The Vicious Cycle: How Dehydration Worsens Migraines and Tension Headaches
For those who grapple with the relentless grip of migraines and tension headaches, the search for triggers, remedies, and preventative measures often feels like navigating a labyrinth in the dark. We scrutinize diets, track sleep patterns, manage stress, and experiment with an array of medications. Yet, one of the most fundamental and often overlooked culprits, an insidious force capable of turning a mild ache into a debilitating assault, remains quietly at work: dehydration.
It’s not merely a lack of water; it’s a systemic imbalance that throws the delicate physiological symphony of the human body into disarray. And when it comes to the complex neurobiology of headaches, dehydration isn’t just a simple trigger – it’s a silent saboteur, weaving itself into a vicious cycle that amplifies pain, prolongs suffering, and undermines the body’s natural resilience.
This isn’t just a clinical explanation; it’s a story of the body’s intricate dance with water, a narrative revealing how a seemingly benign oversight can escalate into a profound source of distress. For our knowledgeable audience, we delve beyond the surface, exploring the profound physiological mechanisms that transform thirst into throbbing, and how understanding this cycle is the first step towards breaking free.
The Protagonists: Understanding Migraines and Tension Headaches
Before we unveil dehydration’s role, let’s briefly reacquaint ourselves with the main characters in our story of pain:
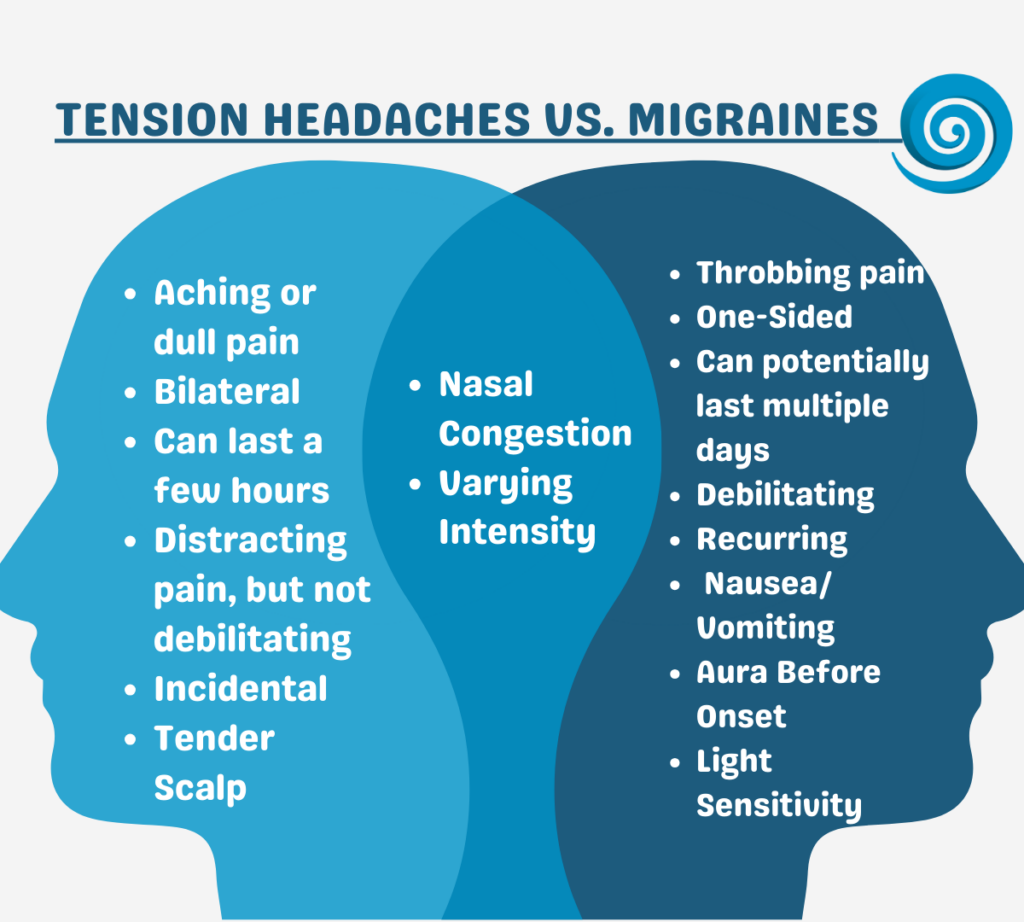
Tension Headaches: Often described as a tight band around the head, a dull ache, or pressure, tension headaches are the most common type. While traditionally linked to muscle tension in the head and neck, modern understanding acknowledges a more complex interplay of central nervous system mechanisms, including heightened pain sensitivity and neurotransmitter imbalances. They can be episodic or chronic, ranging from mildly annoying to moderately debilitating.
