The Tug-of-War: How Fluid Loss Puts Pressure on Your Skull Nerves
Imagine a world, meticulously crafted and breathtakingly intricate, nestled within the unyielding confines of a bony fortress. This is the inner sanctum of your skull, where the brain, the universe’s most complex known object, conducts the symphony of your existence. It’s a realm of delicate balance, where every component – from the pulsating neural networks to the protective membranes and the life-sustaining fluids – plays a critical role in maintaining harmony. But what happens when this equilibrium is disrupted, when a silent, insidious battle begins to rage, pulling at the very threads of this delicate ecosystem?
This is the story of the "Tug-of-War" – a hidden struggle initiated by something as seemingly innocuous as fluid loss, yet capable of exerting profound pressure on the most vulnerable residents of our cranial cavity: the skull nerves. For the knowledgeable mind, understanding this intricate dance between hydration and neurological integrity unveils a deeper appreciation for the body’s magnificent design and its ceaseless efforts to maintain homeostasis.
Chapter 1: The Inner Sanctum – A Tour of the Cranial Landscape
Our journey begins with an exploration of the cranial landscape, a meticulously organized environment designed for protection and optimal function.
The Skull: The Unyielding Fortress
The first and most obvious feature is the skull itself – a rigid, non-expanding bony casing. Unlike a balloon that can expand and contract, the skull is a fixed volume container. This fundamental characteristic is crucial because it means that any change in the volume of its contents – the brain tissue, blood, or cerebrospinal fluid (CSF) – directly impacts the pressure within. There’s no room for negotiation; if one component decreases, another must compensate, or tension and pressure will mount.
The Brain: The Master Controller
At the heart of this fortress lies the brain, a three-pound marvel of biological engineering. It’s a soft, gelatinous organ, astonishingly delicate yet possessing an unparalleled capacity for thought, emotion, and action. Its vulnerability necessitates a robust support system, which brings us to its immediate protectors.
The Meninges: The Protective Envelopes
Enveloping the brain and spinal cord are three layers of membranes known as the meninges, providing both physical protection and a structural framework.
- Dura Mater: The outermost layer, tough and fibrous, resembling thick parchment. It adheres closely to the inner surface of the skull, forming folds that partition the cranial cavity and anchor the brain. This dura is richly innervated, meaning it’s sensitive to stretching or irritation – a key player in our story.
- Arachnoid Mater: A delicate, web-like membrane situated beneath the dura. It doesn’t follow the brain’s contours but bridges over its sulci (grooves). The space beneath it, the subarachnoid space, is a critical reservoir for cerebrospinal fluid.
- Pia Mater: The innermost layer, a thin, transparent membrane that intimately adheres to the surface of the brain, following every gyri (ridge) and sulcus. It contains a rich network of tiny blood vessels that nourish the brain.
Together, these meninges act as a multi-layered cushion and support system, suspending the brain and preventing it from directly impacting the bony skull.
Cerebrospinal Fluid (CSF): The Lifeblood of the Brain
Perhaps the most unsung hero in our cranial drama is the cerebrospinal fluid. This clear, colorless liquid, produced primarily by the choroid plexuses within the brain’s ventricles, is more than just a simple fluid; it’s a dynamic, circulating system vital for brain health.
- Buoyancy: The CSF effectively reduces the brain’s weight from about 1400 grams to a mere 50 grams, allowing it to float buoyantly within the skull. This buoyancy is critical; without it, the brain’s own weight would compress the delicate structures at its base, leading to ischemia and necrosis.
- Shock Absorption: It acts as a hydraulic cushion, protecting the brain from minor blows and sudden movements.
- Nutrient Delivery and Waste Removal: CSF facilitates the transport of nutrients to brain tissue and carries away metabolic waste products.
- Maintaining Homeostasis: It helps maintain a stable chemical environment for optimal neuronal function.
- Intracranial Pressure (ICP) Regulation: Crucially, CSF volume is a primary determinant of intracranial pressure. Its constant production (about 500 ml/day) and reabsorption (into the venous system via arachnoid granulations) maintain a delicate pressure balance.
