado, olive oil), and some fruits. This supports overall health and helps prevent nutrient deficiencies.
Part 4: The Reintroduction Phase – Unmasking the Culprits
This is the most critical and revealing phase of the Trigger Tracker. Having cleared your system and hopefully reduced your baseline headache activity, you now systematically reintroduce foods to pinpoint the specific triggers. Think of it as a controlled experiment on your own body.
The Scientific Method Applied to Your Body: One Food at a Time, Slow and Steady
The cardinal rule of reintroduction is one food at a time, slowly. This allows you to isolate the effect of each food. If you reintroduce multiple foods simultaneously and experience a reaction, you won’t know which one was responsible.
The Reintroduction Protocol:
- Choose One Eliminated Food: Select a food you miss or suspect might be a trigger.
- Consume a Small Amount: On Day 1, eat a small portion of the chosen food (e.g., a tablespoon of yogurt, a slice of bread, a small piece of chocolate).
- Observe for 24-72 Hours: Meticulously record any symptoms in your food and symptom diary. Pay attention to all symptoms: headache, fatigue, brain fog, digestive upset, skin changes, mood shifts. Many food sensitivities have delayed reactions, so this observation window is crucial.
- Gradually Increase Amount (If No Symptoms): If no symptoms appear after the initial small exposure, try a slightly larger amount of the same food on Day 2. Continue to observe.
- Declare "Safe" (If No Symptoms): If after 2-3 days of increasing exposure (and no symptoms), the food appears to be well-tolerated, you can tentatively declare it "safe" for now and reincorporate it into your diet.
- Identify "Trigger" (If Symptoms Occur): If you experience any symptoms (especially a headache) after reintroducing a food:
- Stop consuming that food immediately.
- Allow symptoms to clear completely. This might take a few days.
- Confirm with a Second Exposure: After a symptom-free period, try a small amount of the same food again. If symptoms reappear, you have likely identified a trigger.
- Return to Elimination Diet Between Foods: After testing one food, return to your strict elimination diet for 2-3 days before introducing the next food. This ensures your body has cleared any residual effects from the previous reintroduction and that your system is reset for the next test.
Interpreting Reactions: Beyond Just Headaches
Remember, food sensitivities often manifest beyond just a headache. Be vigilant for any of the following, which could indicate a trigger:
- Neurological: Brain fog, difficulty concentrating, dizziness, irritability, anxiety, mood swings, fatigue, insomnia.
- Digestive: Bloating, gas, abdominal pain, diarrhea, constipation, heartburn, nausea.
- Skin: Rashes, hives, acne, eczema flare-ups.
- Musculoskeletal: Joint pain, muscle aches.
- Respiratory: Nasal congestion, sneezing, post-nasal drip.
These associated symptoms are powerful corroborating evidence that a particular food is problematic for your system.
The Nuance of Dose and Context:
It’s important to recognize that reactions aren’t always black and white.
- Dose-Dependence: You might find that a small amount of cheese is fine, but a large portion triggers a headache. This means you might not need to eliminate it entirely but can manage your intake.
- Cumulative Effect: A food might not trigger a headache on its own, but combined with poor sleep, high stress, or another trigger food, it could be the "straw that breaks the camel’s back." This is why your diary’s "other factors" section is so valuable.
- Context: Sometimes, the way a food is prepared or the time of day it’s eaten can influence a reaction.
Be patient, be meticulous, and trust your body’s signals. This phase is about learning your unique biological blueprint.
Part 5: Life After Identification – Crafting Your Personalized Blueprint
Having navigated the rigorous phases of elimination and reintroduction, you now possess invaluable knowledge: your personalized blueprint for headache prevention. This isn’t just about avoiding pain; it’s about understanding your body on a profound level and empowering yourself to make informed choices.
Building Your "Safe Food" List and "Trigger Food" List
At the end of your Trigger Tracker journey, you will have two distinct lists:
- Your "Safe Food" List: These are the foods you’ve successfully reintroduced without any adverse reactions. These form the foundation of your new, personalized diet.
- Your "Trigger Food" List: These are the foods that reliably provoked symptoms during reintroduction. These are the ones you’ll need to manage carefully.
Strategic Avoidance: How to Live with Triggers
Identifying triggers doesn’t mean a life of deprivation; it means a life of conscious choice.
- Complete Avoidance: For severe triggers that cause debilitating symptoms, complete avoidance is often the most sensible path. The relief from headaches far outweighs the temporary pleasure of the trigger food.
- Managed Consumption: For milder triggers, or those with a dose-dependent effect, you might be able to incorporate them sparingly. This requires self-awareness, portion control, and an understanding of your personal threshold. For example, a small amount of chocolate might be fine, but a whole bar is not.