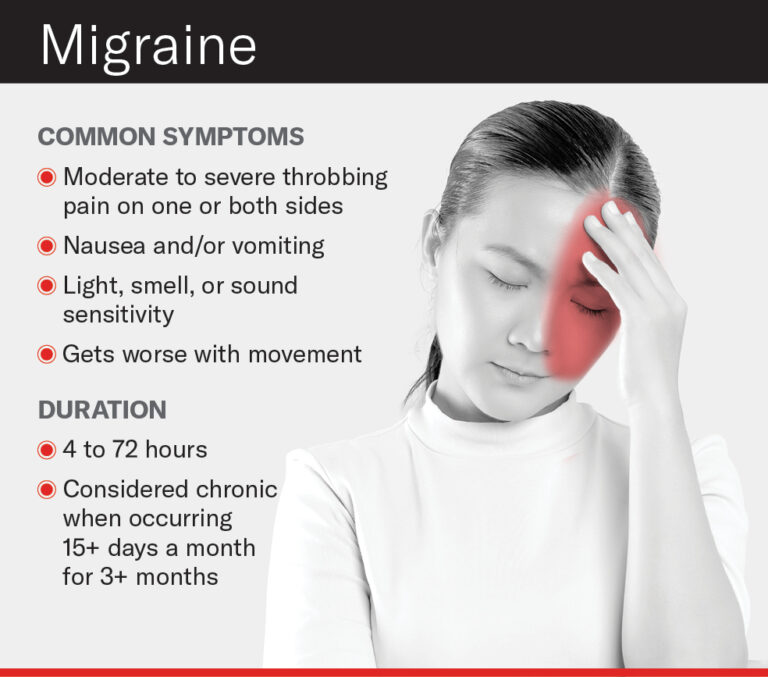
Migraines: Far more than just a severe headache, migraines are a complex neurological disorder characterized by moderate to severe throbbing pain, often on one side of the head. They are frequently accompanied by an array of debilitating symptoms such as nausea, vomiting, extreme sensitivity to light (photophobia), sound (phonophobia), and sometimes smell (osmophobia). Migraines often progress through distinct phases:
- Prodrome: Subtle warning signs hours or days before the attack (mood changes, fatigue, neck stiffness, food cravings).
- Aura: Reversible neurological symptoms occurring before or during the headache (visual disturbances like flashing lights or zigzag lines, numbness, speech difficulties).
- Attack: The headache phase, lasting from 4 to 72 hours.
- Postdrome: The "migraine hangover" phase, characterized by fatigue, confusion, and difficulty concentrating.
Both types of headaches, though distinct, share common pathways in their aggravation by dehydration, pointing to a fundamental disruption in the body’s homeostasis.
The Silent Saboteur: The Nature of Dehydration
Dehydration isn’t always the dramatic scenario of being stranded in a desert. More often, it’s a chronic, subtle state, a consequence of insufficient daily fluid intake compounded by factors like exercise, hot weather, high altitude, illness (fever, vomiting, diarrhea), excessive caffeine or alcohol consumption, and even certain medications (diuretics).
The human body is approximately 55-60% water. Every cellular process, from nutrient transport to waste elimination, depends on adequate hydration. Even a mild reduction in total body water (as little as 1-2% of body weight) can trigger a cascade of physiological responses designed to conserve fluid, but which also have far-reaching consequences, especially for the sensitive neurological system.
The Vicious Cycle Unveiled: How Dehydration Fuels Headache Pain
Now, let’s peel back the layers and explore the intricate ways dehydration becomes a central player in the headache narrative, creating a self-perpetuating cycle of pain.