Cranial Nerves: The Brain’s Messengers
Emerging directly from the brain and brainstem are twelve pairs of cranial nerves, each a specialized cable transmitting vital information. Unlike spinal nerves, which exit the vertebral column, cranial nerves pass through specific foramina (openings) in the skull, directly connecting the brain to various parts of the head, face, neck, and even the torso. They govern our senses (sight, smell, hearing, taste, touch), control facial expressions, eye movements, swallowing, and even regulate internal organs through the autonomic nervous system.
These nerves are incredibly delicate. As they exit the brainstem, they traverse the subarachnoid space, bathed in CSF, before piercing the dura mater and passing through their respective bony foramina. Their long, vulnerable trajectories make them susceptible to stretching, compression, or irritation, especially when the surrounding environment within the skull undergoes changes.
Chapter 2: The Onset of the Tug-of-War – When Fluid Balance Falters
With a foundational understanding of our cranial landscape, we can now introduce the antagonist in our story: fluid loss, or dehydration. This is where the tug-of-war truly begins.
Defining Fluid Loss (Dehydration)
Dehydration isn’t merely feeling thirsty; it’s a state where the body loses more fluid (and often electrolytes) than it takes in, disrupting its delicate internal balance. Causes are ubiquitous: insufficient water intake, excessive sweating (exercise, heat), vomiting, diarrhea, fever, certain medications (diuretics), and even medical conditions like diabetes insipidus. The body’s initial response involves thirst and the release of antidiuretic hormone (ADH) to conserve water, but if the deficit persists, systemic dehydration ensues.
The Brain’s Response to Dehydration: A Shrinking World
When systemic dehydration sets in, it doesn’t spare the brain. Brain tissue, like all other tissues, is composed largely of water. As the body attempts to maintain plasma volume and blood pressure, water is drawn from cells, including brain cells. This leads to a measurable reduction in brain volume.
Picture the brain, normally plump and cushioned, now slightly shrunken, like a deflated balloon within its rigid skull. This shrinkage is not insignificant; studies using MRI have shown even mild dehydration can lead to a decrease in brain volume.
Impact on CSF Volume and Dynamics
The relationship between brain volume and CSF is reciprocal. When the brain shrinks, it creates a relative increase in the space within the cranial cavity. While the body initially tries to maintain CSF volume to compensate for this lost brain mass and prevent the brain from "sagging" too much, prolonged or severe dehydration can also impact CSF production. The choroid plexuses, like other tissues, require adequate blood flow and hydration to function optimally. Reduced systemic fluid can lead to reduced CSF production, further compromising the brain’s buoyant support.
This dynamic shift creates an unsettling scenario. The brain, now slightly smaller, loses some of its essential buoyancy. It’s no longer perfectly suspended; instead, it can subtly "settle" or "sag" within the cranial vault.
The "Slosh" and "Sag" Theory
This "sagging" is a critical component of the tug-of-war. The brain, anchored by its dural folds and by bridging veins that connect its surface to the dural venous sinuses, experiences tension. Imagine a boat anchored to the seabed. If the water level drops, the anchors become taut, pulling down on the boat. Similarly, as the brain volume diminishes, the dura mater and its associated structures are subjected to increased tension.
The bridging veins, in particular, are vulnerable. These delicate vessels traverse the subarachnoid space, connecting the cerebral veins on the brain’s surface to the large dural venous sinuses (e.g., superior sagittal sinus). When the brain sags, these veins are stretched, which can cause pain and, in severe cases, even rupture (though this is rare and associated with extreme dehydration or trauma). The tension on these veins and the surrounding dura is a primary source of the headache associated with dehydration.
Chapter 3: The Pressure Mounts – The Direct Impact on Cranial Nerves
The "sagging" brain and the resulting meningeal tension are not benign. They create a cascade of effects that directly impact the cranial nerves, leading to a spectrum of neurological symptoms.