- The "Cost-Benefit" Analysis: Before consuming a known trigger, ask yourself: Is it worth the potential headache? Sometimes, for a very special occasion, you might make a conscious choice to indulge, knowing the potential consequences and having a plan for managing them. This is an act of agency, not passive suffering.
The Power of Rotation: Preventing New Sensitivities
Once you’ve identified your triggers, it’s wise to consider a rotational diet for your safe foods. Eating the same foods day in and day out, even "safe" ones, can sometimes lead to the development of new sensitivities. By rotating your diet – eating different foods on different days – you expose your immune system to a wider variety of proteins and compounds, reducing the likelihood of developing new intolerances.
Beyond Food: Holistic Headache Management
While food is a powerful lever, it’s rarely the only factor in chronic headaches. The Trigger Tracker is one piece of a larger puzzle. To achieve optimal, sustained relief, integrate other holistic management strategies:
- Stress Reduction: Chronic stress is a potent headache trigger. Incorporate practices like mindfulness meditation, deep breathing exercises, yoga, or spending time in nature.
- Sleep Hygiene: Prioritize consistent, high-quality sleep. Create a dark, cool, quiet sleep environment. Avoid screens before bed.
- Hydration: Continue to make adequate water intake a cornerstone of your daily routine.
- Movement & Exercise: Regular, moderate physical activity can reduce headache frequency and severity, improve circulation, and manage stress.
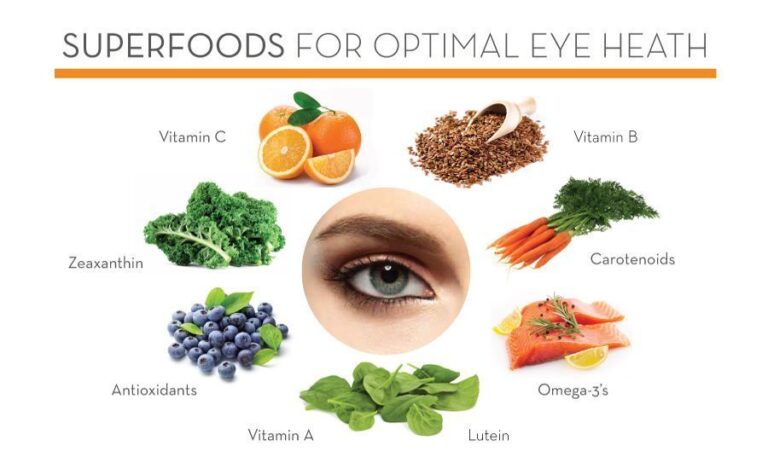
- Nutrient Deficiencies: Certain micronutrients play vital roles in neurological health and headache prevention. Discuss with your doctor or dietitian about testing for deficiencies in magnesium, riboflavin (B2), and CoQ10, and consider appropriate supplementation.
- Environmental Triggers: Be aware of other non-food triggers like strong perfumes, bright or flickering lights, loud noises, and changes in barometric pressure.
- Hormonal Influences: For women, hormonal fluctuations (menstrual cycle, perimenopause) can be significant headache drivers. Work with your healthcare provider to explore strategies for managing these.
Patience and Persistence: A Lifelong Journey
The body is dynamic. Triggers can change over time due to shifts in gut health, stress levels, or hormonal status. What was a trigger today might be tolerated in a year, and vice-versa. Therefore, periodically re-evaluating your diet and re-testing suspected triggers is a wise practice. The Trigger Tracker is not a one-time event but a philosophy of ongoing self-awareness and active health management.
Conclusion: From Shadows to Sovereignty
The journey through the Trigger Tracker is not for the faint of heart. It demands discipline, meticulousness, and an unwavering commitment to self-discovery. But for those who embark upon it, the rewards are profound. It is a story of liberation – liberation from the chains of chronic pain, from the uncertainty of unpredictable suffering, and from the passive acceptance of a debilitating condition.
You began this journey as someone battling an invisible enemy. You emerge as a knowledgeable sovereign of your own body, armed with the precise understanding of what nourishes you and what harms you. The Trigger Tracker isn’t just about identifying foods; it’s about cultivating a deeper relationship with your body, listening to its signals, and honoring its needs.
This isn’t merely about eliminating headaches; it’s about reclaiming your life. It’s about enjoying meals without fear, engaging with the world with clarity and energy, and experiencing the profound joy of a body in balance. The power was always within you, waiting to be unearthed. The Trigger Tracker simply provides the map and the compass to guide you home to a life free from the tyranny of pain. Embrace this journey, and step into the light of lasting relief and empowered well-being.