1. Reduced Blood Volume and Brain Contraction: The Immediate Physical Stressor
One of the most direct impacts of dehydration is a reduction in total blood volume (hypovolemia). When the body lacks sufficient fluid, the plasma component of blood decreases. This has several critical implications for the brain:
- Brain Shrinkage: The brain, encased within the rigid skull, is highly sensitive to changes in fluid balance. A decrease in systemic hydration can cause the brain tissue itself to slightly contract or shrink away from the dura mater, the tough outer membrane that surrounds the brain and spinal cord. The dura mater is richly supplied with pain-sensitive nerve fibers. This subtle "pulling" or traction on the dura can directly trigger pain signals, initiating a headache.
- Cerebral Blood Flow Compromise: Reduced blood volume also means less blood available to adequately perfuse the brain. While the brain has robust autoregulatory mechanisms to maintain cerebral blood flow (CBF), severe or chronic dehydration can challenge these systems. A decrease in CBF can lead to mild cerebral hypoxia (reduced oxygen supply), which is a potent trigger for pain and can exacerbate neurological dysfunction, particularly in the context of migraine. The body may also respond by vasoconstriction (narrowing of blood vessels) to maintain blood pressure, further restricting blood flow to the brain and potentially causing ischemic pain.
2. Electrolyte Imbalance: Disrupting Neural Communication
Water isn’t just H2O; it’s the solvent for a crucial array of electrolytes like sodium, potassium, magnesium, and calcium. These charged particles are fundamental to nerve impulse transmission, muscle contraction, and maintaining cellular membrane potentials. Dehydration directly impacts their concentration and balance:
- Sodium (Na+): Hyponatremia (low sodium) or hypernatremia (high sodium), both possible consequences of fluid imbalance, can profoundly affect brain cell function. Sodium is critical for the firing of action potentials in neurons. Imbalances disrupt this electrical activity, leading to confusion, seizures, and headache.
- Potassium (K+): Crucial for repolarization of neurons after an action potential. Imbalances can lead to muscle weakness, fatigue, and contribute to the general malaise associated with headaches.
- Magnesium (Mg2+): A vital co-factor in over 300 enzymatic reactions, magnesium plays a key role in neurotransmitter release, nerve transmission, and muscle relaxation. Many migraine sufferers have chronic magnesium deficiencies. Dehydration can exacerbate this deficiency or impair magnesium’s absorption and utilization, leading to increased neuronal excitability, muscle tension, and potentiation of pain pathways. Magnesium also helps regulate blood vessel tone, and its deficiency can lead to cerebral vasoconstriction followed by rebound vasodilation, a pattern often implicated in migraine.
- Calcium (Ca2+): Essential for neurotransmitter release and neuronal excitability. Imbalances can disrupt normal brain function.
When these electrolytes are out of whack, the precise firing of neurons becomes erratic, contributing to the "electrical storm" characteristic of migraine aura and attack, or simply increasing general neuronal hyperexcitability that underlies tension headaches.
3. Neurotransmitter Dysregulation: The Brain’s Chemical Messengers Go Awry
The brain’s complex communication network relies on neurotransmitters, chemical messengers that transmit signals between neurons. Dehydration, through its impact on blood volume, electrolyte balance, and cellular metabolism, can significantly disrupt this delicate equilibrium:
- Serotonin (5-HT): This neurotransmitter is a major player in migraine pathophysiology. Fluctuations in serotonin levels are thought to trigger migraine attacks. Dehydration can stress the body, potentially leading to altered serotonin synthesis, release, and receptor sensitivity. A drop in serotonin can lead to vasodilation of cerebral blood vessels and activation of the trigeminal pain pathway.
- Glutamate: The primary excitatory neurotransmitter in the brain. Dehydration, especially leading to cerebral hypoxia or electrolyte imbalances, can increase glutamate release or impair its reuptake, leading to excitotoxicity – overstimulation of neurons that can cause cell damage and contribute to pain sensitization, particularly relevant in migraine.
- GABA (Gamma-Aminobutyric Acid): The main inhibitory neurotransmitter. Dehydration and electrolyte imbalances can reduce GABAergic activity, leading to less inhibition and increased neuronal excitability, making the brain more susceptible to pain signals and triggers.