The Brain’s Descent and Meningeal Tension
As the brain shrinks and loses its buoyancy, it subtly pulls away from the inner surface of the dura mater. The dura, as mentioned, is exquisitely pain-sensitive. The stretching and tension on the dura, particularly along the falx cerebri (which separates the cerebral hemispheres) and the tentorium cerebelli (which separates the cerebrum from the cerebellum), generate pain signals. This dural tension is a major contributor to the diffuse, often throbbing, headache characteristic of dehydration.
Bridging Veins and Venous Sinuses: More Than Just Drainage
Beyond their role in anchoring, the bridging veins and dural venous sinuses are vital for cerebral venous drainage. Tension on these structures can impede the smooth outflow of venous blood from the brain. If venous outflow is even slightly compromised, it can lead to a subtle increase in cerebral venous pressure. While not true intracranial hypertension, this localized venous congestion can contribute to the feeling of pressure within the skull and further irritate surrounding pain-sensitive structures.
Direct Nerve Compression and Irritation: The Nerves in Peril
This is the heart of the "tug-of-war." As the brain shifts and the meninges become taut, the cranial nerves, particularly where they pierce the dura mater and exit the skull through rigid bony foramina, become vulnerable. They can be stretched, compressed, or irritated against these unyielding structures.
Let’s look at some specific cranial nerves and the symptoms that can arise from their irritation due to fluid loss:
- Trigeminal Nerve (V): This is arguably the most commonly affected nerve in dehydration headaches. It’s responsible for sensation in the face, mastication, and innervates large portions of the dura mater itself. Irritation of the trigeminal nerve, either directly as it exits the brainstem or via the dural branches, is a major source of the pain and pressure felt in the head and face during dehydration. Symptoms can range from a dull ache to a sharp, shooting pain, or a generalized feeling of facial pressure.
- Vestibulocochlear Nerve (VIII): Responsible for hearing and balance. When the brain sags, this nerve, as it emerges from the brainstem and enters the internal auditory meatus, can be stretched or irritated. This can manifest as dizziness, lightheadedness, vertigo (a spinning sensation), tinnitus (ringing in the ears), or even subtle balance disturbances.
- Vagus Nerve (X): A crucial nerve for autonomic functions, including heart rate, digestion, and gag reflex. While less directly compressed by brain sag, its intracranial segment can be influenced. More often, systemic dehydration’s impact on blood volume and electrolyte balance can indirectly affect vagal tone, contributing to symptoms like nausea, malaise, and altered heart rate.
- Optic Nerve (II): Responsible for vision. While direct compression is less common, dehydration can lead to subtle visual disturbances. Reduced cerebral blood flow and altered osmotic gradients can affect the optic nerve and surrounding structures, leading to blurry vision, sensitivity to light (photophobia), or even transient visual field changes.
- Oculomotor (III), Trochlear (IV), Abducens (VI) Nerves: These nerves control eye movements. Stretching or irritation of these nerves as they traverse the subarachnoid space and exit the skull can lead to eye pain, difficulty moving the eyes, double vision (diplopia), or subtle nystagmus (involuntary eye movements). The feeling of "eye strain" often associated with dehydration can stem from this.
- Olfactory Nerve (I) and Facial Nerve (VII): While less frequently cited, subtle changes in smell or taste (Olfactory, Trigeminal, Facial) or mild facial weakness/twitching (Facial) can also occur in severe dehydration due to nerve irritation or electrolyte imbalances affecting nerve function.
The "headache of dehydration" is, therefore, not simply a vague discomfort. It’s a complex neurophysiological event stemming from a combination of dural tension, stretching of pain-sensitive bridging veins, and the direct irritation or compression of cranial nerves, particularly the trigeminal nerve.
Chapter 4: Beyond the Skull – The Ripple Effect
The impact of fluid loss extends far beyond the immediate cranial nerves, creating a ripple effect throughout the entire nervous system and body.
Systemic Dehydration and its Neurological Manifestations
- Electrolyte Imbalances: Water and electrolytes (sodium, potassium, chloride) are inextricably linked. Dehydration often leads to dysregulation of these crucial ions. Sodium, in particular, is vital for nerve impulse transmission. Hyponatremia (low sodium) or hypernatremia (high sodium) can profoundly alter neuronal excitability, leading to confusion, seizures, or even coma in severe cases.