- Norepinephrine (Noradrenaline): A stress hormone and neurotransmitter. Dehydration activates the stress response, leading to increased norepinephrine release, which can contribute to vasoconstriction, increased heart rate, and heightened pain perception.
4. Inflammation and Oxidative Stress: Fueling the Fire
Dehydration is a physiological stressor that can activate inflammatory pathways and increase oxidative stress, both known contributors to headache pain:
- Systemic Inflammation: When the body is dehydrated, it can trigger the release of pro-inflammatory cytokines (e.g., IL-1β, TNF-α). These chemical messengers can cross the blood-brain barrier, causing neuroinflammation. Neuroinflammation is increasingly recognized as a key component in the pathogenesis of chronic pain conditions, including migraines, by sensitizing pain pathways and exacerbating neuronal excitability.
- Oxidative Stress: Dehydration can impair the body’s antioxidant defenses, leading to an accumulation of reactive oxygen species (ROS). These free radicals can damage cellular components, including neurons and blood vessels. Oxidative stress can contribute to mitochondrial dysfunction (see below) and further fuel inflammation, creating a damaging cycle that lowers the pain threshold and makes the brain more vulnerable to headache triggers.
5. Mitochondrial Dysfunction: The Energy Crisis
Mitochondria are the powerhouses of our cells, producing ATP (adenosine triphosphate), the primary energy currency. Neurons, particularly in the brain, are highly energy-dependent. Dehydration can impair mitochondrial function through various mechanisms:
- Reduced Nutrient Delivery: Less blood flow means less oxygen and glucose reaching the mitochondria.
- Electrolyte Imbalances: Magnesium and other electrolytes are crucial for mitochondrial enzyme function.
- Oxidative Stress: Damages mitochondrial DNA and proteins.
When mitochondria aren’t functioning optimally, neurons struggle to maintain their membrane potentials, clear neurotransmitters, and manage cellular waste. This energy deficit can make neurons more vulnerable to excitotoxicity, less resilient to stress, and more prone to initiating or sustaining pain signals. Many theories of migraine involve a component of mitochondrial dysfunction, and dehydration can directly exacerbate this vulnerability.
6. The HPA Axis and Stress Response: A Symphony of Misery
Dehydration is perceived by the body as a stressor, activating the Hypothalamic-Pituitary-Adrenal (HPA) axis. This leads to the release of stress hormones like cortisol.
- Cortisol: While essential for stress response, chronically elevated cortisol levels can lower the pain threshold, increase inflammation, disrupt sleep, and deplete neurotransmitter precursors, all contributing to increased headache frequency and intensity. The headache itself is also a stressor, further activating the HPA axis, creating a feedback loop where stress, dehydration, and pain amplify one another.
7. Gut-Brain Axis Disruption: An Unexpected Link
The gut and brain are intimately connected through the gut-brain axis, a bidirectional communication system involving nerves, hormones, and the microbiome. Dehydration can affect this axis in several ways:
- Gut Motility: Dehydration slows gut motility, leading to constipation, which is a known headache trigger for some individuals.
- Microbiome Imbalance: Chronic dehydration can alter the gut microbiome composition, potentially leading to dysbiosis. A disrupted microbiome can increase gut permeability, allowing inflammatory compounds to enter the bloodstream and contribute to systemic and neuroinflammation, thereby exacerbating headache pain.
- Nutrient Absorption: Impaired gut function can lead to suboptimal absorption of essential nutrients and electrolytes, further contributing to the imbalances that trigger headaches.
8. Sleep Disruption: The Exhaustion Factor
Adequate sleep is a critical component of headache prevention. Dehydration can disrupt sleep in several ways:
- Nocturia: Drinking insufficient water during the day might lead some individuals to overcompensate by drinking large amounts closer to bedtime, leading to frequent nocturnal awakenings to urinate.
- Muscle Cramps: Dehydration and electrolyte imbalances (especially magnesium and potassium) can cause muscle cramps, including those in the legs, which can disturb sleep.
- General Discomfort: Dry mouth, thirst, and general malaise from dehydration can make falling and staying asleep difficult.
Poor sleep, regardless of its cause, is a well-established trigger for both tension headaches and migraines, further deepening the vicious cycle. An exhausted brain is a vulnerable brain, more susceptible to pain signals and less able to regulate its delicate neurochemical balance.
9. Impaired Medication Efficacy and Increased Side Effects
For many headache sufferers, medication is a lifeline. However, dehydration can subtly undermine the effectiveness of these treatments and even increase their side effects:
- Reduced Absorption and Distribution: Adequate hydration is necessary for the efficient absorption and distribution of oral medications throughout the body. Dehydration can slow gastric emptying and reduce blood flow, potentially delaying or reducing the bioavailability of headache medications.
- Exacerbated Side Effects: Many medications, particularly NSAIDs, can have gastrointestinal side effects. Dehydration can worsen these. Furthermore, some migraine-specific medications (triptans) can cause vasoconstriction; in a dehydrated state, this effect might be more pronounced or lead to other systemic issues.
- Kidney Strain: The kidneys are vital for metabolizing and eliminating medications. Dehydration puts strain on the kidneys, potentially impairing drug clearance and leading to higher concentrations of drugs in the system, increasing the risk of side effects.
Breaking the Cycle: The Path to Hydration and Relief
The good news in this story of suffering is that the antidote is remarkably simple, though often challenging to implement consistently: proactive, consistent hydration. Breaking the vicious cycle requires conscious effort and understanding.
-
Prioritize Consistent Fluid Intake:
- Listen to Your Body (and Beyond): Don’t wait until you’re thirsty. Thirst is often a sign that you’re already mildly dehydrated. Aim for regular sips throughout the day.
- The "Rule of Thumb": A general guideline is around eight 8-ounce glasses of water (about 2 liters) daily, but individual needs vary based on activity level, climate, and health conditions. Athletes, those in hot climates, or individuals with certain medical conditions may need significantly more.
- Hydrating Beverages: While water is king, herbal teas, diluted fruit juices, and broths also contribute to fluid intake. Be mindful of excessive caffeine and alcohol, which are diuretics and can worsen dehydration.
- Electrolyte Balance: For those with chronic headaches or high activity levels, consider incorporating electrolyte-rich fluids (e.g., coconut water, electrolyte-enhanced water, or homemade oral rehydration solutions) to replenish crucial minerals.
- Hydrating Foods: Fruits and vegetables (e.g., watermelon, cucumbers, oranges, berries, leafy greens) have high water content and contribute to overall hydration.
-
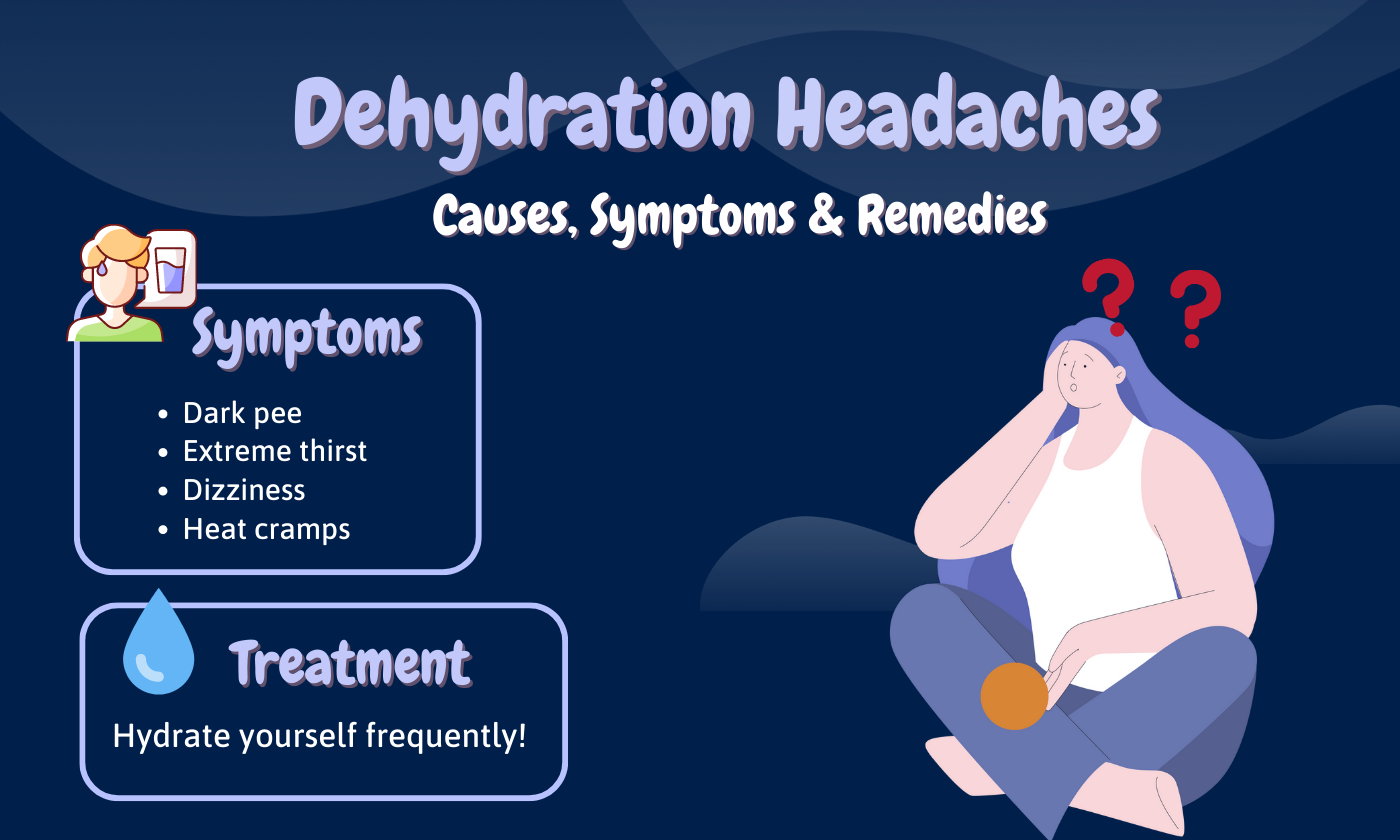
Monitor Your Hydration Status:
- Urine Color: A simple and effective indicator. Aim for pale yellow urine. Darker urine suggests dehydration.
- Regularity of Urination: Infrequent urination can be a sign of inadequate fluid intake.
-
Address Lifestyle Factors:
- Balanced Diet: A diet rich in whole foods, fruits, and vegetables provides not only water but also essential electrolytes and antioxidants.
- Adequate Sleep: Prioritize 7-9 hours of quality sleep per night. Creating a conducive sleep environment and a consistent sleep schedule can significantly reduce headache frequency.
- Stress Management: Implement stress-reduction techniques such as mindfulness, meditation, yoga, or deep breathing exercises.
- Regular Exercise: Moderate, regular physical activity can improve circulation, reduce stress, and enhance overall well-being, but remember to increase fluid intake during and after exercise.
-
Medical Consultation:
- If you experience severe or persistent headaches, or if increasing fluid intake doesn’t alleviate your symptoms, consult a healthcare professional. They can rule out other underlying conditions, provide a definitive diagnosis, and recommend appropriate treatment plans.
- Discuss your hydration habits with your doctor, especially if you are on medications that affect fluid balance (e.g., diuretics) or have conditions like diabetes or kidney disease that impact hydration.
Conclusion: The Power of Water
The story of headaches and dehydration is a compelling narrative of cause and effect, an intricate dance between the simple act of drinking water and the complex neurophysiology of pain. Dehydration is far from a trivial oversight; it is a profound physiological stressor that can initiate, exacerbate, and prolong both tension headaches and migraines through a multitude of interconnected mechanisms – from altering blood volume and brain structure to disrupting neurotransmitter balance, fueling inflammation, and compromising cellular energy.
For the knowledgeable individual seeking to regain control over their headache journey, understanding this vicious cycle is empowering. It transforms the seemingly mundane act of drinking water into a potent, proactive intervention. By consistently prioritizing hydration, we not only replenish our bodily fluids but also actively stabilize our internal environment, calm the nervous system, bolster our resilience against pain, and ultimately, begin to unravel the insidious grip of chronic headaches. The simple, often underestimated power of water stands as a testament to the body’s profound wisdom and its capacity for healing, offering a clear path towards a life less defined by pain.