- Reduced Blood Volume and Cerebral Blood Flow (CBF): Systemic dehydration reduces overall blood volume. The body attempts to compensate by constricting peripheral vessels, but if dehydration is severe, it can lead to reduced blood pressure and, consequently, reduced cerebral blood flow. The brain is highly dependent on a constant supply of oxygen and glucose. Even a slight reduction in CBF can lead to hypoxia (oxygen deprivation) and energy deficits in brain cells, impairing their function.
- Autonomic Nervous System Dysregulation: The autonomic nervous system controls involuntary bodily functions. Dehydration can throw it off balance, leading to symptoms like orthostatic hypotension (dizziness upon standing due to a drop in blood pressure), increased heart rate, and impaired thermoregulation.
Cognitive Impairment
The brain, under the stress of dehydration, struggles to perform its higher-level functions. Brain fog, difficulty concentrating, impaired memory, slower reaction times, and reduced alertness are common complaints. These are direct consequences of reduced CBF, electrolyte shifts affecting neuronal communication, and the brain’s overall metabolic distress. Studies have shown that even mild dehydration can impair cognitive performance, particularly tasks requiring attention, motor coordination, and executive function.
Mood Disturbances
The link between hydration and mood is often overlooked. Dehydration can trigger or exacerbate feelings of irritability, anxiety, fatigue, and even mild depression. The physiological stress on the brain and the associated discomfort contribute to this psychological toll.
Exacerbation of Existing Conditions
Individuals with certain pre-existing conditions are particularly vulnerable to the neurological impact of fluid loss:
- Migraines: Dehydration is a well-known trigger for migraine attacks. The dural tension and nerve irritation described earlier can easily initiate a migraine cascade in susceptible individuals.
- Postural Orthostatic Tachycardia Syndrome (POTS): Patients with POTS often experience severe orthostatic intolerance due to autonomic dysfunction. Fluid loss can drastically worsen their symptoms, leading to extreme dizziness, rapid heart rate, and fainting.
- Fibromyalgia and Chronic Fatigue Syndrome (ME/CFS): Individuals with these conditions often report heightened sensitivity to fluid shifts and can experience significant worsening of their symptoms (pain, fatigue, brain fog) with even mild dehydration.
- Concussion/Post-Concussion Syndrome: A brain that has already suffered trauma is more susceptible to the stressors of dehydration, potentially prolonging recovery and exacerbating post-concussion symptoms.
Chapter 5: Reclaiming Balance – The Path to Relief
The story of the tug-of-war needn’t end in constant struggle. Understanding the mechanisms behind these symptoms empowers us to reclaim balance and alleviate the pressure on our delicate cranial nerves.
Prevention: The First Line of Defense
Consistent, proactive hydration is the simplest and most effective strategy.
- Adequate Intake: The "8 glasses a day" rule is a good starting point, but individual needs vary based on activity level, climate, body size, and health status. Listen to your body’s thirst signals, but don’t wait until you’re parched.
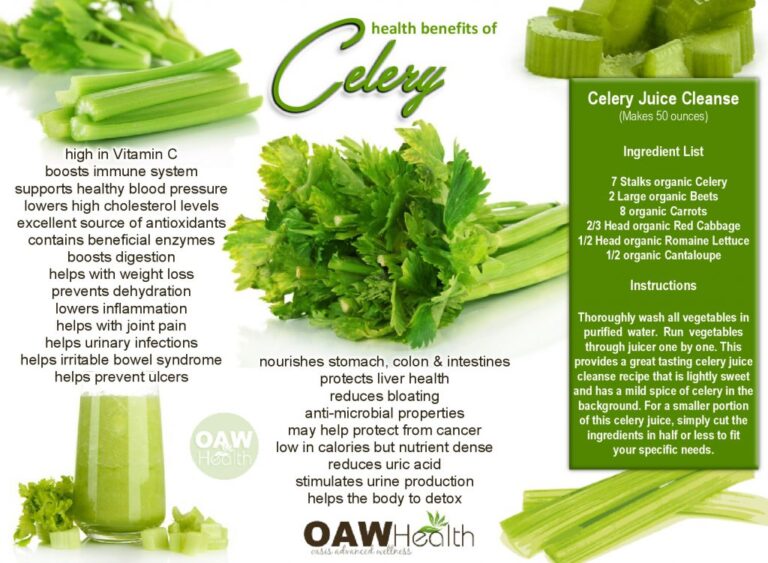
- Electrolyte-Rich Fluids: Water is essential, but during prolonged exercise, illness, or hot weather, consuming electrolyte-rich fluids (like coconut water, diluted fruit juice, or oral rehydration solutions) can be beneficial to replenish lost salts.
- Fruits and Vegetables: Many fruits and vegetables have high water content and provide natural electrolytes, contributing significantly to overall hydration.
- Monitoring Urine Color: A simple, yet effective indicator. Pale yellow urine generally signifies good hydration, while dark yellow or amber urine suggests a need for more fluids.
- Mindful Hydration: Be particularly vigilant during periods of increased fluid loss (intense exercise, illness with fever/vomiting/diarrhea), hot and humid weather, or when consuming dehydrating substances like alcohol or excessive caffeine.
Treatment for Dehydration
For acute, mild to moderate dehydration, gradual rehydration is key.
- Oral Rehydration Solutions (ORS): These solutions contain precise ratios of water, salts, and sugar, optimized for rapid absorption by the gut, effectively restoring fluid and electrolyte balance.
- Sip, Don’t Gulp: Especially if nauseated, sipping fluids slowly can prevent further stomach upset.
- Medical Intervention: Severe dehydration, characterized by extreme thirst, lethargy, confusion, or inability to keep fluids down, requires immediate medical attention, often involving intravenous (IV) fluid administration.
Long-Term Management
For those who experience chronic or recurrent symptoms related to fluid imbalance, a more comprehensive approach is needed.
- Identify Underlying Causes: Are there medical conditions contributing to dehydration (e.g., diabetes, kidney issues, autonomic dysfunction)? Is medication a factor? A thorough medical evaluation can uncover and address these.
- Lifestyle Adjustments: Consistent sleep, stress management, and a balanced diet all support overall physiological balance, including fluid regulation.
- Recognize Individual Triggers: Keep a symptom journal to identify patterns and triggers related to hydration. Understanding what exacerbates your symptoms allows for proactive intervention.
The Body’s Resilience
Despite the complexities of the cranial environment and the profound impact of fluid loss, the human body possesses remarkable resilience. When adequately supported with proper hydration and nutrition, it can restore balance, alleviate tension, and allow the cranial nerves to function optimally, silencing the insistent pressure and discomfort.
Conclusion: The End of the Tug-of-War (or the Beginning of Awareness)
The story of the tug-of-war within our skulls is a powerful reminder of the intricate interplay between seemingly simple physiological needs and profound neurological well-being. What begins as a subtle shift in fluid balance can escalate into a symphony of distressing symptoms: headaches that throb with dural tension, dizziness that signals struggling vestibular nerves, and brain fog that clouds our cognitive landscape. These are not merely inconveniences; they are distress signals from a system under pressure, a complex internal world where every drop of fluid matters.
For the knowledgeable, this journey into the cranial landscape illuminates the delicate dance of cerebrospinal fluid, the protective embrace of the meninges, and the vital pathways of the cranial nerves. It reveals how the rigid confines of the skull transform brain shrinkage into meningeal strain, bridging vein tension, and direct nerve irritation. The "pressure" felt within the head is a tangible manifestation of this physical and physiological stress.
Ultimately, the resolution of this tug-of-war lies within our grasp. By embracing consistent, mindful hydration, we provide the essential resources for our brain to float buoyantly, our meninges to remain relaxed, and our cranial nerves to transmit their vital messages unimpeded. This isn’t just about quenching thirst; it’s about safeguarding the very command center of our being, ensuring that the symphony of life within our skull plays on, clear and harmonious, free from the silent, insistent pressure of an unseen battle. Let this story be a call to action: to listen to our bodies, respect their intricate design, and provide the fundamental support necessary for optimal brain health and an unburdened mind.